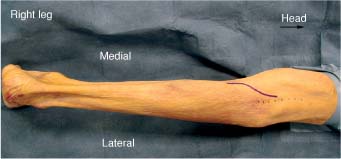
13 The tibial nerve continues the line of the sciatic nerve after its bifurcation in the middle to distal third of the thigh. Its fibers are derived from the ventral divisions of the ventral rami of the fourth and fifth lumbar nerves and the first, second, and third sacral nerves. At its origin the nerve is overlapped by the margins of the semimembranosus and biceps femoris muscles. In the popliteal fossa the tibial nerve becomes more superficial, first lying posterior and lateral to the popliteal vessels and then crossing obliquely to their medial side before moving into the leg. In the leg it lies beneath the heads of the gastrocnemius and plantaris. Lying superficial to the popliteus and under the tendinous arch of the soleus the nerve travels distally in the leg between the gastrocnemius and the tibialis posterior muscles. As the nerve courses through the popliteal fossa it may give off sensory branches to the proximal calf as well as branches to the gastrocnemius, soleus, plantaris, popliteus, and tibialis posterior muscles. Distally the tibial nerve lies between the flexor digitorum longus and flexor hallucis longus muscles. In the distal third of the leg the nerve is covered only by skin and fascia as it descends toward the ankle region. Finally the nerve curves anteroinferiorly into the sole of the foot behind the medial malleolus, deep to the flexor retinaculum and between the tendons of the flexor hallucis longus and the flexor digitorum longus. This is the so-called tarsal tunnel. The tarsal tunnel may be divided into a proximal portion, which extends from the flexor retinaculum to the origin of the abductor hallucis muscle, and a distal portion, which begins at the fibrous origin of the abductor muscle and extends through the belly of the muscle. The nerve runs with the tendons of the tibialis posterior, the flexor digitorum longus, and the flexor hallucis longus muscles (the mnemonic “Tom, Dick, and Harry” can be useful in remembering the tendinous structures that course through the tarsal tunnel). Also accompanying the tendons and nerve are the posterior tibial artery and veins. The tibial nerve usually divides into medial and lateral plantar nerves ~1 cm proximal to the fibrous leash of the abductor hallucis muscle. The nerve ends at this level as it divides into medial and lateral plantar nerves. A calcaneal branch is given off just proximal to the tarsal tunnel. The lateral plantar nerve runs deep in the instep and supplies foot intrinsic muscles and sensation on a portion of the sole of the foot and the fourth and fifth toes. The medial plantar nerve supplies sensation to the central portion of the sole of the foot and the first three and one half toes. The sural nerve, a cutaneous branch of the tibial nerve, arises at the middle or lower aspect of the popliteal fossa. It descends in the leg, with or without a contribution from the peroneal nerve between the two heads of the gastrocnemius muscle. The nerve pierces the deep fascia and gives off a small medial sural cutaneous nerve. Just after this it is joined by a communicating branch from the lateral sural cutaneous nerve in ~75% of patients.1 As it continues down the leg it pierces the fascia ~16 cm proximal to the lateral malleolus and then continues to move distally in an oblique direction toward a more lateral position on the posterior aspect of the leg. It gives off branches to the skin on the lower lateral leg and heel. The terminal portion of the sural nerve is the lateral dorsal cutaneous nerve that supplies sensation to the lateral foot and small toe. The tibial nerve at the level of the popliteal fossa is explored in the prone position. After intubation and induction of general endotracheal anesthesia, usually on a stretcher, the patient is placed on the operating table on bolsters, allowing the abdomen to hang freely. The arms may be either tucked to the side or brought forward on arm boards. The midline of the popliteal fossa and leg just superior to it should be marked. The incision begins at the midline of the leg and extends distally to run obliquely in a medial direction across the popliteal fossa. It continues down the leg just medial to the midline (Fig. 13-1). This type of incision avoids a direct cut across the popliteal fossa and avoids scar tissue that can cause a knee flexion contracture. The skin is infiltrated with a 1% lidocaine with 1:100,000 epinephrine solution. The skin and subcutaneous tissue are divided, and the fat plane that the nerve travels in is faintly visible (Fig. 13-2). The fascia overlying this fat is divided and the plane between the two heads of the gastrocnemius muscle is developed (Fig. 13-3). The tibial nerve is located in the midline, just deep to this fat pad and in close approximation to the popliteal artery and vein (Figs. 13-4 and 13-5). Care must be taken to preserve these important vascular structures. The artery should not be skeletonized unless there has been, or is a need for, vascular repair of the vessel. If extensive scarring is present, it may make the popliteal vessels difficult to find and therefore vulnerable to injury. A vascular surgeon should be on standby if the operator is not familiar with vascular repair. The small saphenous vein also runs close by the tibial nerve and should be preserved (Fig. 13-6). The tibial nerve may then be dissected out into its various distal branches (Fig. 13-7). If difficulty is encountered locating the tibial nerve due to injury or distorted anatomy, the incision should be extended proximally in the midline onto the thigh to normal or unscarred tissue. The sciatic nerve can be located in the midline of the thigh and may then be traced along to its bifurcation, thereby locating the tibial nerve (Fig. 13-8).
TIBIAL NERVE
ANATOMY
POSITIONING AND SURGICAL EXPOSURE
In Thigh
Tibial Nerve
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








