7 The Tech Sector: Lasers, Light, and Energy Devices
Summary
Lasers and light-based therapies are powerful and versatile nonsurgical tools that can be used to treat a wide range of cosmetic and medical dermatologic conditions, including several that are more prevalent in men. As the number of male patients seeking non-invasive cosmetic procedures continue to increase, tailoring treatment methodologies to account for gender-specific anatomical variances and preferences will be essential in optimizing cosmetic outcomes and increasing patient satisfaction. Herein this chapter we will review the major classes of lasers by clinical indication, with particular focus on their use in men.
Keywords: lasers lasers in men laser hair removal laser tattoo removal laser resurfacing vascular lasers.
7.1 Background
The demand for surgical and nonsurgical cosmetic procedures has increased dramatically in the past decade, with an estimated 18,100,000 procedures performed in 2019 alone.1 Although the total number of yearly cosmetic procedures has risen by 44.8% since 2009, minimally invasive procedures account for 94.6% of this increase, with laser and light-based treatments encompassing a significant portion of this growth.1,2
Although the demographic landscape of the cosmetic market is comprised mostly of female patients, interest in cosmetic procedures has also been steadily increasing among male patients, with 1,300,000 total cosmetic procedures performed in 2019 according to the American Society of Plastic Surgeons.1 Minimally invasive procedures accounted for the vast majority of this volume (83.7%), with laser hair removal (LHR) and laser skin resurfacing ranking as the second and sixth most popular procedures among male patients, respectively.1
A multitude of factors contribute to the rising interest in laser and light-based therapies among male patients. Advancements in the field of lasers and light-based therapies have provided aesthetic patients a minimally invasive option for treating a large breadth of cutaneous cosmetic concerns, including several conditions that are more prevalent or severe in the male population such as acne scarring, rhytids, pseudofolliculitis barbae (PFB), and rhinophyma.3 These procedures can often deliver meaningful yet subtle natural results while also offering minimal downtime and reduced risk—characteristics that have been highlighted in recent research as important considerations for male aesthetic patients.4,5 Furthermore, it is the opinion of the authors that laser and light-based therapies carry a lower risk of feminizing the face compared to other minimally invasive modalities, such as injectable dermal fillers.
As awareness and social acceptability of cosmetic procedures continue to rise among male patients, it is essential that health care professinals understand not only the capabilities and limitations of different treatment options available but also the distinct nuances of male facial anatomy. Adapting treatment protocols to account for these differences and appreciating the varied treatment goals of different patient demographics will lead to improved cosmetic outcomes and patient satisfaction.6 Herein this chapter we will review these topics as they pertain to laser and light-based therapies.
7.2 Anatomy and Physiology
As the largest organ in the human body, the skin is comprised of multiple layers and complex adnexal structures that serve various barrier, immunologic, thermoregulatory, and sensory functions.7,8 It is well established that genetics and hormonal differences contribute to underlying sex-related biophysical differences in cutaneous structure and function.9 These differences can have implications not only in the prevalence and pathogenesis of certain skin diseases but also in terms of treatment protocols and cosmetic interventions. Knowledge of these underlying gender-linked differences is essential when performing laser and light-based therapies on men.
Multiple studies have demonstrated that dermal skin thickness is increased in men compared to women across all ages and anatomical regions.8,10,11 Additionally, whereas skin thickness decreases linearly over time in men, it has been shown to remain constant in women up until the fifth decade, after which it steadily declines.10 These observations have been attributed to the influence of sex hormones on collagen production, which has been shown to directly correlate with skin thickness in both animal models and humans.8,11–13 On the contrary, men tend to have less subcutaneous adipose, which, combined with stronger muscles of facial expression, may lead to more severe, dynamic wrinkles in certain locations such as the forehead.5,14,15 Additionally, men may initially present with deeper wrinkles because they tend to pursue cosmetic treatment at later stages compared to women.5 In order to achieve a comparable cosmetic result in men, more aggressive protocols or greater number of laser and light-based treatments may be required.
Men also have a greater density of dermal microvessels, resulting in greater baseline facial skin arterial perfusion. This perfusion is especially increased in the lower face, which is highly vascularized to support the coarse terminal hairs in the beard region.5,6,16 Consequently, male patients experience a higher rate of postoperative bleeding complications after undergoing plastic facial surgical procedures such as rhytidectomy.17 Likewise, they may be at increased risk of bruising after certain laser procedures.
There are also gender-related differences in hair characteristics and distribution. The effect of androgens on hair growth in men can vary according to anatomic region.9 Men typically will have an increased density of coarse terminal hairs on the face and neck compared to women. Thus, physicians should be cognizant of the potential risk to inadvertently damage hair follicles when performing laser and light-based procedures on the face and neck.
As with the other features of male cutaneous anatomy discussed earlier, the sebaceous and eccrine glands on the face are also hormone dependent. Adult male patients generally exhibit larger pore sizes and secrete significantly greater amounts of sebum compared to age matched female patients, which may explain why males are more prone to certain diseases, such as rhinophyma or more severe acne resulting in more severe scarring.8,11,18,19
Awareness of these anatomical and physiologic gender-related differences is important when counseling male cosmetic patients and constructing problem-based treatment plans that optimize cosmesis and minimize potential adverse outcomes.
7.3 Introduction to Lasers
Most modern-day lasers in clinical dermatology employ the theory of selective photothermolysis, which was introduced by Anderson and Parrish in 1983.20 This theory details how pulsed laser energy can be applied to preferentially target specific structures in the skin for thermally mediated injury while minimizing damage to surrounding tissues. This process involves a combination of selective light absorption by specific chromophores present in the skin and applying a pulse duration equal to shorter than the thermal relaxation time (TRT) of the target tissue so that thermal injury is confined to the desired regions, minimizing the potential for adverse effects.20 Additionally, the fluence, or energy density, must be adequate to destroy the intended target.21
Clinically relevant chromophores can be endogenous or exogenous. The principle endogenous chromophores in the skin include water, melanin, and hemoglobin. Exogenous chromophores most often include tattoo pigment. The majority of lasers available today emits energy at specific wavelengths that correspond to the absorption spectrum of one or more of these chromophores.22 Importantly, the laser–skin interaction is complex and depends on several additional factors such as the size, depth, and surrounding environment of the target tissue.23 These anatomic elements, which can vary significantly with gender, must also be considered when selecting laser parameters such as wavelength, pulse duration, spot size, and fluence.
Lasers can be broadly categorized based on their intended targets and clinical applications. In the following sections, we will review the major classes of lasers and their common clinical applications in male aesthetic patients.
7.3.1 Resurfacing Lasers
Advances in laser resurfacing technology have provided laser surgeons powerful nonsurgical tools to address a wide range of cosmetic cutaneous concerns, such as photoaging, rhytids, dyspigmentation, scarring—including hypertrophic scars and keloids, and superficial skin growths. Modern-day resurfacing lasers can be broadly categorized into two main classes—ablative and nonablative, both of which can be subdivided further into fractionated and traditional, or full field, forms.24 In general, ablative resurfacing techniques vaporize the epidermis, leading to prolonged recovery times, but in many cases yielding more dramatic cosmetic results. Nonablative techniques preserve the epidermis and thus are associated with shortened recovery times and fewer side effects.
7.3.2 Ablative Resurfacing Lasers
Traditional ablative resurfacing lasers include the 10,600-nm carbon dioxide (CO2) lasers and the 2,940-nm erbium:yttrium aluminum garnet (Er:YAG) laser. CO2 lasers emit light at a wavelength absorbed by water in skin tissue, triggering water superheating and destruction of the entire epidermis and a variable part of the dermis to a controlled depth.25 Thermal injury is also extended to the adjacent tissue causing coagulation necrosis in the area directly bordering the ablated tissue.26 Further away from the direct interaction, there is reversible thermal damage, which causes heat-induced collagen shrinkage and leads to tighter and smoother skin during the healing process.26,27
Traditional full-field ablative CO2 lasers were highly efficacious for treatment of photodamaged skin; however, they carried notable risk for posttreatment side effects such as edema, prolonged erythema, burning discomfort, pigmentary alteration—including delayed-onset permanent hypopigmentation—infection, and scarring.27–30 In a retrospective analysis of 500 patients who underwent cutaneous laser resurfacing with a CO2 laser by a single operator, 100% of patients developed postoperative erythema lasting on average several months, and 37% of patients developed hyperpigmentation lasting on average 32 days postoperatively.28 The risk of postprocedure pigment alteration is greater in patients with Fitzpatrick skin type IV or greater (Fig.7.1).28,31
The Er:YAG laser was developed after CO2 lasers in an attempt to retain the benefits of ablative CO2 laser resurfacing while decreasing side effects. Er:YAG laser emits near-infrared light at a wavelength of 2,940 nm, which yields an absorption coefficient of water 16 times that of the CO2 laser.32 As the epidermis is composed predominantly of water, the vast majority of the laser energy is absorbed superficially. This corresponds to more superficial ablation with less surrounding thermal damage in the dermis. Therefore, the Er:YAG laser results in less dermal coagulation, and may be associated with poorer intraoperative hemostasis.25 Although the Er:YAG laser was effective for superficial targets and offered faster recovery time, it was less effective than CO2 lasers when targeting deep rhytids and skin laxity, controlling for fluence per pulse and number of passes.26 Consequently, increasing the pulse duration or number of passes is often needed to achieve the desired depth of thermal damage and clinical outcome.33,34 A retrospective study found similar side effect profiles and comparable healing times in 100 patients who underwent laser skin resurfacing with either single-pass CO2 or multipass long-pulsed Er:YAG.33
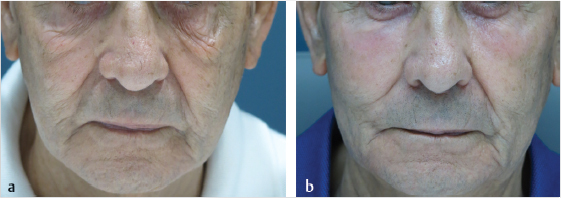
Fig. 7.1 (a) Lower eyelid laxity and photodamage (pre-treatment). (b) Post-treatment after one session with ablative full field 10,600 nm CO2 laser. (Courtesy of Jose Raul Montes, MD).
Fractional ablative technology has largely replaced the traditional full-field ablative resurfacing lasers, which, although very effective, were undermined by their significant posttreatment morbidity and side effect profiles. Fractionated ablative resurfacing employs the concept of fractional photothermolysis, which involves creation of vertical columns of epidermal and dermal ablation, also known as microscopic treatment zones (MTZs), surrounded by uninjured tissue at regularly spaced intervals.35 Only a fraction of the skin is treated in an individual session, and the presence of adjacent unaffected tissue offers a viable reservoir of cutaneous stem cells, which can facilitate rapid re-epithelialization.36 As a result, fractional ablative methods tend to have fewer posttreatment side effects and less downtime compared to traditional full-field ablative laser resurfacing, while still offering meaningful cosmetic outcomes.24,37,38 Skin resurfacing with fractional ablative CO2 or Er:YAG lasers can therefore be an option for men with deeper rhytids, significant solar elastosis, or skin laxity. However, it is important to note that although fractionated ablative lasers are safer than their nonfractionated counterparts, they still carry increased risk and recovery time compared to nonablative fractionated lasers, which have become the contemporary standard for skin resurfacing.39 Notably, prolonged erythema of up to 2 months have been reported, which may be particularly challenging for male patients, who do not typically wear makeup to camouflage skin.36
Beyond photorejuvenation, ablative lasers can be used to treat rhinophyma, a cosmetically disfiguring complication of rosacea that almost exclusively affects male patients at a ratio of 30:1 compared to female patients.40 Rhinophyma is characterized by progressive bulbous enlargement of the nose, sebaceous gland hyperplasia, enlarged pores, hypervascularity, and fibrosis.41 Although a benign entity in of itself, rhinophyma can often be psychologically distressing and cause functional impairment such as nasal obstruction in the late stages.42 Management can be difficult and usually necessitates surgical or destructive procedures. Full-field and fractionated ablative CO2 and Er:YAG lasers have all been shown to be tolerable, effective, and provide comparable results to electrosurgery (Fig. 7.2).43,44,45,46
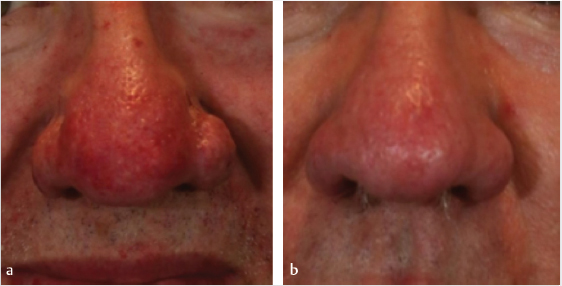
Fig. 7.2 (a) Rhinophyma (pre-treatment). (b) Post-treatment after one session with ablative full field 10,600 nm CO2 laser. (Courtesy of Jennifer L. MacGregor, MD).
7.3.3 Nonablative Resurfacing Lasers
The original nonablative resurfacing lasers entered the clinical arena in the late 1990s in response to concerns regarding prolonged recovery time and posttreatment complications associated with traditional full-field ablative lasers.24,29 Nonablative resurfacing is based on the premise that dermal thermal injury is the catalyst for collagen formation, remodeling, and contraction, and thus the basis for the clinical improvement seen with ablative resurfacing lasers.47 Nonablative lasers that were traditionally used for resurfacing purposes emitted light at wavelengths that were either absorbed by oxyhemoglobin in dermal vasculature (585–595 nm) or dermal water (1,000–1,500 nm)21,47 or 585- and 595-nm pulse dye lasers have been trialed for skin resurfacing purposes, and although well tolerated, their use in this capacity is limited due to overall inconsistent and unimpressive results.48,49 The long-pulsed 1,320-nm neodymium:yttrium aluminum garnet (Nd:YAG) laser was the first laser marketed exclusively for nonablative skin resurfacing.50 At this infrared wavelength, absorption by superficial epidermal tissue is relatively weak, which allows for energy penetration deeper into the dermis. Nonablative systems also utilize concomitant cooling devices to further prevent epidermal heating and damage. Because the epidermis is preserved, downtime and risk of side effects are minimal. Although several studies have demonstrated clinical improvement in the appearance of mild to moderate winkles and acne scarring with the 1,320-nm Nd:YAG laser, the effects are generally mild compared to their ablative counterparts and require multiple sessions to achieve.51,52,53 Other infrared lasers that have been used for nonablative skin resurfacing include the 1,064-nm Nd:YAG, 1,450-nm diode, and 1,540-nm erbium:glass lasers. These systems also exhibit similar side effect profiles and limitations in efficacy.
The first commercially available fractional resurfacing device was the nonablative fractionated laser, which has since become the most popular and widely utilized class of resurfacing lasers, especially in male patients.54 Nonablative fractionated lasers are more effective than their nonablative predecessors while concomitantly offering faster recovery and a more tolerable side effect profile compared to ablative resurfacing.32
Men and women may seek resurfacing laser treatments for different reasons. A retrospective review of a single dermatologist’s experience over a 14-month period found that the most popular concern among men seeking nonablative fractional resurfacing was acne scarring, accounting for 44% of male patients compared to only 14% of female patients.54 This correlates with the greater prevalence of severe nodulocystic acne in men, likely due to the effects of androgens on the skin.55 Several studies have corroborated the safety and efficacy of the 1,550-nm erbium fiber fractional laser in the treatment of acne scarring, including patients of Fitzpatrick skin types IV to VI.56,57
Improving the appearance of photoaged skin is another common reason why both the male and female patient may pursue resurfacing treatments.54 Multiple wavelengths utilized within nonablative fractional devices, such as 1,470, 1,540, 1,550, and 1,927 nm, have been shown to be effective for men who wish to improve the texture, tone, and pigmentation of photodamaged skin. One device offers both the 1,550- and 1,927-nm wavelengths, as the 1,550-nm wavelength is more effective at targeting solar elastosis and stimulating neocollagensis as it penetrates deeper in the dermis while the 1,927-nm wavelength targets superficial structures of the skin and has been shown to improve pigmentation as well as treat actinic keratoses.58,59 Actinic damage is significantly more prevalent in men, especially among elderly men with androgenetic alopecia.60 Results of a prospective, multicenter study suggest that the combination of wavelengths in a single treatment is a safe and effective treatment to address both the deeper and superficial sequelae of photodamaged skin.58
Picosecond pulse duration lasers such as the 755-nm alexandrite laser with a diffractive lens array, and the dual 532 and 1,064 nm with holographic beam splitter, have also been shown to be a safe and effective option for the treatment of facial acne scarring and photoaging, even in darker skin tones.61,62,63,64 Although picosecond pulse duration lasers were originally developed with removal of tattoo and pigmentation in mind, the combination with a diffractive lens array allows the picosecond pulse to be distributed into few highly concentrated beams surrounded by background areas with low-level heat energy. The unique action of these high-energy beams promotes neocollagenesis without ablation with minimal side effects and downtime, with posttreatment erythema lasting only for several hours.62,63,65
7.4 Pigmentation
7.4.1 Laser Hair Removal
In 2019, LHR was the second most popular noninvasive cosmetic procedure among men, with more than 170,000 procedures performed.1 This represents a 100% increase from 2000.1,66 For men, the most commonly treated areas include the neck, chest, and back. The targeted chromophore in LHR is melanin in the hair shaft, which, upon absorption of sufficient laser energy, will induce thermal injury to nearby hair stem cells in the hair bulge and bulb.67
Melanin does not exhibit a single absorption peak. Rather, it absorbs wavelengths from 400 to 1,200 nm, with greater absorption at the lower end of this spectrum.68 Consequently, lasers that emit light at lower wavelengths carry higher risk for epidermal damage and subsequent dyspigmentation or scarring, especially in individuals of darker skin types.69 Although the ideal LHR candidate may be a patient with fair skin and dark terminal hairs, utilizing longer wavelength lasers and concomitant epidermal contact cooling can diminish the risk for epidermal injury in patients with darker skin types. Conversely, longer wavelength lasers are less effective at destroying lightly pigmented or thinner hair due to relatively weaker melanin absorption.
Although used less in practice today, the long-pulsed ruby laser was one of the first lasers approved for hair removal. At an emission wavelength of 694 nm, light from the ruby laser is avidly absorbed by melanin and does not penetrate deeply into the skin, limiting its use in patients with darker skin types, especially during the summer months, given high risk of blistering, burns, and pigmentary alteration.70
The 755-nm alexandrite laser is a popular and effective option for patients with Fitzpatrick skin types I to III. At 755 nm, the alexandrite laser penetrates deeper than the 694-nm ruby and thus is theoretically safer in darker skin types; however, a retrospective study looking at the side effect profiles of different hair removal lasers in Fitzpatrick skin types I to V found that the 755-nm alexandrite laser was associated with higher risk of side effects compared to the 1,064-nm Nd:YAG laser.70 Thus, caution is still advised in patients with darker skin types.
The 810-nm diode laser is also a popular and effective option for LHR.71,72 In head-to-head comparative study of patients undergoing LHR with diode, Nd:YAG, and alexandrite lasers, the diode laser and alexandrite were more effective than Nd:YAG, a finding that was statistically significant.73 Meanwhile, there was no statistically significant difference between the diode and alexandrite lasers.73 Newer versions of the diode laser offer larger spot sizes resulting in brisk treatment of larger surface areas such as the chest and back.74 Although diode lasers are generally thought to be safer than its lower wavelength counterparts, some of the same concerns regarding unwanted collateral epidermal damage in darker skin individuals remain (Fig. 7.3).
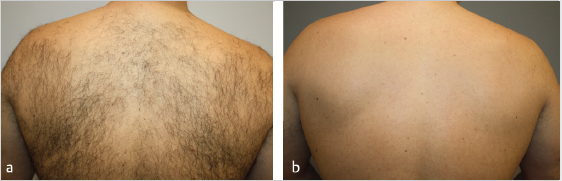
Fig. 7.3 (a) Unwanted hair (pre-treatment). (b) Post-treatment after six sessions with a 1064-nm Nd:YAG. (Courtesy of Shino Bay Aguilera, DO).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








