Photodynamic therapy with ALA or MAL is an excellent treatment for multiple actinic keratoses
Large field photodynamic therapy can eradicate multiple actinic keratoses with a shorter downtime than 5-fluorouracil or imiquimod
Multiple large field photodynamic therapy sessions can delay the appearance of actinic keratoses
Photodynamic therapy with MAL is approved in several countries for the treatment of superficial basal cell carcinoma and Bowen’s disease
Photodynamic therapy with ALA or MAL has been successfully used off-label for the treatment of acne vulgaris and to improve photoaging.
Intense pulsed light and pulsed dye lasers can be used to activate porphyrins after ALA or MAL application
Introduction
Photodynamic therapy was officially discovered at the turn of the twentieth century The use of photodynamic therapy with ALA to treat actinic keratoses and basal cell carcinoma was pioneered in Canada by Kennedy and Pottier Both ALA and MAL are transformed into porphyrins which can be activated by blue or red light |
Photodynamic therapy (PDT) combines the administration of a photosensitizer or photosensitizer precursor with its activation by light of the appropriate wavelengths. In the presence of oxygen, this leads to generation of reactive oxygen species and free radicals. Treatment with plants containing photosensitizers followed by sunlight exposure was practiced by several civilizations since antiquity, but PDT was officially discovered at the turn of the twentieth century by Oscar Raab, a medical study working in Germany in the laboratory of Von Tappeiner.1 The discovery that pre-malignant and malignant skin lesions can be treated with topical aminolevulinic acid (ALA) application followed by light exposure was made in Canada by Kennedy and Pottier in the late 1980s.2
Aminolevulinic acid (ALA) can enter the heme biosynthetic pathway which leads to production of porphyrins and ultimately of heme, as protoporphyrin IX is transformed into heme by the enzyme ferrochelatase. Heme has a negative feedback on ALA synthesis. The addition of exogenous ALA bypasses this negative feedback leading to accumulation of porphyrins which can be activated with visible light (Fig. 1). Blue light is the most efficient waveband for porphyrin activation but red light is also often used as it penetrates deeper than blue light. Following this discovery, researchers experimented with several ALA derivatives including methylaminolevulinate (MAL)3. This ester of ALA also enters the heme biosynthetic pathway where it is transformed into porphyrins.
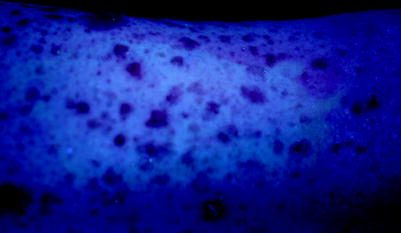
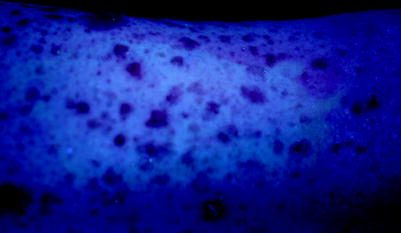
Fig. 1
Accumulation of porphyrins (pink-red) in basal cell carcinomas of a patient with Gorlin’s syndrome 3 h after application of ALA. Photograph taken under Wood’s lamp
With the approval of ALA and MAL in several countries, photodynamic therapy is now a well established procedure in Dermatology. Both drugs are approved to treat actinic keratoses (AK). In addition, MAL is approved in several countries, but not in the US, for the treatment of various types of non-melanoma skin cancers. Since the approval of MAL and ALA, physicians have successfully used these two photosensitizer precursors for the treatment of several other skin diseases and have combined them with different lasers, intense pulsed light and other non-coherent light sources for porphyrin activation.
Indications and Contraindications
Indications |
Aminolevulinic acid: minimally to moderately thick actinic keratoses of the face and scalp |
Methylaminolevulinate: non hypertrophic actinic keratoses of the face and scalp |
PDT with MAL is approved in several countries, but not in the US, for the treatment of superficial basal cell carcinoma and Bowen’s disease |
Contraindications |
Porphyria and sensitivity to visible light |
Presence of invasive squamous cell carcinoma in the treatment field |
Morpheiform basal cell carcinoma |
Topical or systemic medications inducing visible light sensitivity |
Allergy to MAL |
Warning: MAL contains peanut oil |
Indications
Aminolevulinic acid is approved in the US, Canada and Brazil for the treatment of minimally to moderately thick actinic keratosis of the face and scalp in combination with the Blu-U unit (Fig. 2). The original approval was for non-hypertrophic actinic keratoses. This has recently been changed to minimally to moderately thick AK at the FDA’s request. In practice, this wording is similar and refers to the fact that PDT is not approved for thick and hypertrophic AKs. There are two issues related to treatment of hypertrophic AKs with PDT. The first is inadequate penetration of ALA through the hyperkeratotic portion of the lesion and the second is the possibility that some of the more hypertrophic lesions might be micro-invasive SCCs. The current approval is based on phase III studies where ALA was applied on visible lesions for 14–18 h followed by 10 J/cm2 of blue light from a Blu-U unit.4 However, in practice very few physicians use ALA-PDT with a 14–18 h incubation. Most will use a shorter incubation of 45 min to 2 h. This off label use is supported by a small pilot study which showed that incubation of 1–3 h in patients with extensive sun exposure leads to AK lesion cure rates that are similar to what has been reported with longer incubations in phase III studies.5 Complete responses on BCC have been reported following ALA-PDT,6 however the efficacy of ALA-PDT for the treatment of BCC has never been studied in multicenter phase III trials and the long term recurrence rates have not been well studied.


Fig. 2
Blu-U device. This non-coherent light source is approved for the treatment of actinic keratoses with ALA
MAL is currently FDA-approved for the treatment of non hypertrophic actinic keratoses of the face and scalp in immunocompetent patients when used in conjunction with lesion preparation and when other therapies are considered medically less appropriate. AK cure rates following either a single MAL-PDT session repeated at 3 months if necessary or 2 MAL-PDT sessions performed 7 days apart have been reported to be around 90%.7 ’ 8 Studies presented at meetings suggest that multiple large surface ALA or MAL PDT sessions can delay the appearance of new actinic keratoses in organ transplant patients. This suggests that large surface PDT may be able to prevent skin cancer.
Several countries have also granted approval of MAL-PDT for the treatment of various non-melanoma skin cancers. The indications vary from one country to another but in general most countries approved MAL-PDT for the treatment of Bowen’s disease and superficial BCC when other therapies such as surgery are considered inappropriate.9–11 The complete response rate of superficial BCC following MAL-PDT has been shown to be 97% and the 48-month long-term recurrence rate 22%.12 ’ 13 The main advantage of PDT for the treatment of sBCC and Bowen’s disease is the excellent cosmetic outcome as compared to surgery, cryotherapy or electrodessication and curettage.6 ’ 9 Some countries have also approved MAL-PDT for thin nodular BCC, but because the cure rate is lower than with sBCC many countries have restricted their approval to sBCC. Recurrences for superficial BCCs, nodular BCCs and Bowen’s disease usually occur during the first 2–3 years after therapy with no increase in recurrence between the third and the fifth year.
At the time this text was written, MAL was not yet commercially available in the US because the FDA approved MAL only in combination with the Curelight device, an earlier LED light source that is rather cumbersome. In most countries MAL is approved with the Aktilite (Fig. 3), a smaller and more convenient device. Studies comparing the efficacy of Curelight and Aktilite in the treatment of AK are currently being completed in the US. These studies should lead to FDA approval of MAL-PDT performed with the Aktilite device.


Fig. 3
Aktilite device. This LED light source is approved in several countries for the treatment of AK and/or Bowen’s disease and/or superficial basal cell carcinoma with MAL
Initial studies conducted with PDT for skin diseases often used lasers. However, the current off-label trend with ALA-PDT is to use broad area application ALA or MAL in order to treat non-visible lesions, improve photoaging and eventually prevent the appearance of new lesions. This trend combined with the cost and limited availability of lasers in the 400–450 nm and 630–640 nm ranges has limited the use of lasers for PDT in Dermatology. When physicians are using ALA with a non-approved light source, they tend to favor LEDs or intense pulsed light. However, the pulsed dye laser at 595 nm has also been used for the treatment of actinic keratoses and acne.14
ALA and MAL have been reported to successfully treat various non oncologic skin conditions in small pilot studies or in single case reports. These include acne, sebaceous hyperplasia, hidradenitis suppurativa and photoaging.14–19 MAL and ALA are both in phase II for the treatment of acne. A number of small controlled studies have shown that MAL and ALA can improve acne.14 ’ 15 ’ 20 ’ 21 This is related in part to the intense accumulation of porphyrin in sebaceous glands following topical application of ALA and MAL (Fig. 4). Light exposure could induce partial necrosis of sebaceous glands and reduce sebum excretion thus reducing acne lesions. Preliminary findings with ALA suggest that this is one of the mechanisms of ALA-PDT when used for the treatment of acne.22 Studies performed with PDT in acne are complicated by the fact that blue or red light alone can improve acne by elimination of propionibacterium acnes as these bacteria naturally accumulate porphyrins.23 The best treatment parameters for acne are currently unknown. Most controlled studies which have shown good efficacy report a strong post PDT phototoxic reaction. Clinical photographs published in some of the articles which used MAL under occlusion for 3 h show moderate to severe erythema with crusting 1 day post-PDT. These publications report severe pain in many patients during light exposure.15 ’ 21 Such a strong phototoxic reaction is probably not needed to see improvement in acne. However, it is possible that prolonged remission requires a certain degree of phototoxic reaction as necrosis of sebaceous gland tissue might be necessary. The current literature suggests that PDT for acne is more efficacious for patients with moderate to severe inflammatory acne.
Fig. 4
(a) Porphyrin fluorescence in sebaceous glands 3 h after application of MAL. (b) Same section stained with hematoxylin
Touma and colleagues have demonstrated that the use of ALA-PDT with a 1–3 h incubation followed by blue light exposure in patients with multiple actinic keratoses can improve photoaging.5 Small wrinkles, pigmentation and sallowness were the parameters best improved with ALA-PDT. ALA-PDT performed with IPL has also been shown to improve photoaging.18 ’ 24 Small studies have also shown complete response in AKs treated with ALA and IPL.24 ’ 25 There are currently a very wide variety of devices approved and used for the treatment of photoaging. Most physicians using ALA or MAL-PDT for photoaging either combine PDT with other devices and treatments or favor ALA or MAL-PDT for patients with actinic keratoses who would also like to have improvement in photoaging.
Contraindications
ALA and MAL are contraindicated in patients sensitive to visible light corresponding to the spectral output of the light source used (400–450 nm for Blu-U and 630–640 nm for Aktilite). Patients with porphyria and some patients with solar urticaria are also sensitive to visible light. ALA and MAL-PDT performed on patients using concomitant photosensitizing drugs such as phenothiazines, tetracyclines, thiazides and sulphonamide have not been thoroughly studied and could theoretically increase the phototoxic reaction seen after PDT. Current use of topical or systemic retinoids such as tretinoin, adapalene, acitretin or isotretinoin could also increase the phototoxic reaction. MAL contains peanut oil. It should not contain the protein allergen present in peanuts, but many physicians refrain from using MAL-PDT in patients allergic to peanuts.
Histological variants of BCCs that are at high risk of recurrence such as morpheiform BCC are a contraindication to PDT with MAL. Pigmented basal cell carcinoma is usually considered a contraindication to PDT as pigment limits light penetration. However several physicians have reported complete responses of pigmented BCCs with PDT.
Techniques
Pre-operative management Informed consent with emphasis on difficulty to predict phototoxic response Thorough examination of skin areas to be exposed to detect malignant lesions Consider herpes simplex prophylaxis Description of the technique Skin preparation to enhance penetration (mandatory for MAL) Photosensitizer application Interval to allow porphyrin build-up Light exposure Post operative management Sun avoidance Ferrous oxide containing sunscreen Moisturizer |
Pre-operative Management
A complete skin examination of the areas to be treated is necessary. This is of the utmost importance when performing large surface PDT. This examination should focus on the identification of malignancies such as basal cell carcinoma, squamous cell carcinoma and melanoma. Sub-optimal treatment of these malignant lesions could lead to later, deeper recurrences. Any suspicious lesion should be biopsied. If PDT is performed to treat a malignant lesion such as BCC or Bowen’s disease, a pre-treatment biopsy is recommended. A complete medical history including the existence of visible light sensitivity diseases such as porphyria or solar urticaria should be recorded. Patients should be asked about current use of any topical product on the areas to be treated. Products that can alter the stratum corneum such as topical retinoids can increase ALA and MAL penetration and create a more severe phototoxic reaction following PDT. The use of systemic treatments that increase visible light sensitivity such as St-John’s wort should be avoided.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree