Fig. 15.1
Completed graft for intra-articular anterior cruciate ligament (ACL) reconstruction with lateral extra-articular augmentation. A gracilis autograft has been passed through a 4.5 mm hole (black arrow) drilled in the semi-trapezoidal tibial bone block of a patellar tendon autograft. The smaller patellar bone block has been shaped to easily fit in a 9 mm tibial tunnel (white arrow)
While the graft is being prepared, preparation of the knee continues. Prior to arthroscopy, an incision is created on the anterolateral knee extending from just proximal to the lateral epicondyle to the level of Gerdy’s tubercle (GT). One then divides the iliotibial band (ITB) in line with its fibers from the level of Gerdy’s tubercle proximally to the end of the incision, taking care not to damage the underlying lateral collateral ligament (LCL) (Fig. 15.2). The LCL is identified by palpation with the knee in Fig. 15.4 position. Soft tissue is cleared to provide good visualization of the ligament, but dissection under the ligament is avoided prior to arthroscopy to prevent extravasation of arthroscopic fluid.
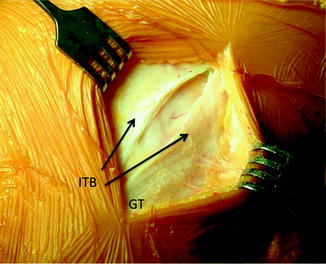
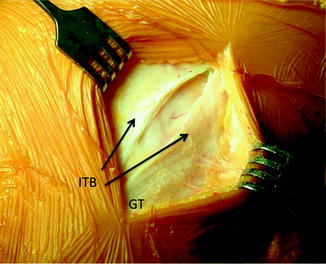
Fig. 15.2
An anterolateral incision extending proximal from Gerdy’s tubercle (GT) has been carried down through the iliotibial band (ITB)
Gerdy’s tubercle is then identified in the distal portion of the incision and a small amount of the origin of the tibialis anterior is elevated to improve visualization. A bone tunnel from superomedial to inferolateral is created with an awl and dilated sufficiently to allow passage of a doubled gracilis graft (Fig. 15.3).
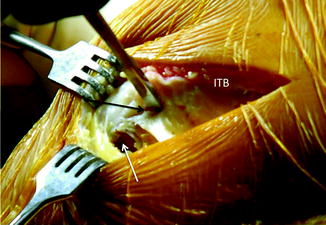
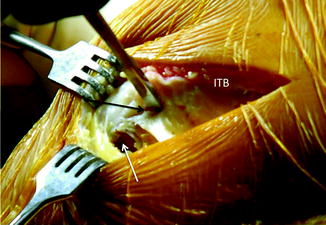
Fig. 15.3
View through the anterolateral incision and divided ITB. The bone tunnel through Gerdy’s tubercle (GT) has been created inferolaterally with an awl (white arrow) after elevating some of the origin of the tibialis anterior. The superomedial end of the bone tunnel is being created with an awl (black arrow)
At this point the arthroscope is placed into the knee and notch preparation proceeds as with an isolated intra-articular reconstruction. Tunnel placement may be complicated in revision cases. Decisions must be made regarding tunnel reuse vs. the creation of new tunnels. The femoral tunnel is generally drilled to 10 mm and the tibial tunnel to 9 mm. If significant bone loss is present from a prior femoral tunnel, the tibial bone block size can be increased at harvest to fill this defect and still obtain a good press fit.
The graft is passed in an antegrade direction (from femur to tibia) and the patellar bone block is directed into the tibial tunnel. Femoral fixation is achieved with a press-fit technique, simultaneously fixing the lateral extra-articular graft into the femur (Fig. 15.4). Tibial fixation of the intra-articular graft is then performed with an interference screw.
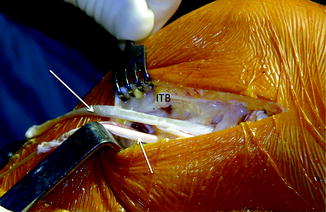
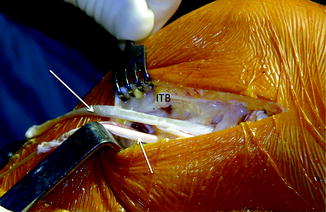
Fig. 15.4
View through the anterolateral incision and divided ITB. The intra-articular portion of the graft has been passed into the knee in an antegrade direction. The two limbs of the gracilis graft (arrows) that have been looped through the bone block prior to press-fitting the graft into the femur can be seen
The two free ends of the gracilis graft are then passed toward the tibia for fixation into Gerdy’s tubercle. The more posterior limb is passed under the LCL, superficial to the popliteus tendon, and through the tunnel in Gerdy’s tubercle in a superomedial to inferolateral direction. The other limb is passed under the LCL, superficial to the popliteus tendon, under the posterior portion of the ITB, and through the same tunnel in Gerdy’s tubercle in an inferolateral to superomedial direction. The graft is tensioned with the knee in approximately 30° of flexion and neutral rotation and the two limbs of the graft are sutured to each other in a side-to-side manner, completing the reconstruction (Fig. 15.5).
Fig. 15.5
Line drawing demonstrating the completed graft position. Note that the graft passes deep to the lateral collateral ligament (LCL) as it passes toward Gerdy’s tubercle (GT) from its femoral attachment site proximal to the LCL origin
In the rare case of well-placed and intact intra-articular graft that fails to adequately control rotation, one can consider the addition of a lateral extra-articular reconstruction. We prefer to utilize the central third of the ITB for such reconstructions as described by Lemaire [24, 25].
Outcomes
The role of lateral extra-articular augmentation of intra-articular ACL reconstruction procedures remains unclear due to a lack of high-level evidence. Published comparative studies of patients with and without lateral extra-articular augmentation have reported inconsistent results. Several authors have reported no difference in stability with lateral augmentation [26, 27], while others have demonstrated increased stability with augmentation, generally in specific populations such as female athletes reconstructed with soft tissue grafts [28] and those with significant lateral compartment translation preoperatively [13–15].
Specific to the revision ACL population, Trojani et al. recently noted an improvement in the pivot-shift in patients in whom a lateral extra-articular augmentation was added to an intra-articular reconstruction [19]. They noted a persistent pivot-shift in 35 % of patients treated with intra-articular reconstruction along vs. 19 % in those in whom the intra-articular reconstruction was augmented. However, they noted no difference in the overall IKDC scores between patients in the two groups.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree