(1)
Obesity Institute, Geisinger Medical Center, Southold, NY, USA
Abstract
Therapeutic endoscopy refers to the new emerging field of endoscopic interventions for weight loss. The field is in its infancy, but interest seems to be driven by the awareness that weight control for most is a life-long struggle and that bariatric surgery is not curative for extreme obesity. The failure of conventional weight loss treatments has stimulated interest in a treatment strategy for obesity, which may involve a series of low-risk less-invasive interventions with modest weight loss expectations as a compliment to, or possible alternative to bariatric surgery. Endoscopic interventions with the capability of full thickness endoscopic suturing are being used both as an adjunct to bariatric surgery in the management of pouch and stomal dilatation, and as primary interventions for weight loss. In addition, newly designed gastric balloons are being investigated with promising results in regard to weight loss and resolution of comorbid conditions. This chapter reviews the published outcomes of endoscopic interventions for weight control.
Endoscopic Procedures for Weight Loss
Endoscopic interventions to promote weight loss began 25 years ago with the introduction of the initial intragastric balloon. Although the field remains in its infancy, the technology is now rapidly expanding, perhaps driven by the huge impact of bariatric surgery on health afflictions related to obesity. This technology has the potential to provide low-risk intervention options which can be used for preoperative weight loss in high risk candidates for bariatric surgery, ambulatory repetitive treatments to address problems with weight maintenance following bariatric surgery, and low-risk primary procedures for obesity treatment. The increased interest in endoscopic interventions is driven by the major unsolved issues in bariatric surgery today, which include the proper management of the postoperative patient who struggles with weight maintenance and weight regain as well as patient access to bariatric surgery [1–4].
Many of these endoluminal technologies remain investigational at present and outcomes must be carefully scrutinized in regard to safety, efficacy, and durability of results. Additional challenges to implementation include the need for advanced endoscopic skills and equipment with implications regarding cost, training, learning curve, and patient risk. A recent survey of bariatric surgeons concerning expectations for endoluminal therapy suggests that more modest weight loss outcomes are acceptable as these procedures are low risk in comparison to surgical revision [3]. For these new interventions, clearly defined benchmarks for efficacy in balance with risks are needed for thorough evaluation of each technology [3, 4].
Endoscopic Procedures to Restore Pouch and Stoma Size After Bariatric Surgery
Weight maintenance and weight regain are major concerns after foregut bariatric surgery procedures. This is often a progressive problem in later follow-up and is frequently associated with some recurrence of the obesity disease burden [5, 6]. Bariatric surgeons have observed that the early and prolonged satiety, which occurs after the gastric bypass and restrictive procedures, does diminish somewhat in association with enlargement of pouch and stoma. This loss of prolonged satiety causes earlier return of hunger, which may be accentuated by reactive hypoglycemia. The frequent result is increased frequency of small meals and weight regain. Foregut workup in many of these patients does reveal some enlargement of gastric pouch and gastrojejunal stoma.
The exact cause of weight regain after gastric bypass and other procedures is unknown and is probably multifactorial. Several studies have demonstrated that preservation of a small gastric pouch and stoma is associated with better 1–2 year weight loss, and that pouch and stoma enlargement correlates negatively with 1–2 year weight loss [7, 8]. Other studies examining pouch and stoma size after gastric bypass demonstrate an association between weight regain and pouch and stoma size [9, 10]. These are all retrospective observational studies, which do not confirm causality, but they have led bariatric surgeons to offer surgical revision in order to restore the early and prolonged satiety in order to better manage weight regain and maintenance. A major need in bariatric surgery is prospective trials aimed at identifying patient and anatomical factors which influence weight loss and weight maintenance.
Endoscopic Sclerotherapy
Endoscopic sclerotherapy of the enlarged gastrojejunostomy stoma (Fig. 11.1a) is a procedure designed to reintroduce early satiety by the endoscopic injection of a sclerosing solution (sodium morrhuate) circumferentially into the tissue around the anastomosis and reduce stoma size (Fig. 11.1b, c) [11]. This procedure was first reported in 2003 [12], and has been reported in a number of small case series with the injection of 6–13 ml of sclerosing solution per patient [13–15]. The procedure does appear to reintroduce early satiety, and results in improvement in weight trends in the majority, especially after multiple treatments [13–15]. Reported weight loss is modest, and only short-term results with up to 1-year follow-up in small numbers of patients have been reported. The poor track record of gastric restriction procedures for obesity would suggest that this technique, when used repeatedly, may have a role in weight maintenance after gastric bypass, but should be combined with other aggressive efforts to change lifestyle and behavior. The evidence to date suggests that this procedure is unlikely to be the definitive solution for gastric bypass weight maintenance struggles.
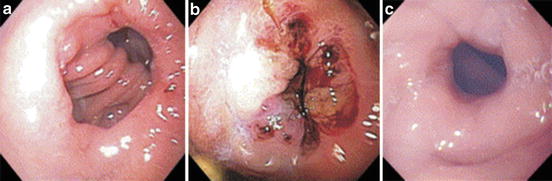
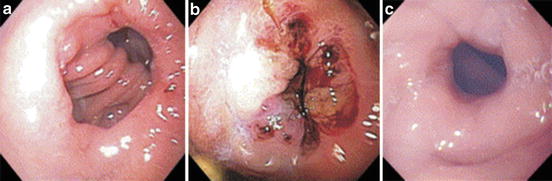
Fig. 11.1
(a) A dilated gastrojejunostomy stoma in a patient gaining weight after gastric bypass. (b) The gastrojejunostomy stoma of the patient in panel (a) after injection with sodium morrhuate (c) The gasrojejunostomy stoma of the patient in panels (a) and (b) after several injections with sodium morrhuate (Reprinted with permission from Catalano M, Rudic G, Anderson A, Chua T. Weight Gain After Bariatric Surgery as a Result of a Large Gastric Stoma: Endotherapy with Sodium Morrhuate May Prevent the Need for Surgical Revision. Gastrointest Endosc. 2007;66:240–245. © 2007 Elsevier) [11]
Reported complications are minimal in most series. The largest series reports a 2.4 % incidence of bleeding, and there is a case report of life threatening hematemesis occurring in a patient who underwent endoscopic sclerotherapy 11 days after a cardiac catheterization with placement of a drug-eluting stent in the left anterior descending coronary artery with institution of daily aspirin and anti-platelet treatment [16]. This procedure is fairly simple, can be repeated on an ambulatory basis, and does not require specialized equipment or training. Longer-term prospective randomized trials are needed to further define the role of this technology.
Bard Endocinch Suturing System
This technology (C.R. Bard, Inc., Murray Hill, NJ) has been used for gastric plication in the treatment of gastroesophageal reflux and for gastrojejunal stoma reduction after gastric bypass. Under endoscopic visualization, suction is used to draw tissue into a hollow capsule at the end of an endoscope. A hollow needle is then used to pass a suture through the tissue held in the capsule. The process is repeated in a second tissue bite, and the suture is tied using a knot-pusher [2]. After pilot studies demonstrated feasibility and safety, the technology was utilized in a randomized, double-blind, Sham-controlled trial of 77 patients with weight loss problems after gastric bypass. The results of this trial are published in abstract form. General anesthesia was used and treated patients underwent anastomotic mucosal ablation and plication of the anastomosis with interrupted stitches. Sequential follow-up was provided for 6 months. Reduction of stoma diameter to <10 mm was achieved in 89 %. Weight loss was modest at 6 months (4.7 % in test patients vs. 1.9 % in controls, p = .041). Weight stabilization or weight loss occurred in 96 % vs. 78 % in controls (p < .001). Adverse events were minor including nausea, vomiting and throat pain [17]. This technology has also been used in a small study to treat refractory dumping after gastric bypass with promising results [18]. No peer-reviewed reports of weight loss trials or additional weight loss studies using this technology are found, and currently, the device is not available.
Stomaphyx
This technology can provide a full-thickness gastric plication, and serosa-to-serosa tissue folds for either antireflux or gastric plication for obesity. The device uses a helical retractor to draw the full-thickness gastric wall into the device and the plication is established by the placement of polypropylene H fasteners. Multiple H fasteners can be placed to achieve gastric volume reduction (Fig. 11.2). In the initial pilot study, 39 patients with late weight regain after gastric bypass underwent endoscopic pouch reduction. Multiple fasteners (12 to 41) were placed, with an average of 17 per patient. Procedure duration averaged 35 min. Adverse events were minor with 87 % experiencing sore throat and 77 % self-limited epigastric pain. Weight loss was modest (10–19 % excess weight loss), with only limited numbers evaluated at 6 and 12 months after the procedure [19].
Fig. 11.2
A diagram showing gastric plication and volume reduction after endoscopic placement of multiple H fasteners (with permission from Endogastric Solutions, ©2014 EndoGastric Solutions, Inc.)
This transoral plication technology was also studied in 64 patients after gastric bypass with inadequate weight loss, gastroesophageal reflux or dumping. An average of 23 fasteners were placed per patient with procedure time averaging 55 min. Adverse events were minor with only two patients requiring observation in hospital, one for transient bleeding and one for nausea. Common adverse events were sore throat and transient epigastric pain. Symptoms were improved in 80 %, and weight loss was modest with only short-term follow-up [20]. This technology has also been used for pouch reduction following vertical banded gastroplasty with only short-term results reported, an average hospital stay of 1.5 days, and only minor adverse events. No long-term weight loss data is provided [21].
More recent studies have raised some concern because two studies suggest that weight loss is maximal in the first 6 months with subsequent weight regain [22, 23]. One of the studies reporting follow-up endoscopy in 12 patients, at an average of 18 months post procedure demonstrates no sustained reduction in pouch or stoma size from the original sizes [22]. In addition, a major life-threatening complication of this procedure, performed by an inexperienced endoscopist, has recently been reported [24]. Currently, this technology is no longer available, but similar technology is in use for transoral fundoplication.
Incisionless Operating Platform
The Incisionless Operating Platform (USGI, San Clemente, CA) combines endoscopy and laparoscopic technologies in a multilumen system with channels for endoscopy and three operating channels for tissue grasping, tissue approximation, and full thickness suture placement (Fig. 11.3a, b). In place of sutures, the system deploys unique tissue anchors that can be drawn together and cinched under direct vision with tactile feedback. The anchors are designed to distribute the tissue tension over a large area, which may be advantageous for tissue healing (Fig. 11.3c).
Fig. 11.3
(a, b) The incisionless operating system provides multiple endoscopic channels, which allow for tissue grasping, tissue approximation and full thickness suture placement. (c) Illustration of a full thickness, serosa to serosa plication using the incisionless Operating System tissue anchors (with permission from USGI Medical, © 2014 USGI Medical, San Clemente, CA)
This technology has been studied in a series of revision procedures following gastric bypass (Restorative Obesity Surgery Endoscopic; ROSE). A pilot study of five patients demonstrated feasibility, safety and short-term weight loss [25]. This trial was continued and expanded to include 20 patients with weight gain and dilated stomas after gastric bypass surgery. Successful tissue plications were accomplished in 17 of the 20 patients with an average of five plications per patient. Procedure time averaged 1 h and 43 min and general anesthesia was utilized. Complications were minor and weight loss averaged 5.8 kg at 1 month and 8.8 kg at 3 months. Technical difficulties occurred in small and narrow gastric pouches [26].
This technology was also studied in a multicenter trial involving 9 institutions and 116 patients with prior gastric bypass. Successful plications were placed in 112 of 116 patients, with an average operative time of 87 min to place 5.9 tissue anchors per patient. Procedures were performed in the operating room (88 %) or the Endoscopy unit (12 %). Most (85 %) were discharged the same day, and complications were minor and self-limited (three asymptomatic superficial distal esophageal tears, pharyngitis, nausea, vomiting, and epigastric pain). Follow-up endoscopy was performed at 3 months (n = 83), and at 1 year (n = 13). Durability of anchors and tissue plication was noted in 94 % at 3 months and in all patients at 1 year. Mean 6-month weight loss was 6.5 kg. The authors noted that technical modifications improved the procedure capabilities [27]. A later review of this same cohort with additional follow-up demonstrated the continued presence of tissue anchors at the 1-year endoscopy exam in 61 of 66 patients studied. The overall 1-year follow-up was 65 % and weight loss was 5.9 ± 1.1 kg. These investigators found in a multiple regression analysis that a smaller stoma was associated with better weight loss [28].
This interesting technology is also being studied in trials of primary endoluminal interventions for weight loss, which will be discussed in a subsequent section of this chapter.
OTSC-Clip
The OTSC-clip (Ovesco Endoscopy, Los Gatos, CA) has been used for treatment of upper gastrointestinal bleeding and closure of the stomach in natural orifice trans-luminal endoscopic surgery. In addition, it has been recently shown to have promise in gastrointestinal leak repair [29]. The clip is made of nitinol (Fig. 11.4a), and applies constant pressure to the tissue between its closed jaws. The clip is mounted on an applicator cap, which attaches to the tip of an endoscope (Fig. 11.4b). The edges of the tissue to be approximated are grasped with forceps and pulled into the applicator cap. The clip is then applied to the tissues in the cap (Fig. 11.4c). This has been studied in 94 patients with loss of satiety or increased meal frequency after banded gastric bypass. The average stoma diameter was 35 mm. General anesthesia was used and procedure time averaged 35 min. Stoma size was reduced by 80 %. There were no major complications. Five patients with post-procedure dysphagia required endoscopy and two needed dilatations. Modest weight loss was reported with follow-up to 1 year [30]. No other trials of this technology for weight regain after bariatric surgery are found at this time.
Fig. 11.4
(a) The OTSC-clip used to approximate gastric tissue. (b) The OTSC-clip mounted on an applicator which is attached to an endoscope. (c) Diagram illustrating the endoscopic application of the OTSC-clip to the gastric wall (with permission from Ovesco Endoscopy USA Inc © 2014 Overco Endoscopy USA Inc.)
Overstitch Endoscopic Suturing System
The OverStitch Endosocopic Suturing System (Apollo Endosurgery, Inc., Austin, TX) is a suture applicator in a cap mounted at the end of a double-channel endoscope (Fig. 11.5a). The anchor, which is passed through the primary channel functions like a curved needle has the capability of placing interrupted, or continuous sutures under direct vision (Fig. 11.5b). The suture is secured using a cinch device.


Fig. 11.5
(a) The suture applicator mounted on a double channel endoscope. (b) The suture applicator at the tip of the endoscope. (c) An endoscopic view of a dilated post-gastric-bypass gastrojejunostomy stoma after stomal reduction with interrupted endoscopic sutures (with permission from Apollo Endosurgery, Inc., Austin TX © 2014 Apollo Endosurgery Inc.)
As yet, there are no published peer-reviewed clinical trials using this technology. The technology has been used in a successful endoscopic closure of a chronic gastro-cutaneous fistula after percutaneous endoscopic gastrostomy [31]. A series of nine patients with gastrojejunal stomal dilatation after gastric bypass underwent stomal reduction with the OverStitch technology and was presented in abstract form only. All stomas were successfully reduced from and average of 26.2 mm to <10 mm in an average time of 36 min, with a median of three interrupted sutures (Fig. 11.5c). Weight loss at 1 month was 6.9 % of total weight. Several complications were reported. All were minor except one patient who required balloon dilation after 4 days [32]. Several other small series demonstrating feasibility and safety have been recently presented at national forums. This technology is promising and appears to provide good full-thickness tissue approximation. It may also be an important technology for the treatment of leaks, fistulas, and other bariatric complications [2].
Endoscopic Intervention as a Primary Treatment of Obesity
Gastric Balloon
The gastric balloon is the most widely studied endoscopic intervention for weight loss. Beside its space occupying effect in the stomach, there is another physiologic rationale for this intervention. Gastric distension is a stimulus for cholecystokinin secretion from the duodenum. In addition to its other better-known effects, cholecystokinin delays gastric emptying and causes pyloric constriction. Gastric distension does appear to influence satiety and results in decreased food intake [33].
The original gastric balloon was introduced in 1985. This balloon was insufflated with 220 ml of air, which is now considered too little volume. Modest weight loss was observed, but complications including gastric erosions, gastric ulcers, small intestinal obstruction and esophageal injuries during placement resulted in its removal from the market. After a panel of experts was convened for design recommendations and an extended period of research, the BioEnterics intragastric balloon (BIB, Allergan Inc., Irvine, CA) was introduced. This balloon is spherical, made of non-irritating silicone elastomer, and holds 400–700 ml of saline (Fig. 11.6




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








