CHAPTER 38 Tibiotalocalcaneal and Pan-Talar Arthrodesis
TIBIOCALCANEAL AND TIBIOTALOCALCANEAL ARTHRODESIS
Fixation Alternatives
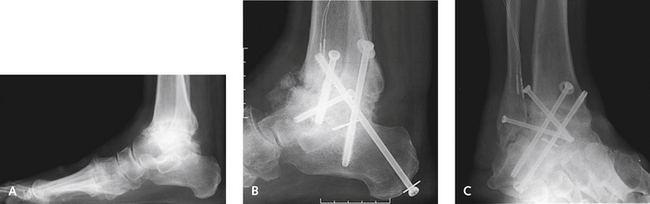
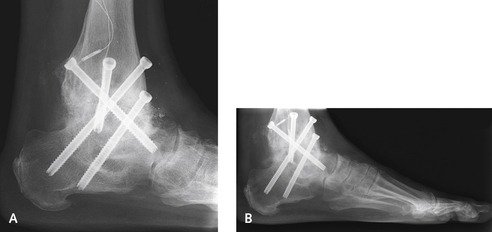
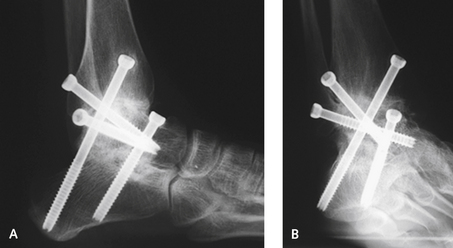
I do sometimes use screws alone for a TTC fusion, but only when the bone quality is good, the alignment of the limb is not significantly abnormal, and focal arthritis is present without bone loss or avascular necrosis (Figures 38-1 to 38-4). I rarely use screws alone when the talus is missing and the overall alignment of the limb is not satisfactory. At present, therefore, for a TTC arthrodesis, I use screws for correction of minimal deformity in ankles with good bone quality and an IM rod in a majority of the remaining cases. A blade plate remains useful when tibia deformity is present, if an IM rod cannot be used or if a simultaneous tibia osteotomy cannot be performed for realignment.
Surgical Approaches
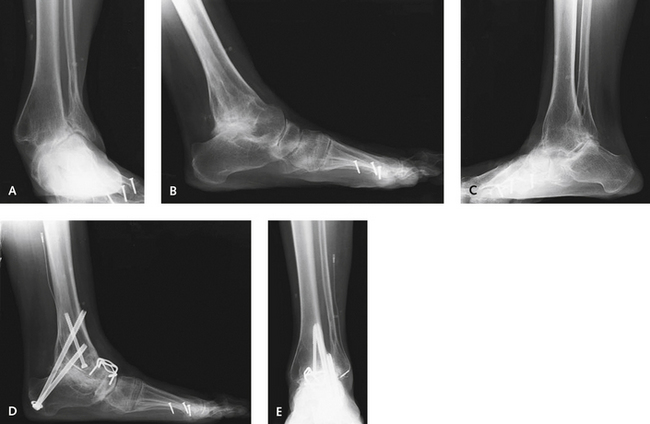
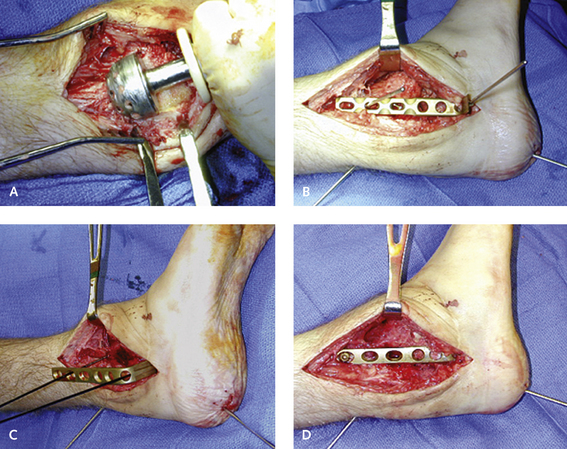
A lateral transfibular approach to the ankle and hindfoot can be used for correction of severe deformity. Although this distal fibulectomy will devascularize the lateral ankle, an alternative often is unavailable for correction of severe deformity, particularly when the ankle is angulated and in varus and the fibula is prominent. The incision is made vertically, directly over the fibula, extending down distally over the sinus tarsi toward the inferior aspect of the calcaneus. The sural nerve must be identified and then retracted inferiorly with the peroneal tendons. A fibulectomy is performed with an acetabular reamer, which is used to completely denude and decorticate the fibula. The reamings that are obtained are preserved for later use as bone graft material (Figure 38-5).
When a talectomy plus a TC arthrodesis is performed for avascular necrosis, the necrotic remnants of the talus are completely excised. A sizable defect remains; either it can be filled with bone graft or the talus can be apposed directly onto the calcaneus (Figure 38-6). Usually, despite the contouring of the posterior aspect of the calcaneus and the undersurface of the distal tibia, joint apposition cannot be easily obtained. It is difficult to appose the calcaneus flush up against the tibia, because the hindfoot tilts up into dorsiflexion, leaving the hindfoot in a calcaneus position. A defect of variable size, depending on bone erosion, is always present between the undersurface of the tibia and the dorsal surface of the posterior facet; the shape of the defect may range from a trapezoid to a large triangle (Figure 38-7). At times, if the apposition between the tibia and the calcaneus is very good and the defect is not too large, it can be filled with cancellous graft only. Some bone graft is needed in the more anterior aspect of the arthrodesis to fill the defect properly. Here either cancellous graft or a tricortical structural allograft can be used; the choice will depend on the availability of large structural graft and the size of the defect. It is clearly easier to secure the posterior tibia to the dorsal calcaneus and then fill the defect with cancellous graft. Over the past several years, with the increased use of orthobiologic adjuvants, the latter has been my preferred technique (Figure 38-8). I use a structural graft when the height of the limb must be restored. In some circumstances, this structural graft has to be used between the tibia and the calcaneus. Of note, in performing a talectomy and TC arthrodesis, as the heel is pushed up against the tibia, the skin on either side of the ankle gets compressed, and closure can no longer be achieved without tension on the skin (the so-called accordion effect—as the structure is elongated, it narrows, and as it is compressed, it widens).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree