CHAPTER 9 The Papular and Pruritic Dermatoses of Pregnancy
Introduction
The papular and pruritic dermatoses of pregnancy encompass three historical disease entities that are described in the same chapter because each of the terms applied is still quoted in the literature: (1) prurigo of pregnancy; (2) papular dermatitis of pregnancy; and (3) pruritic folliculitis of pregnancy.
Significant overlap between them and the lack of unequivocal clinical or diagnostic features, as available in pemphigoid gestationis, polymorphic eruption of pregnancy, and intrahepatic cholestasis of pregnancy, have led to considerable doubt that they were all distinct clinical entities. Indeed, papular dermatitis of pregnancy was the first to be no longer regarded as a distinct condition but to belong in the spectrum of prurigo of pregnancy. And prurigo of pregnancy and pruritic folliculitis of pregnancy, according to the most recent classification of pregnancy dermatoses1, are now summarized within a new disease complex that has been termed atopic eruption of pregnancy (AEP: see Chapter 8). This chapter shortly outlines the historical background and clinical characteristics of each entity.
Prurigo of pregnancy
In 1904, Besnier et al. first introduced the term “prurigo gestationis”’ to include all patients with pregnancy-related dermatoses, other than those with herpes gestationis2. At that time, “prurigo” was the term used to describe atopic dermatitis; Besnier was the first to describe the association between atopic dermatitis, allergic rhinitis, and asthma3,4. Costello, in 1941, coined the term “prurigo gestationis of Besnier” and estimated an incidence of 2%5. The condition was first clearly outlined by Nurse in 1968, who termed it “early-onset” prurigo of pregnancy, in contrast to a late form, that is nowadays known as polymorphic eruption of pregnancy6. Nurse described accompanying eczematous features in most of his 31 patients with early-onset prurigo. But it was Holmes and Black in 1983 who first suggested that prurigo of pregnancy would result from pruritus gravidarum in women with atopic diathesis rather than being a distinct entity7. They based their argument on the finding that 18% of pregnancies are complicated by pruritus8 and that 10% of the population displays atopy9. It might therefore be expected that both conditions would coincide in about 2% of pregnancies. In a large retrospective study on more than 500 pregnant patients with pruritus, 45/49 (92%) patients originally diagnosed with prurigo of pregnancy met the preset criteria of atopic eczema1. The remaining 4 patients all showed multiple minor criteria of atopy, as outlined by Hanifin and Rajka10, and shared histopathological features with eczema. Based on these observations, prurigo of pregnancy was included in a new disease complex that was termed “atopic eruption of pregnancy” and summarizes all patients formerly labeled as eczema in pregnancy, prurigo of pregnancy, and pruritic folliculitis of pregnancy.
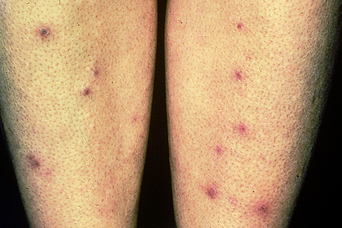
Clinically, the lesions formerly described as prurigo of pregnancy today represent the “P-type” variant of AEP (see Chapter 8). Lesions, then and now, are described as discrete erythematous or skin-colored papules, which are extremely pruritic, with the result that an excoriated surface soon develops over the papules. The papules tend to be small and are seldom larger than 0.5 cm in diameter. Characteristically, the papules appear on the extensor surfaces of the extremities and trunk (Figures 9.1–9.3). The histological features of prurigo of pregnancy have not been studied systematically, and consequently the diagnosis has been made on clinical criteria alone. Where biopsies have been performed, the pathology usually shows nonspecific findings such as mild acanthosis, parakeratosis, and surface excoriation. A mixed perivascular infiltrate is found, often containing eosinophils and some neutrophils7. Direct immunofluorescence (DIF) is negative7.
Prurigo of pregnancy has always been considered a benign disorder, as is AEP nowadays. However, the patient may find the persistent pruritus distressing. Symptomatic relief of pruritus can usually be achieved with moderately potent topical corticosteroid creams and oral antihistamines at night.