2 Tincture of Time: Facial Aging and Anatomical Considerations
Summary
Genetic aging and photoaging result in thinning of all layers, effacement of the dermal-epidermal junction, loss of collagen, disorganization of elastin fibers, clumping of melanocytes, and advancing dermal elastosis. This process driven by extrinsic and intrinsic factors occurs equally across genders, male and female, however it has been published that extrinsic factors such as sun exposure and tobacco usage are more associated with male behavior. Therefore, the skin aging changes are expected to be accelerated in the male patient population sooner than in females.
The face and scalp are arranged in six concentric tissue which are thicker and heavier in men, accounting for more gravitational pull with aging and consequential tissue descend, which translates into lowering eyebrows with aging, more pronounced than in females. Furthermore, the forehead is greater in height and width, and the supraorbital rims form a more prominent ridge in men than in women. In men, temples are expected to be flat or slightly convex in contrast to their woman counterpart where temples are flat or slightly concave. The midface region in the male patient is characterized by a nose with a more straight and wider dorsum. In general, the female cheek fuller with a higher point light reflection (or projection) laterally. Men’s cheeks are usually flatter and present with a wider bizygomatic distance. On this chapter anatomic male features will be discussed as a guiding compass for surgical and non-surgical cosmetic treatment planning in the male patient.
Keywords: anatomy of aging male anatomy male and female anatomic differences male aesthetic procedures approachs to facial aging
2.1 Background
The number of aesthetic procedures performed in the United States has significantly increased over the past several decades. Between 1997 and 2016, there was a 99.2% increase in the number of cosmetic surgical procedures performed annually in the United States, and a massive 650.2% increase in nonsurgical procedures.1 In 2014, Americans spent more than $12 billion on combined surgical and nonsurgical cosmetic procedures, of which eyelid surgery, nose surgery, botulinum toxin, fillers, and chemical peels ranked among the top procedures performed. More than 40% of all cosmetic procedures were performed on individuals between the ages of 35 and 50 years. Almost 70% of adults in the United States are currently considering a cosmetic procedure.2 While 90% of cosmetic procedures are performed in females, interest among males continues to increase. Between 1997 and 2014, there was a 273% increase in the number of cosmetic procedures performed on men, with botulinum neurotoxin and dermal fillers being the most common. This compares to a 429% increase for females during the same period.
Facial aging is a multifactorial process and results in a broad range of physiologic and morphologic changes affecting every tissue system, including bones, ligaments, muscles, fascia, deep and subcutaneous fat, and skin. The process of aging is the same for everyone, although the age of onset and the rate of aging changes vary considerably between different individuals, genders, ethnic groups, and among various lifestyles. Age-related changes of the facial skeleton underlie alterations in the soft tissues that are suspended from it, and are recognized as key elements in the aging process.3,4,5,6
Men age differently than women largely because of differences in genetic and hormonal characteristics, facial anatomy, environmental exposure, and behavior. In a survey of 600 aesthetically oriented men, facial areas of primary concern were facial and forehead wrinkles, baggy eyelids, tear troughs, sagging skin, and hair loss reflecting the importance of the upper face in social interaction.7 Considering the growing number of men seeking surgical, and especially noninvasive cosmetic, procedures each year, the aesthetic provider must become comfortable with the facial anatomy of men, and the most important aspects of facial aging. Although the procedures performed in men and women are similar, anatomical details may vary, as do aesthetic objectives of men.8
2.2 Male Facial Anatomy and Aging Changes
2.2.1 Aging and Gender
Numerous soft-tissue changes gradually evolve during the aging process in the face. Both intrinsic and extrinsic factors contribute to skin aging. Smoking and ultraviolet (UV) radiation are the most important extrinsic risk factors for aging skin and for the formation of coarse wrinkles.9,10,11,12 Smoking reduces capillary blood flow, decreasing collagen and elastin fibers in the dermis and impairing elasticity. UV exposure leads to accelerated degradation of dermal collagen matrix. In general, men develop more wrinkles earlier in life than women. Although these have sometimes been attributed to higher occupational sun exposure in men, the difference remains significant even after adjusting the wrinkling for occupational sun exposure. 13 Other extrinsic factors include gravity, which acts on facial soft tissues, as well as other environmental insults, such as pollutants (e.g., heavy metals), and pesticides. Personal habits, such as diet and lack of sleep, also contribute to the onset and degree of aging changes.
Age and genetic background are the major intrinsic factors related to facial aging and the formation of fine wrinkles. Men tend to show aging phenomena more than women because of reduced innate antioxidant capacity, and increased levels of oxidative stress.14 Men are more likely to participate in behavior such as smoking, alcohol use, and UV exposure, which accelerate the aging process.15 The facial skeleton is larger in men and facial muscles have increased mass, which contribute to contraction-induced static wrinkles over time. Under the influence of these intrinsic and extrinsic factors, all of the facial skin undergoes major changes with age that progress at variable rates for each individual. Genetic aging and photoaging result in thinning of all layers, effacement of the dermal–epidermal junction, loss of collagen, disorganization of elastin fibers, clumping of melanocytes, and advancing dermal elastosis.16 This results in loss of dermal understructure with the development of ridges and wrinkles, uneven pigmentation, loss of elasticity, and stretching of small blood vessels with areas of patchy redness (Fig. 2.1).
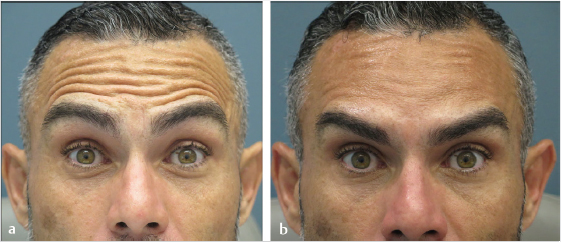
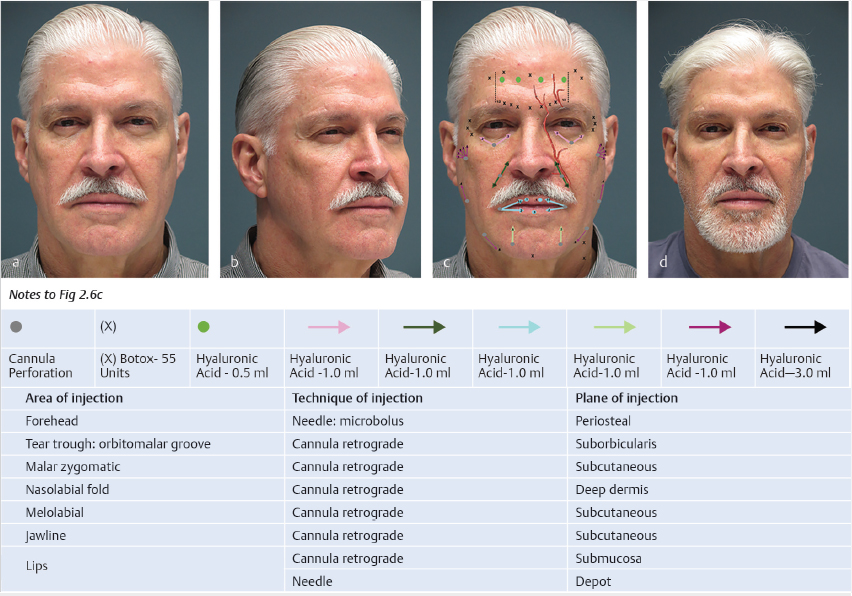
Fig. 2.1 A male patient with deep frontal ridges and wrinkles before and after neuromodulator treatment (45 units total on glabella, lateral orbicularis oculi, and frontalis muscle). (a) Before. (b) After.
2.2.2 Forehead and Temple
The face and scalp are arranged in six concentric tissue layers that consist of skin, subcutaneous tissue, superficial musculoaponeurotic layer, loose areolar tissue, deep fascia and periosteum, and bone.17 Except for thickness, the skin and subcutaneous layers are basically the same over the entire face and scalp. The musculoaponeurotic fascial layer is attached above to the skin and subcutaneous layers by fine connective tissue bands called retinacula cutis fibers. Over the scalp and forehead, the musculoaponeurotic layer is formed by the galea aponeurotica and its two muscular components, the occipitalis muscle posteriorly and frontalis muscle anteriorly. Here, the skin, subcutaneous layer, and galea form a single functional unit that is mobile over an underlying loose avascular areolar tissue layer.
These six tissue layers are thicker and heavier in men, accounting for more gravitational pull with aging and consequential tissue descend, which translates into lowering eyebrows with aging, more pronounced than in females. In the skull, however, older females have thicker bone thickness as compared to males.
The eyebrows are part of the forehead and scalp anatomy, and their mobility is part of the complex system of facial expression. They are situated over the superior bony orbital rims, at the junction between the upper eyelid and the forehead. The brows extend from just above the trochlear fossa medially, near the frontozygomatic suture line laterally. The flattened glabellar region is central in the midline and separates the two eyebrows. Above the brows, the forehead is covered by skin that becomes thinner closer to the top of the head and thicker closer to the eyebrows. The eyebrow is separated from the superior orbital rim by a prominent underlying fat pad. The skin in this region contains short, course eyebrow hairs that emerge at an oblique angle. Medially these hairs may be directed slightly upward, but they are usually directed more horizontally or slightly downward and laterally in the central and lateral brow. These variable orientations are important to consider during direct brow elevations with resection of skin immediately above the brow line, because cutting the hair follicles will result in loss of cilia and exposure of the scar line.
The eyebrow is capable of a wide range of vertical movement. These movements are accomplished by the interaction of five striated muscles that insert into the dermal tissues along the brow. These are the frontalis, procerus, depressor supercilii, corrugator supercilii, and orbicularis oculi muscles.18 All are innervated by the seventh cranial, or facial, nerve. The frontalis muscle fibers are oriented vertically on the forehead and form the anterior belly of the occipitofrontalis musculofascial complex. The galea aponeurotica covers and invests the frontalis and occipitalis muscles on either end, and carries a rich supply of blood vessels and nerves. The galea is attached to the overlying skin by a firm dense adipose layer, and is separated from the underlying cranial periosteum by a loose areolar fascial space that allows for mobility of the scalp. At 8 to 10 cm above the superior orbital rim, the galea splits into superficial and deep layers that extend anteriorly and surround the forehead muscles. The deep layer of the galea extends below the frontalis muscle and fuses to periosteum 8 to 10 mm above the superior orbital rim. The superficial layer continues downward over the anterior surface of the frontalis muscle to the orbital rim, where it inserts onto a fusion line, the arcus marginalis, around the margin of the orbital rim. From the arcus marginalis, the anterior galea continues downward into the upper eyelid, where it continues as the anterior layer of the orbital septum.
The frontalis muscle is paired and has no bony attachments. Its proximal fibers originate from the galea aponeurotica at about the level of the coronal suture line and extend toward the supraorbital rim (Fig. 2.2).
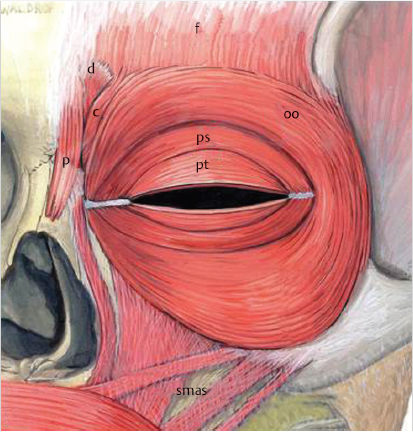
Fig. 2.2 Forehead muscles (c, corrugator; ds, depressor supercilii; f, frontalis; oo, orbicularis oculi; p, procerus; smas, musculoaponeurotic system superficial; ps, preseptal; pt, pretarsal).
Frontalis muscle fibers interdigitate with the corrugator and the orbital portion of the orbicularis muscles.19 The medial fibers blend with those of the procerus and depressor supercilii muscles. The frontalis muscle does not extend beyond the junction of the middle and lateral thirds of the brow, so that the lateral brow lacks an elevator. Because of this relationship, the lateral brow is under the depressor influence of the lateral portion of the orbicularis muscle.
Owing to the lack of frontalis action, lateral eyebrow or eyebrow tail tends to descend with aging. Neurotoxin injection on the lateral orbicularis is indicated to elevate the lateral eyebrow.
The superficial fascia over the forehead and brows is relatively thin. The skin is closely applied to the superficial layer of the galea over the frontalis muscle by fibrous septa that extend through the galea and superficial fat to the dermis. On its deep surface, the frontalis muscle is separated from the underlying periosteum by a fat layer within the deep fascia of the forehead. This has been referred to as the sub-brow fat pad or the superior retro-orbicularis oculi fat, or ROOF.20 This fat pad measures approximately 1 cm vertically and is about 5 mm in thickness, and helps cushion the brow during movement over the supraorbital bony rim. This sub-brow fat pad may get deflated with aging and is one of the target zones at the periocular area for injectable implants. The frontalis muscle elevates the brow and, together with the posterior occipitalis belly, tightens the scalp providing mobility of the skin along the temples (Fig. 2.3 and Video 2.1).
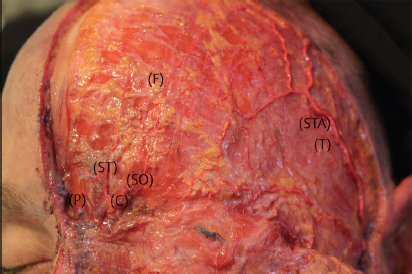
Fig. 2.3 The procerus and corrugator muscles with supraorbital and supratrochlear arteries.

Video 2.1 Roof Injection.
Forehead and brow ptosis is a prominent feature of the aging face.21,22,23 As brow ptosis progresses, dermatochalasis of the upper eyelids may become more pronounced. When a patient is evaluated for blepharoplasty, it is important to evaluate whether the dermatochalasis is the result of redundant upper eyelid skin, or a manifestation of downwardly displaced forehead skin, or both. Failure to recognize the etiology of this deformity may result in failure to correct the responsible anatomic defect (Fig. 2.4).

Fig. 2.4 An aging male face with horizontal forehead furrows, and horizontal and vertical glabellar creases.
In selected cases, neurotoxin injection, specifically at the glabellar brow depressor muscles and the lateral orbicularis, may result in eyebrow elevation that may correct a “pseudo dermatochalasis”.
Three anatomic findings that may help you predict an effective brow elevation with neurotoxin:
•Patients with thin skin on forehead/eyebrow, usually women.
•Patients with preexisting tarsal plate show.
•Patients with strong lateral orbicularis action (crow’s feet).
The procerus is a small pyramidal muscle closely related to the frontalis muscle complex. It arises by tendinous fibers from periosteum on the lower portion of the nasal bone. The muscle passes vertically upward between the brows and separates into its paired heads, which interdigitate with the medial borders of the frontalis muscle on either side and insert onto the dermis of the skin over the lower central forehead (Fig. 2.2). Contraction of the procerus muscle draws the medial portion of the brow downward and produces transverse wrinkles over the glabella and the nasal bridge. The depressor supercilii muscle was previously believed to be part of the orbicularis muscle, but it is now considered a separate structure.24 It arises from the frontal process of the maxillary bone as two distinct heads, runs superiorly deep to the lateral edge of the procerus, and inserts into the dermis of the medial brow (Fig. 2.2).
Patients with a strong nasalis muscle contraction or “bunny lines” usually have strong depressor supercilii recruitment as well. On these patients, extend your glabellar neurotoxin pattern of injections to include these muscles.
The corrugator supercilii muscle forms a pyramidal band of fibers beneath the medial fibers of the frontalis and orbicularis muscles (Fig. 2.2). It arises from the medial end of the frontal bone at the superomedial orbital rim and divides into two separate heads. The oblique head runs superiorly and slightly laterally and interdigitates through the frontalis and orbicularis muscles to insert into dermis along the medial eyebrow. This head, along with the depressor supercilii, the procerus, and the medial slip of the orbital portion of the orbicularis muscle, acts to depress the medial brow.25 The larger transverse head of the corrugator muscle passes laterally and slightly superiorly beneath the orbital portion of the orbicularis muscle within the galeal fat pad and inserts into the deep fascia of the frontalis and orbicularis muscles along the central one-third of the brow. Contraction of the corrugator muscle pulls the brow medially and downward, and produces vertical glabellar folds.
In gross shape, the forehead is greater in height and width, and the supraorbital rims form a more prominent ridge in men than in women.26 The medial supraorbital ridges in men blend into the central glabella, so that the glabellar region is more prominent than in women.27 Although the orbit is absolutely larger and more rounded in men, the male orbit is proportionally smaller in relation to the overall size of the skull.28 The eyebrow is flatter in contour and sits lower along the orbital rim.29 Men with deep-set eyes and more prominent supraorbital rim may exhibit a slightly lower brow position (Fig. 2.4).30
Stronger and bigger muscles at glabella in men required more units of neurotoxin.31 Low-set eyebrows in men required careful assessment of frontalis muscle action before neuromodulator injection to prevent potential eyebrow droopiness. In the heavy low-set male patient, consider neurotoxin injection at the glabella and the lateral orbicularis; avoid forehead injections (Fig. 2.4).
The temple refers to the anatomic area of the temporal fossa. The borders are the superior temporal line superiorly, the frontal process of the zygoma anteriorly, the zygomatic process of the temporal bone and zygoma inferiorly, and the temporal hairline and the ear posteriorly.32 The temporal fossa contains the temporalis muscle, which originates from the superior temporal fusion line and inserts inferiorly on the coronoid process of the mandible. The surface of the temporalis muscle is covered by a dense fibrous layer, the deep temporal fascia that contains a temporal fat pad inferiorly. Superficial to the deep temporal fascia is a loose areolar layer, the temporoparietal or superficial temporal fascia. The superficial temporal artery runs superiorly, and the temporal branches of the facial nerve course diagonally through this facial layer. These are important structures to be avoided in temporal forehead lift procedures and during temporal zone filler placement since it is recognized as one of the “danger zones.”
Forehead, temples, glabella eyelid, nose, mid face, nasolabial fold are facial “danger zones” because they are connected to the very complex orbital circulation. Accidental intra-arterial filler injection may produce a retrograde embolization reaching to the orbital and retinal circulation with catastrophic outcomes such as blindness33 (Fig. 2.5).
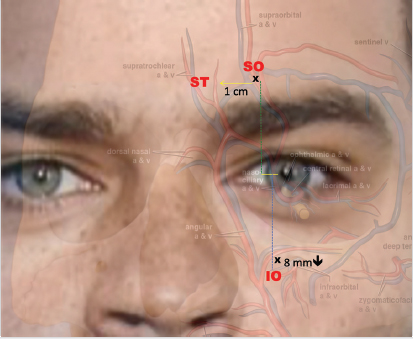
Fig. 2.5 Localization of the main periorbital vascular structures. Note: The best way to locate the main vessels around the eye is to use your patient’s pupil as your guiding compass. For instance, to find the foramen (or cleft where the bundle of supraorbital nerves and vessels emerges), use the iris’ medial limbus and the orbit’s superior margin. The neurovascular structures of the infraorbital foramen are aligned between the iris’ medial limbus and the pupil at approximately 8 mm to 1 cm from the lower orbital rim. Remember that the supratrochlear artery is located approximately 1 cm medial to the supraorbital artery. All these structures emerge from deep within these foramina.
It is well recognized that bone remodeling occurs throughout life, with a gradual additive projection of bone in the forehead by thickening of the frontal bone.34,35 The upper forehead also shows some regression due to loss of calvarial height and volume with increasing age.36 Temporal hollowing is a prominent feature of the aging face, often attributed to atrophy of the temporal fat pad. However, more recent studies suggest that redistribution of fat inferiorly rather than atrophy is more likely responsible for the relative superior hollowing in this region.37
In men, supraorbital or frontal bossing is common with an increased concavity at central forehead with aging; consider a combination of neurotoxin and filler injections in selected cases to improve the appearance of deep rhytids without lowering the “heavy” brow complex (Fig. 2.6 and Video 2.2).
Fig. 2.6 A 61-year-old patient with exemplary men’s features: low set eyebrows, frontal bossing, prominent chin, and squared jawline. (a) Before (front). (b) Before (right side). (c) Marking for injection. (d) After.

Video 2.2 Mid forehead injection in combination with neurotoxin; lip augmentation with cannula; injection jawline with cannula.
The “young” women temples are usually flat; with aging, they may become dramatically concaved. In men, temples are expected to be flat or slightly convex. For filler injection to temple, there are two schools of thought: superficial/subcutaneous injection or deep supraperiosteal injection. In our opinion, deep injection over bone is safer (Fig. 2.7 and Video 2.3).
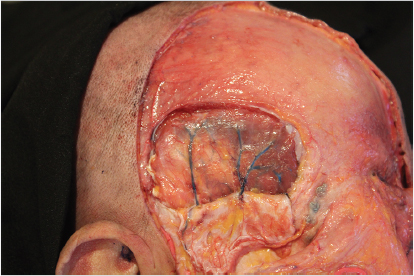
Fig. 2.7 Superficial temporal fascial.

Video 2.3 Temporal fossa injection, deep needle injection technique.
2.2.3 Eyelids and Periorbital Region
In the young adult, the interpalpebral fissure measures 10 to 11 mm in vertical height, but with advancing years the upper eyelid assumes a more ptotic position, resulting in a fissure of only about 8 to 9 mm (Fig. 2.8). The horizontal length of the fissure is 30 to 31 mm by the age of about 15 years. The upper and lower eyelids meet medially and laterally at an angle of approximately 60 degrees. The interpalpebral fissure is usually inclined slightly upward at its lateral end, such that the lateral canthal angle generally is about 2 to 3 mm higher than the medial canthal angle. In the primary position of gaze, the upper eyelid margin usually lies at the superior corneal limbus in children and 1.5 to 2.0 mm below it in the adult. The upper eyelid marginal contour usually reaches its highest point just nasal to the pupil, and the lower eyelid margin rests at the inferior corneal limbus. These anatomic landmarks are similar in both men and women.
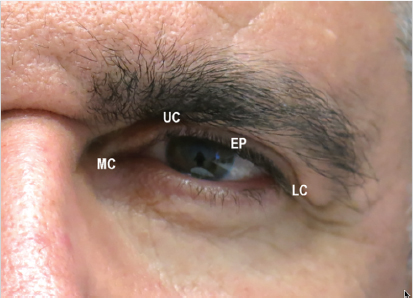
Fig. 2.8 External eyelid and the periorbital region (EP, eyelid platform; LC, lateral canthal angle; MC, medial canthal angle; UC, upper eyelid crease).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree