and Berthold Rzany2
(1)
Clínica Médica Dr Mauricio de Maio, São Paulo, São Paulo, Brazil
(2)
RZANY & HUND Privatpraxis für Dermatologie und Ästhetische Medizin, Kurfüstendamm, Berlin, Germany
6.1.1 Introduction
6.1.2 Anatomy
6.1.4 Techniques
6.2 Temples
6.2.1 Introduction
6.2.2 Anatomy
6.2.4 Technique
6.2.5 Complications
6.3 Eyebrow
6.3.1 Introduction
6.3.2 Anatomy
6.3.4 Technique
6.3.5 Complications
6.4.1 Epicanthal Fold
6.4.2 Sunken Upper Eyelid
6.5.1 Introduction
6.5.2 Anatomy
6.5.5 Cheekbones
6.5.6 Cheek
6.5.7 Complications
6.6 Nose Reshaping
6.6.1 Introduction
6.6.2 Anatomy
6.6.4 Technique
6.6.5 The Nasofrontal Angle
6.6.6 The Nasolabial Angle
6.6.8 Dorsum
6.6.9 Selection of Filler
6.6.10 Complications
6.6.11 Tips, Tricks and Key Points
6.7 Nasolabial Folds
6.7.1 Introduction
6.7.2 Anatomy/Structure
6.7.4 Technique
6.7.5 Touch-Up
6.7.6 Complications
6.8 The Earlobe
6.8.1 Introduction
6.8.2 Anatomy/Structure
6.8.4 Technique
6.9.1 Introduction
6.9.2 Anatomy
6.9.4 Technique
6.9.5 Complications
6.10 Marionette Lines
6.10.1 Introduction
6.10.2 Anatomy
6.10.4 Technique
6.10.5 Complications
6.10.6 Tips, Tricks and Key Points
6.11.1 Introduction
6.11.2 Anatomy
6.11.4 Technique
6.11.5 Complications
6.11.6 Tips, Tricks and Key Points
6.12.1 Introduction
6.12.2 Facial Advancement
6.12.3 Tips, Tricks and Key Points
Abstract
In the following chapter, the indications will be discussed separately. However, one must be aware that treating one indication might influence the other indication, e.g., treating the temporal region may influence the position of the eyebrow and treating the cheek will influence the appearance of the tear trough and infraorbital hollow.
In the following chapter, the indications will be discussed separately. However, one must be aware that treating one indication might influence the other indication, e.g., treating the temporal region may influence the position of the eyebrow and treating the cheek will influence the appearance of the tear trough and infraorbital hollow.
6.1 Forehead and Glabella
6.1.1 Introduction
The forehead and glabellar areas are characterized by extensive mimic movements of three main muscles: Mm. occipitofrontal, corrugator, and procerus. Horizontal forehead lines appear when the occipitofrontal muscle is activated. The vertical glabellar folds result from the continuous contraction of both corrugator muscles. The horizontal lines in the glabellar area arise from pronounced procerus muscle activity. With time, these lines become embedded into the skin and will not disappear after BoNT-A treatment. Therefore, the best possible overall effect may be gained using fillers (Fig. 6.1).
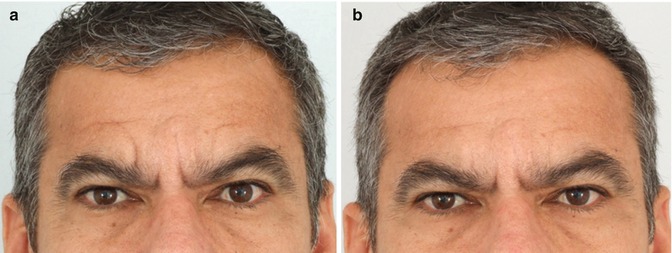
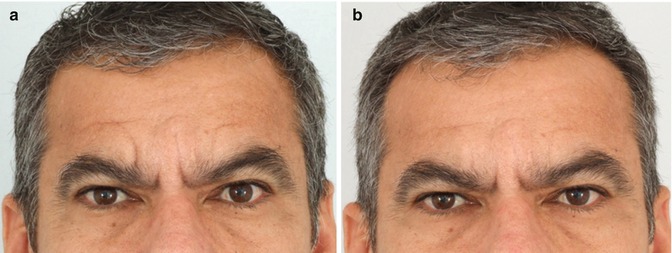
Fig. 6.1
(a) Analysis of the patient at rest: observe that due to overcontraction of the corrugators over time, the patient became hypertonic and is unable to relax these muscles anymore with the result of deep static wrinkles. BoNT-A alone would not be able to correct those lines or maintain a long-lasting result. (b) The patient was submitted to deep injection with HA with a 21G blunt cannula in both scar-like medial and lateral vertical wrinkles. No BoNT-A was injected and there is persistence of corrugators contraction
6.1.2 Anatomy
The aesthetic forehead unit comprises the upper one-third of the classical “facial thirds.” It extends vertically from the supraorbital rim to the anterior hairline. The skin on the forehead is generally thicker than on the lower face, and five layers are encountered at this level: the skin, the subcutaneous tissue, the galea aponeurotica, a part of the submuscular aponeurotic system ( SMAS), the loose subaponeurotic areolar layer, and the periosteum.
The fascia superficialis is known as the temporoparietal fascia in the temporal area and as the galea in the forehead. There is a fat pad called the galea fat pad in the glabella and above the eyebrows. The superficial fat is sparse in the forehead, glabella, temporal, and orbital areas. It is dense due to fibrotic septa in the forehead region. Deep fat is dense in the temporal and periocular areas. At this level, the temporal extension of the deep fat pad of Bichat may be found. In the upper face, the SMAS denominated the galea aponeurotica, which envelops the frontalis, the occipitalis, and the procerus. The frontalis forms the frontal belly of the occipitofrontal muscle and is inserted into the galea aponeurotica. The galea connects the frontalis and the occipital muscles. In the central forehead, the frontalis muscle is paired and united by the superficial fascia. It raises the eyebrows and produces the forehead hyperkinetic lines. The frontalis antagonists are the corrugators, procerus, and orbicularis oculi.
The supraorbital artery is a terminal branch of the ophthalmic artery from the internal carotid artery. The superficial temporal artery is the terminal branch of the external carotid artery and divides into two major branches. The carotid veins accompany these arteries. The frontal branch of the facial nerve may be found within the temporoparietal fascia, from the midportion of the zygomatic arch up to its entrance to the frontalis muscle. It provides motor innervation to the frontalis, corrugator, and procerus muscles. It also innervates the cephalic portion of the orbicularis oculi (Pitanguy and Ramos 1966). The supratrochlear nerve exits the orbit between the periosteum and the orbital septum at the medial supraorbital rim. It runs along the caudal aspect and within the corrugator muscle and then superiorly on the inner surface of the frontalis fascia to supply sensation to the medial and central forehead. The supraorbital nerve exits between the medial and central thirds of the superior orbital rim and runs superiorly and laterally on the inner surface of the frontalis fascia and galea. It is responsible for sensation in the anterior lateral forehead and scalp.
6.1.3 Patient Evaluation and Selection
Patients should be critically appraised for possible pretreatment with BoNT-A; additional filler therapy in these areas often turns out to be unnecessary after pretreatment with BoNT-A. Persistent wrinkles after BoNT-A treatment as the residual wrinkles above the lateral eyebrows may benefit from the treatment with an injectable filler. Patients presenting deep forehead and glabellar folds will require a filler that can be injected more deeply (subcutaneous or intramuscular planes) to increase volume (Fig. 6.2). Patients presenting superficial forehead and glabellar folds or lines may benefit from a fine or very fine filler that must be injected more superficially (Fig. 6.3). Furthermore, for patients with advanced elastosis, repeated treatments with injectable fillers may rejuvenate the whole area. For deep and superficial forehead and glabellar folds, the appropriate fillers should be combined and the proper use of needles or cannulas should be considered.

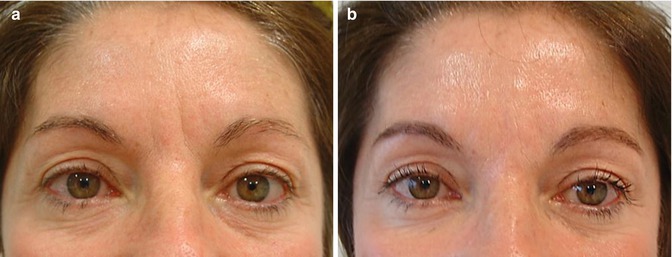

Fig. 6.2
(a, b) Before and 3 weeks after treatment with BoNT-A. Status: relaxed. (c, d) Before and 3 weeks after the treatment with BoNT-A. Status: at maximum frown. (e, f) Immediately after injection of hyaluronic acid relaxed and maximum frown. Please note: the erythema is not always necessarily present
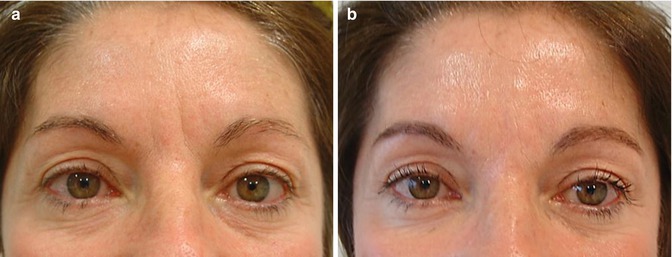
Fig. 6.3
(a) Superficial static lines over the glabella. (b) The patient was submitted to the injection of HA fine lines with a 30G cannula into the superficial dermis to avoid vascular occlusion. BoNT-A was not injected
6.1.4 Techniques
Anesthesia is not usually necessary. Most injectors use the retrograde tunnel technique (i.e., the filler is injected while withdrawing the needle), as it allows a faster application. However, the multiple injection site technique can also be used. This technique will help to blend the filler better into the surrounding area. Deep and superficial forehead and/or glabellar lines may require multilevel injections. The injection should not be too deep. An injection below the fascia may encourage migration of the filler (e.g., from the glabella to the perinasal area). To avoid an occlusion of the arteries, which have been reported for the glabella and forehead area, all injections should be done very carefully, if possible through a 30G or even blunt cannulas when deep planes are treated. Higher volumes should be avoided in this area. Usually 0.2–0.3 ml of an HA filler may be sufficient for the glabellar area (Bachmann et al. 2009). During treatment, avoid injecting into the direction of the upper eyelid if volume replacement at this level is not necessary.
Usually, volume requirement for the whole forehead is high especially when there is severe volume loss and depressions (Figs. 6.4 and 6.5). Medium- to high-viscosity HA products are used with cannulas for forehead and glabella reshape to improve contour and volume loss. In elderly patients with severe dermal and subcutaneous atrophy, lower-viscosity HA products are preferred.
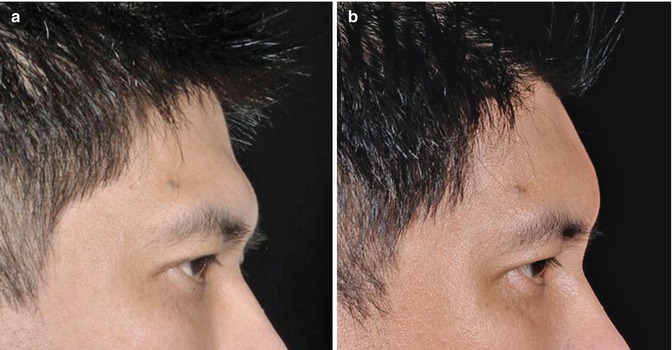
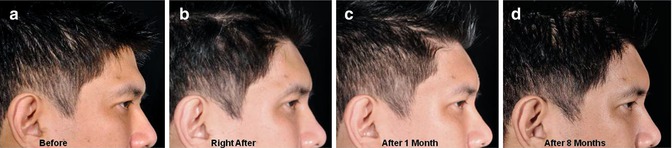
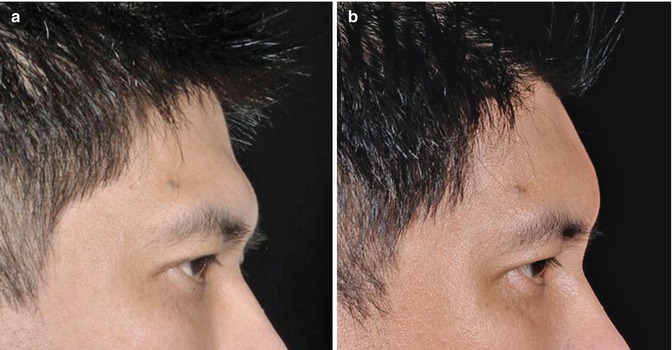
Fig. 6.4
(a) In Asians, due to structural aspect, concavity in the upper forehead and convexity at the glabella level may be found and is considered undesirable. (b) The patient was submitted to an injection of 4 ml Juvéderm Voluma with a single entry point in each eyebrow between the supratrochlear and supraorbital foramina. A 21G non-flexible blunt cannula was used. The after photo was taken after 8 months
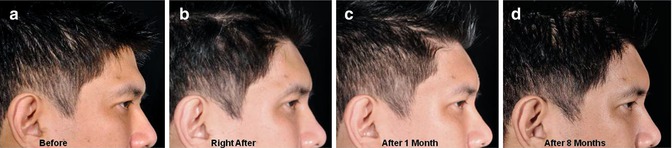
Fig. 6.5
(a–d) Before, immediately after, as well as 1 and 8 months after the forehead reshaping. Note: the consistency of the results over an 8-month period
6.1.5 Tips, Tricks and Key Points
Do’s
Before injecting a filler treating forehead and glabellar folds, it is recommendable to pretreat this area with BoNT-A. The combination of BoNT-A and an injectable filler usually leads to a better overall result. BoNT-A should be injected approximately 2 weeks before the filler, although both procedures can be performed at the same time in this area.
Any remaining superficial lines above the eyebrow after treatment of the upper third with BoNT-A can easily be corrected with a biodegradable filler of low viscosity. Correction with small dosages of BoNT-A is also possible. However, this might carry a small risk of brow ptosis if a significant part of the M. frontalis is affected.
Don’ts
Do not inject too much volume into the glabella and forehead area. In rare cases focal necrosis is reported after the treatment of the glabella and/or the forehead.
Key Points
The glabella is a combination therapy area. BoNT-A therapy should go first.
Do not inject too much volume into the glabella and forehead area. A little less may be preferable to decrease the risk of an unwanted arterial occlusion or extravascular compression.
6.2 Temples
6.2.1 Introduction
Thus far the temples are not frequently requested for treatment. However, when treating the whole face, this area should not be forgotten as it may impact the overall expression of the patient, e.g., the combination of full cheeks and hollow temples may not be aesthetically wanted. Furthermore, treatment of the temporal area may improve eyebrow positioning (see below) and thereby add further improvement to the upper face.
6.2.2 Anatomy
Lateral to the forehead region lies the temporal area. It is located above the zygomatic arch, limited by the temporal crest or linea temporalis (the junction of the frontal, temporal, and parietal bones) and laterally by the hairline. Below the skin and subcutaneous tissue, there are three fascial layers within the temporal region, comprising the superficial temporal fascia (or temporoparietal fascia), which is strongly attached to the subcutaneous tissue, and the superficial and deep layers of the deep temporal fascia attached to the bony floor. The trigeminal nerve supplies the sensory innervation of the temporal region. The temporal branch of the facial nerve passes posterior to the middle aspect of the zygomatic arch, where it lies quite superficially beneath the subcutaneous fat. The superficial temporal artery and vein are also found in the subcutaneous layer in the temporal area.
6.2.3 Patient Evaluation and Selection
Ideally, the temporal area should be slightly convex. With aging, it becomes straight, then concave. The concavity progresses from mild to moderate, then severe and very severe with a skeletonized appearance of zygomatic arch. The higher the volume loss, the higher volume replacement is required. A total amount of 0.5 ml of HA-based volumizer is enough for mild/moderate cases (Fig. 6.6) and an average of 1–2 ml per side in severe cases, and in very severe volume loss, a total of 4 ml of an HA-based volumizer may be required. A treatment of the temporal area may also have a beneficial effect on the lateral eyebrows. Some patients will present lateral eyebrow lifting only with injection into the temporal area.


Fig. 6.6
(a) Volume loss and concave aspect at the temporal area down to the projection of the zygomatic arch before treatment. (b) After injection of 0.5 ml of Juvéderm Voluma per side, a convex aspect was obtained
6.2.4 Technique
Volume replacement at the temporal area may be carried out with needles or cannulas. Products may be placed deep down to the bone and/or subcutaneously. After marking the area of volume loss and identifying the superficial temporal artery (may be visible or may identifiable by its pulse) and the veins, the filler can be injected very safely by needle. The needle should be inserted perpendicular to the skin penetrating the epidermis, dermis, subcutaneous, superficial temporal fascia, temporal muscle, and deep temporal fascia up to the bone. The periosteum should not be scratched to avoid pain. After aspiration to rule out vascular injection, the filler/volumizer may be delivered safely. Advise the patient that (specifically with deep injections) a slight pressure at the temple level may be felt especially during mastication in the first posttreatment day. The disadvantage of this approach is more volume usage compared to the subcutaneous approach. The subcutaneous approach is the second possibility. As needles may lead to bruising and/or intravascular injections, cannulas are encouraged. However, specifically patients with severe subcutaneous atrophy may present irregularities of skin surface after subcutaneous filling with either needles or blunt cannulas.
6.2.5 Complications
With anatomical landmarks marked before, the injection itself is a very safe procedure performing deep temple volume replacement by needle. With the subcutaneous approach, bruising and surface irregularities may be found more commonly. As for the glabella and the nasolabial area also come cases of arterial occlusion have been reported for this area.
6.2.6 Tips, Tricks and Key Points
Most patients are not aware of volume loss at the temporal area. Therefore, the treating physician may suggest this area when designing the treatment plan.
Do’s
Remember that temporal volume replacement may be accompanied by lateral eyebrow elevation.
The use of blunt microcannulas is encouraged using the subcutaneous approach for temporal elevation.
Don’ts
Do not forget to assess and point out the volume loss in the temporal area in your patients. The sooner it is corrected, the lower the volume requirement will be.
Key Points
Temple volume replacement has become more effective since the introduction of HA-based volumizers. We are able not only to correct the sunken aspect but also to lift the lateral aspect of the eyebrow. It is an important ally to BoNT-A treatments for the upper third.
6.3 Eyebrow
6.3.1 Introduction
One of the most important aspects of beauty concerns the position of the eyebrows. It has been established that “well-demarcated eyebrows should arch slightly at the junction of the medial two-thirds and lateral one-third of the face.” Variations of color and texture of the hair contribute significantly to the overall perception of the image. However, it is the volume and mass at this level that determine the uniqueness of beauty. Eyebrow dimensions vary widely on an individual and ethnic basis. Eyebrow hair in the medial one-third is full and tends to sweep upward and laterally. In the middle one-third, hair direction is more horizontal and lateral; in the lateral one-third it points downward. It should be noted that normal eyebrow position differs from men to women, and this has to be taken into account when proper correction of undesired aspects of the eyebrows is considered.
The eyebrows not only frame the upward arc of the orbit but express emotions such as anger, frustration, and uncertainty. Any negative aspect concerning the eyebrow symmetry, position, and fullness influences the overall aesthetic balance of the face. Eyebrow position will change with age, as gravity and loss of soft-tissue support result in ptosis, thereby creating a tired and sad look. Eyebrow ptosis leads to lateral hooding of eyelids. The resulting skin excess influences the crow’s feet lines. Hyperactivity of the frontalis muscle is an attempt to correct malposition of the eyebrow and results in transverse lines in the forehead.
Rejuvenation of the upper face may be accomplished using surgical and nonsurgical techniques. Nonsurgical techniques include ablative methods, BoNT-A, and fillers. The surgical approach includes the temporal lift, the endoscopic brow lift, and the coronal lift. Some of the surgical techniques targeting upper-third rejuvenation present certain limitations. Depending on the chosen technique, there may be no effect on glabellar and forehead lines or those in the middle and medium part of the eyebrow. Therefore, other methods, such as fillers and BoNT-A, are mandatory for a complete improvement.
6.3.2 Anatomy
The forehead and eyebrow positions are dependent on the frontal bone, the supraorbital rims, and the zygoma. The action of the frontalis, corrugator, and procerus muscles also influence their position. The underlying bone structure, rather than the soft tissues, can be responsible for aesthetic challenges. The contour of the orbital bone and its prominence, which can be targeted by fillers, is very important for the eyebrow position. The eyebrow is an important demarcation line dividing the upper and the mid-third of the face.
Understanding the eyebrow shape and its position with respect to the supraorbital rim is essential for promoting good results. The eyebrows should be 5–6 cm below the hairline. The medial portion of the eyebrow should lie on a perpendicular line that crosses the lateral portion of the ala nasi and rest around 1 cm above the inner canthus of the eye. The lateral eyebrow ends at an oblique line drawn from the alar base through the lateral canthus. The medial and lateral end of the eyebrow lies at the same horizontal level. In women, the eyebrow should lie above the supraorbital rim and in an arch shape with its highest point at the level of the lateral limbus of the eye at approximately the junction of the medial two-thirds and the lateral third of the eyebrow. In men, the arch must be smaller and must lie slightly lower at the supraorbital rim than in women. It also tends to be heavier in men than in women (Fig. 6.7).
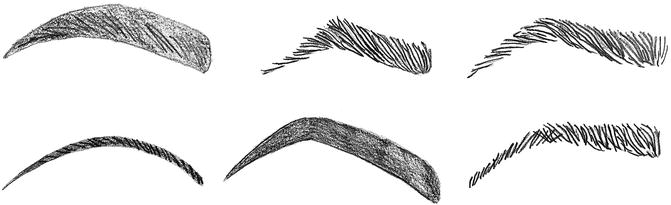
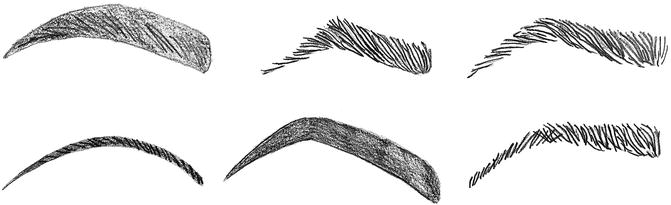
Fig. 6.7
Examples of different eyebrow shapes
6.3.3 Patient Evaluation and Selection
The initial consultation should include a physical evaluation and provision of education about the benefits that fillers may bring to brow reshaping. Patients should understand that it is not a surgical procedure. What fillers may promote is basically a mild volumetric augmentation of the lateral orbital roof and an elevation of the eyebrows in the range of millimeters (Fig. 6.8). Other aspects of the upper third such as hyperkinetic forehead and glabellar lines and the desire to have a major lifting of the eyebrows should be treated with BoNT-A or with selective endoscopic muscle transection. The patient should be evaluated for eyebrow position and mobility, eyelid function, and the presence of skin excess and eye bags. Pretreatment planning should include photographic documentation and a clear explanation of the final result.
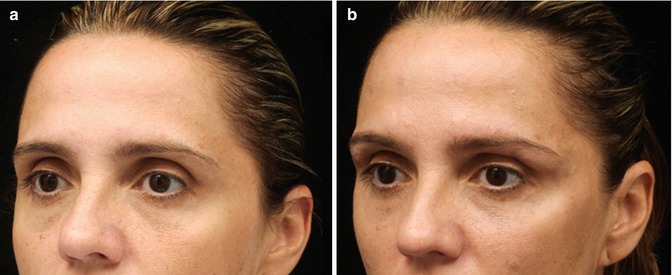
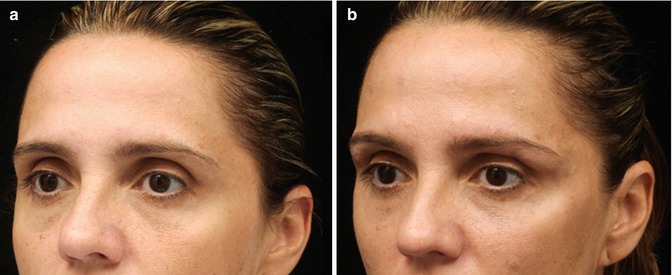
Fig. 6.8
(a, b) Patient before and after injection of 0.8 ml of Juvéderm Ultra Plus along the eyebrow per side and upper eyelid volume replacement with 0.8 ml of the same product per side both with a 21G blunt cannula. Note the projection of the upper lateral aspect of the orbit
Some clinical situations make treatment with fillers difficult or are contraindicated. Severe or moderate ptosis of the eyebrows cannot be improved with fillers because of the inherent limitations of the procedure. The best results are those with symmetric mild ptosis of the eyebrows and thin skin. In these cases, the skin tends to have more mobility for both expansion and elevation. Mild upper eyelid skin excess can be improved in selected cases.
Eyebrow position is one of the common areas for asymmetry. It is quite difficult to find someone with eyebrows that are same shaped and positioned. Therefore, any asymmetry, which is quite common in middle-aged women, must be thoroughly documented before injection. Please note that most patients will present lateral eyebrow lifting only with injection at the temporal level.
6.3.4 Technique
Eyebrow elevation usually does not require local infiltration or nerve blocking prior to injection of the filler. Only topical or no anesthetic at all is usually required for this procedure. With the proper technique, this procedure may be considered quite painless.
After examining the patient, the requirement for medial, central, or lateral elevation must be evaluated. Before starting the injection, it is advisable to stretch up the eyebrow with the finger to verify the mobility of the medial, central, and lateral part of the eyebrow. When major expansion is desired, the entire eyebrow should be injected. In this case, the use of blunt cannula (21, 25, or 27 gauge) may minimize bruising.
If only lateral elevation is desired, a small quantity of the product (0.2 ml) is needed for the lateral part of the eyebrow and is usually performed with needles (Fig. 6.9). Mild differences in positions may be achieved by varying the quantity of the product injected.


Fig. 6.9
In lateral eyebrow lifting, a small quantity of the product may be enough for the lateral upper part of the orbital roof
Although the vast majority of fillers are designed for dermal injections, biodegradable products can be injected into all layers beneath the eyebrow for a better impression of the filler. The filler should be injected onto the periosteum, into the muscle, and subdermally, especially when volumizers are used to improve eyebrow contour and projection. The injection must be soft, and touching the periosteum (which would cause pain) should be avoided. While injecting, it is advisable to stretch the eyebrow and place the thumb on the upper eyelid to avoid migration of the product down this area (Fig. 6.10).


Fig. 6.10
Pinching the eyebrow with the fingers is helpful both to avoid migration of the product down to the upper eyelid. Furthermore, it might decrease pain
After injecting the entire eyebrow or into a specific area, it is advisable to compress the eyebrow for a few seconds to avoid bleeding and keep the product at the proper site. Bleeding is generally light and only minor edema usually occurs. Ice bags are put in place immediately after the procedure. Micro-tapes may be placed onto the site for 2 days to help maintain the eyebrow shape and to reduce edema and migration of the product down to the upper eyelid if we are treating restless patients. However, for the vast majority of patients, no tape is needed. Posttreatment pain is usually minimal and the use of any medication is rare. Patient’s satisfaction is usually good if the limitations of the results have been understood. When fillers/volumizers are combined with BoNT-A treatment, the results tend to be longer lasting and more gratifying.
6.3.5 Complications
Bleeding at the injection site is rare and may cause local and upper eyelid ecchymosis. Proper delicate injection avoiding blood vessels may control bleeding. Immediate compression is advisable in these cases. Local pain and discomfort during injection is probably the result of touching the periosteum with the needle.
Edema after injection is quite common and should be explained to the patient beforehand. Surface irregularities result from irregular placement of the fillers. Asymmetry can be corrected with complementary injections of fillers.
The most feared complication is migration of the filler down to the upper eyelid. Using the proper technique and injecting only small quantities of the required product can avoid this. Other complications, such as those in association with surgical procedures (e.g., numbness, paresis, scars, alopecia, and nerve damage), do not occur in treatment with fillers.
6.3.6 Tips, Tricks and Key Points
Fillers injected into the eyebrow may be easily combined with BoNT-A in the upper part of the face. This will improve the eyebrow position, especially in its upper lateral part. Care should be taken to avoid migration down to the skin of the upper eyelid.
Do’s
Do remember that temporal volume replacement may lift the tail of the eyebrow in selected cases.
Key Points
Eyebrow lifting is crucial for facial rejuvenation. When low positioning of eyebrows are associated with volume loss in the temporal area, the latter should be treated first to provide support for the lateral aspect of the eyebrow.
6.4 Epicanthal Fold and Sunken Upper Eyelid
The following two indications are advanced indications. The indication of the epicanthal fold applies almost exclusively to Asian patients. The sunken upper eyelid is an indication that applies for all ethnic groups.
6.4.1 Epicanthal Fold
Epicanthal fold, epicanthus, or simply eye fold are names for a skin fold of the upper eyelid covering the inner corner (medial canthus) of the eye. One of the primary facial features often closely associated with epicanthal folds is the nasal bridge. Indeed a lower-based nose bridge is more likely to cause epicanthal folds, and a higher-based nose bridge is less likely to do so. There are various factors influencing whether someone has epicanthal folds, including geographical ancestry, age, and certain medical conditions. Epicanthal folds are sometimes found as a congenital abnormality, e.g., in patients with Down’s syndrome, the nasal bridge does not mature. Epicanthoplasty is the eye surgery to remove the epicanthal folds. It can be a challenging procedure because the epicanthal folds overlay the lacrimal canaliculi (tear drainage canals). Epicanthoplasty may leave visible postsurgical scar lines. A common corrective technique involves using a Z-plasty. The use of HA-based injectables with cannulas may be helpful to address epicanthal folds. This can be achieved by advancing the supraorbital ridge, the medial aspect of the orbit, and the nose. With this intervention the features can be improved without surgery. An office-based procedure with no time off may meet patients’ expectations that are not inclined for surgical corrections (Figs. 6.11, 6.12, 6.13, 6.14, 6.15, and 6.16).
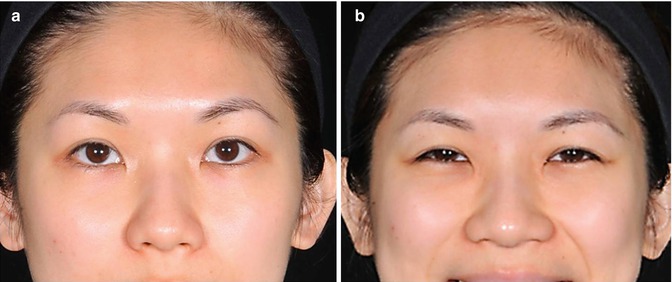
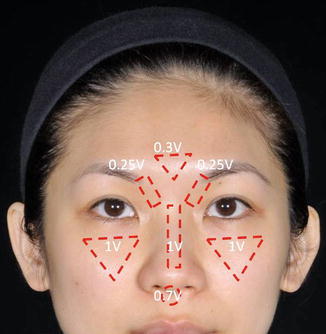
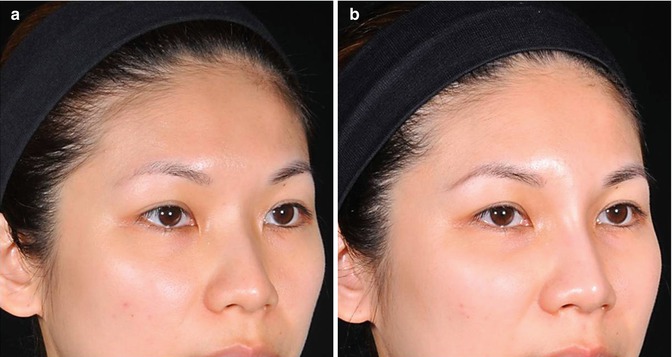
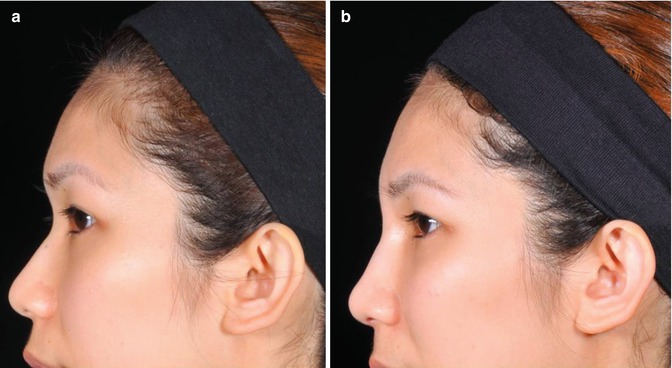
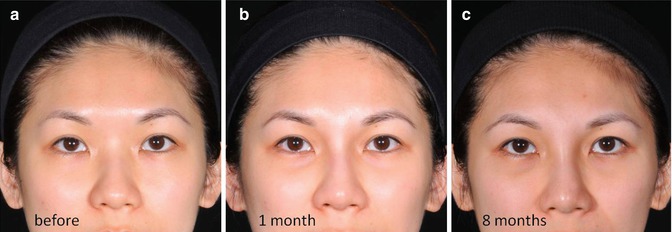

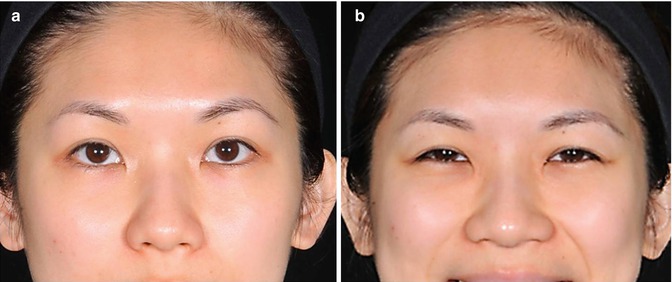
Fig. 6.11
(a) Epicanthal fold at rest. (b) Epicanthal fold on animation
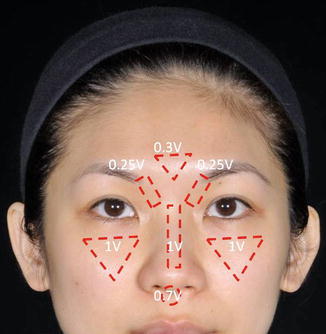
Fig. 6.12
Description of the areas and the quantity of Juvéderm Voluma injected with a 21G blunt cannula: glabella (0.3 ml), supramedial orbit (0.25 ml), nose (1.0 ml), anterior nasal spine (0.7 ml), and cheekbone (1.0 ml)
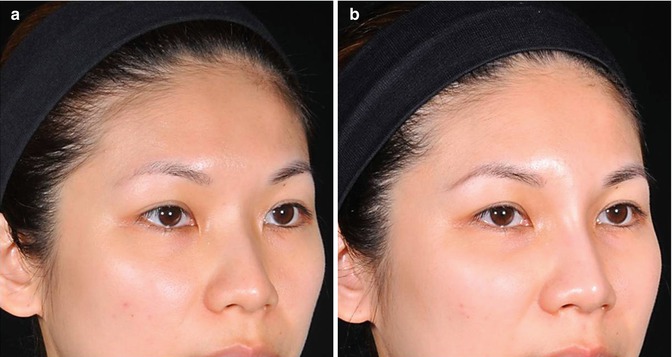
Fig. 6.13
(a) Sunken frontonasal angle and epicanthal fold. (b) After the augmentation of the glabella and nasal bridge, an improvement of the epicanthal fold can be seen
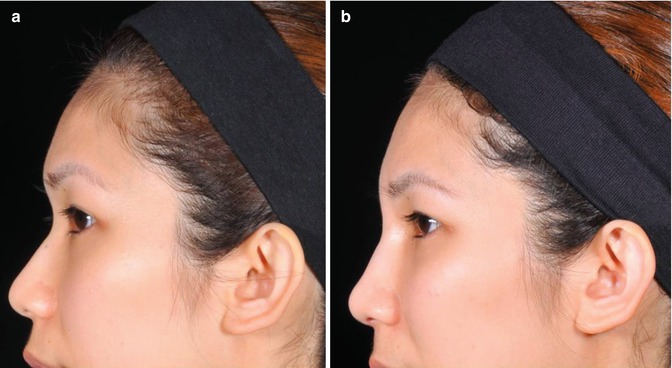
Fig. 6.14
(a, b) Profile view of the same patient: before and after augmentation
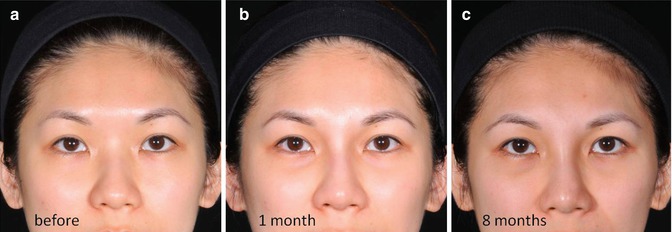
Fig. 6.15
(a–c) Frontal view of the same patient, before, 1 month, and 8 months after treatment

Fig. 6.16
(a–c) Observe the projection of the nose, the medial aspect of the upper part of the orbit, and the evolution of the epicanthal fold
6.4.2 Sunken Upper Eyelid
When we are young the upper eyelid is full and there are only a few millimeters of the upper lid showing. There is no shadow of the upper lid sulcus (see also Sect. 6.1). During aging the upper lid deflates, there is skin excess and folding where fullness was, and the shadow of the upper lid sulcus appears. The fold of the upper lid skin often droops and may reach the lash line and hide completely the upper lid. This status is an indication for aesthetic rejuve-nation.
The treatment of the sunken upper eyelid with HA fillers should only be performed by experienced injectors that have already succeeded with the treatment of complex tear troughs. Persistent edema and mechanical impairment of the upper eyelid excursion may be found if inappropriate technique is performed. Serious risk of vascular injuries may happen if sharp needles are used. The use of blunt cannulas, gentle technique, and low volume is advisable to avoid complications. If proper technique is used, the result may be amazing and much better than fat grafting (Figs. 6.17 and 6.18).
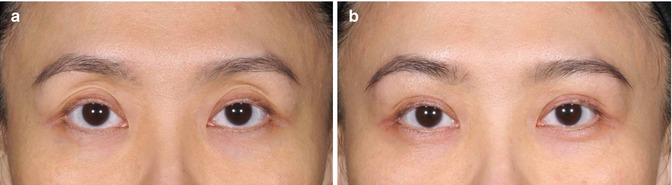
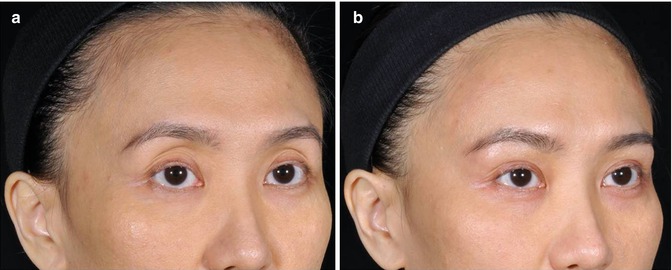
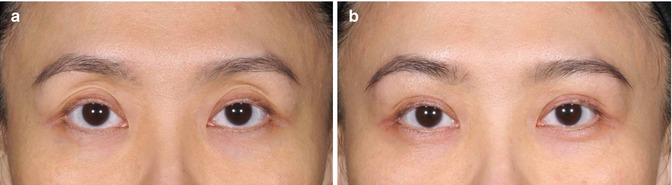
Fig. 6.17
(a) Frontal view: presence of sunken upper eyelid with excessive palpebral show. (b) The patient was submitted to an injection with a 21G cannula. A total amount of 0.45 ml of Juvéderm Ultra Plus was injected into the right side and 0.35 ml into the left side without any complications
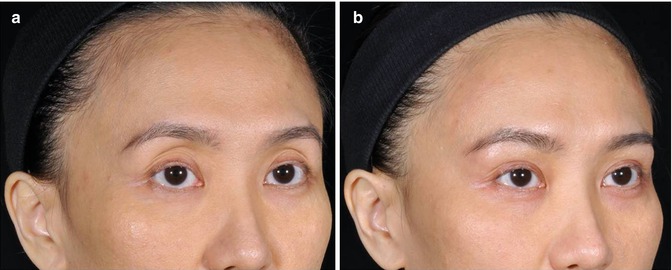
Fig. 6.18
(a) Oblique view: distracting appearance of the upper eyelid. That was patient’s main complaint. (b) After the treatment, a more attractive look was achieved
6.4.3 Tips, Tricks and Key Points
These are tricky indications. Both of them should be restricted to advanced users.
Key Points
We would recommend approaching these indications only after a specific training.
For the sunken upper eyelid, only HA fillers are recommended as in case of overcorrection or edema hyaluronidase might be easily used for correction.
6.5 Infraorbital Hollow, Tear Trough, Cheekbones, and Cheek Reshaping
6.5.1 Introduction
The midface specifically malar projection and full cheeks are important hallmarks of facial beauty and youthful appearance. Therefore, it is important to remember which signs mark a youthful appearance. In youth, the lower eyelid starts at the tarsal insertion and flows in a smooth convexity all the way down to the nasolabial fold and buccal region. The lid-cheek junction is smooth and short, and observing a youthful midface, there is no distinction between the lower eyelid and the cheek.
Volume loss in these areas is a very important landmark and so is the increase of shadows (Pessa 2000). In the lower eyelid, the loss of orbital volume may cause the infraorbital hollow and create a sharp distinction line or shadow that separates the lower eyelid from the cheek. The same loss of orbital volume may reveal the underlying orbital fat provoking eye bags (Lambros 2002). At the cheek level, the anterior view determines the volume loss creating the midface depression. Cheek ptosis with a depression parallel to the nasolabial fold and the face and the presence of the malar mound are important aging signs that are placed in the midface.
HA volumizers have dramatically changed the approach to the mid-third of the face. In the upper mid-cheek and upper lateral cheek area (cheekbone level), volume deficiencies are mostly corrected by the injection of volumizers at this level. Whenever a patient presents infraorbital hollow, tear trough, mid-cheek deficiency, and prominent nasolabial fold, always start by restoring volume at the cheekbone level which will usually lead to an improvement of the infraorbital hollow and the nasolabial fold.
6.5.2 Anatomy
The middle third of the face encompasses the area between the eyebrows and the base of the nose. The inferior third reaches from the nasal base to the menton. The ideal location of the cheekbone prominence is 10 mm lateral and 15 mm inferior to the lateral canthus. Deficits at this level are the result of maxillary elongation and are usually accompanied by a lack of midface projection. The cheek is framed superiorly by the malar complex and inferiorly by the mandible. The size and the shape of the cheeks are determined by the parotid gland, the musculature (mostly the m. masseter), and the buccal fat.
Any midface analysis must include the infraorbital, the tear-trough area, and the submalar triangle (Tobias and Binder 1994). Tear-trough deformities become visible in cases of infraorbital rim depression. The submalar triangle is an inverted triangular area of midfacial depression and is limited superiorly by the prominence of the zygomatic, medially by the nasolabial fold, and laterally by the body of the masseter muscle.
The SMAS comprises the superficial fascia and envelopes the majority of the midfacial musculature. The superficial fat to the SMAS is dense in the cheek, the nasolabial fold, and jowls. The superficial malar fat pad is divided into the cheek portion and the jowl portion. The deep fat is dense in the anterior and the middle cheek. The deep components of the malar fat pad may be encountered between the facial muscles. The buccal fat pad of Bichat is anterior to the masseter and lies deeper to the deep fascia at the buccal level.
The suborbicularis oculi fat ( SOOF) is situated over the lower portion of the zygomatic body and beneath the muscles. It is separated from the periorbital fat by the thin orbital and the malar septum. The presence of malar bags may result from the ptosis of the SOOF.
In the cheek area, the buccinator muscle arises posteriorly from the pterygomandibular raphe. The buccinator muscle is localized deep to the buccal fat pad and extends anteriorly to attach the orbicularis oris. The masseter has a superficial and a deep part. The superficial part arises from the lower border of the anterior two-thirds of the zygomatic arch, and the deep part originates from the inner surface of the posterior third. It inserts the entire lateral ramus of the mandible. Its function is to elevate the mandible.
The malar prominence area has large musculocutaneous perforators. Just lateral to the nasolabial groove, there is a concentration of fatty tissue, the so-called malar fat pad. The facial nerve branches and the parotid duct are deep to the SMAS and superficial to the masseter and buccal fat pad. The zygomatical and buccal branches of the facial nerve become more superficial in the medial cheek (Hamra 1992). The infraorbital nerve is located deeply, along the bony midface. It is responsible for the sensitivity of the cheek and the lip.
As the aging process progresses, ptosis and pseudoherniation of the SOOF and the orbital fat pads occur. Malar bags result from the ptosis of the SOOF and occur below the level of the orbital rim. Loss of the midfacial cheek support causes accumulation of anterior and inferior cheek fat and loss of the lateral and superior cheek fat. This change of anatomy results in deep nasolabial folds, multiple folds in the cheek (while smiling), and a hollowness of the submalar area. The descendent vector will also produce a skeletonized appearance of the cheekbones.
6.5.3 Patient Evaluation and Selection
The use of fillers for reshaping the midface area must obey specific rules: the best results are obtained in patients with good midfacial fullness but insufficient malar projection and with minor malar and submalar deficiencies. It is also a good option for young patients with a good malar bone structure who complain of early onset of flatness in the midface.
Patients with extreme malar deformities and a severe submalar recess are not good candidates for fillers. Conventional malar implants must be considered. Patients with a deficient midface present a narrow nose with a shallow dorsum and a sunken and thin upper lip. The treatment of choice is usually maxillary advancement, and there is generally a 0.5:1 ratio of soft tissue to bony movement. Fillers and specifically the volumizers may also be helpful for complementing soft-tissue advancement.
Balancing the midface in selected cases may promote nice and natural results without the need of surgical procedures with their accompanying postoperative period with ecchymosis and edema.
The skin of the cheeks may show considerable elastosis. Patients with thin skin are in general also suitable for this procedure. Elastotic skin, however, may be difficult to treat. For the forehead area, for example, multiple sessions with a low-viscosity hyaluronic acid may be useful to increase its consistency. Alternatively (see Chap. 9) other interventions as fractionated lasers, peels might be used to improve the texture of the skin.
6.5.4 Tear Trough and Infraorbital Area
The term nasojugal groove was used to describe the concavity at the border of the eyelid and the cheek medially and was named as tear trough later (Flowers 1993; Loeb 1993). It refers to the medial one-third of the infraorbital hollow and may be the first early concavity at the lid-cheek junction in early aging. It is found at the inferior orbital rim down to the hemi-pupillary line. Depending on ethnicity, a trough may be seen in youth in many individuals, and it is its depth or true indentation that leads to a distracting appearance. The tear-trough deformity may be defined as the concavity at the junction of the thin eyelid skin above and the thicker and different nasal and cheek skin below, with attenuated subcutaneous tissue overlying the maxillary bone. The skin in the area of the concavity is indeed of different quality, texture, and color. Hyperpigmentation or full transparency may be found in the skin over the tear trough. Volume loss can be present laterally in more advanced aging, at or just below the orbital rim. At this level, the retaining ligaments are thicker and less distensible. In some individuals, the concavity in the groove is often associated with orbital fat herniation superiorly in the lower lid fat compartments, accentuating its appearance (Fig. 6.19). The orbicularis oculi muscle has a direct attachment to the inferior orbital rim from the anterior lacrimal crest to the medial limbus or approximately one-third of the orbital rim length. Laterally, bone attachment to the bone is given by the orbicularis retaining ligaments which may vary in length, then decreases laterally until these ligaments merge with the lateral orbital thickening in the lateral canthal region. The levator labii superioris originates just below the orbicularis oculi muscle attachment to the medial orbital rim (Muzaffar et al. 2002).


Fig. 6.19
Presence of prominent nasojugal fold, tear trough, and palpebro-malar sulcus. Observe the malar mound and the projection of the orbicularis oculi retaining ligament
As there is scant subcutaneous tissue between the skin and the orbicularis muscle in this area, the tear-trough skin is attached direct to the orbital rim. The cause of the tear-trough deformity may include volume loss, orbital fat herniation, and skin laxity in different degrees of severity among patients.
Mild tear-trough deformities (e.g., infraorbital rim depression) are a good indication for fillers. The presence of fillers along the infraorbital rim may improve the suborbital groove. This is considered an advanced area for injectors, and complications are not rare, especially in the hands of inexperienced users who tend to use too much volume or inappropriate fillers. Minimizing adverse events is of utmost importance here.
It is important to highlight that much of tear-trough deformities can be effectively treated only by mid-cheek volume replacement. Aging process provokes elongation of the lid-cheek junction, and shortening of the lower lid height can be also obtained only by volumizing the cheekbones (Figs. 6.20 and 6.21).
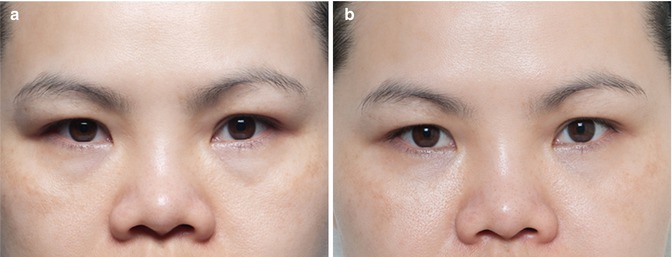
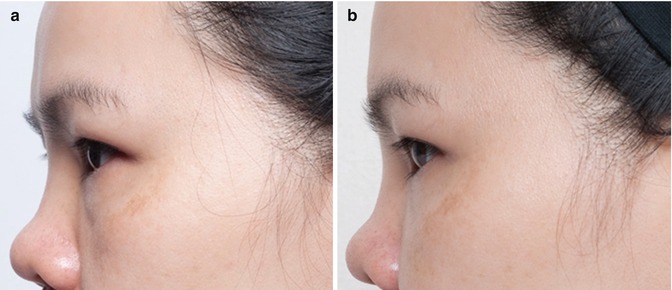
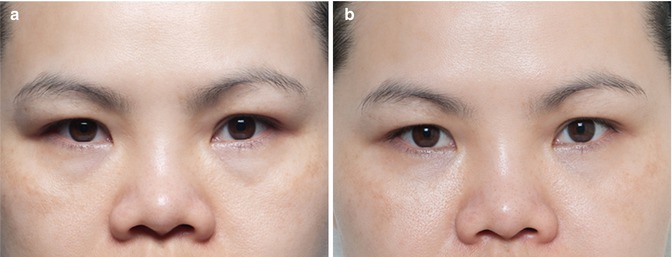
Fig. 6.20
(a) Presence of tired look with elongated lid-cheek junction. (b) After the injection of 0.5 ml of Juvéderm Voluma per side, the transition between the lower eyelid and cheeks was softened. A direct injection into the tear trough was not performed
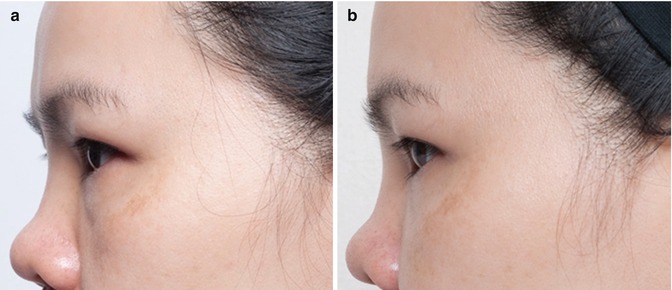
Fig. 6.21
(a) On the profile view, it is evident that the volume loss in the mid-cheek was the cause of the elongated lid-cheek junction and tired look. (b) After the treatment, there is no evidence of a noticeable transition line between both structures
If a hydrophilic product such as HA is to be used at this level, undercorrection is advisable to avoid prolonged edema. Ideally, low-viscosity products are to be injected at the tear-trough level due to the thin aspect of the skin. However, other products as low-viscosity HA preparations may be injected in this area too – provided they are injected deeply.
Treatment in the infraorbital area starts with the marking (Fig. 6.22). The patient should be in upward position and should bend the head forward with “chin down, eyes up.” This position enables more accurate distinction of the elongated lid-cheek junction and accentuates the tear-trough deformity and volume loss along the infraorbital and cheekbones areas. The inferior orbital rim is usually higher, so any intraorbit injection is avoided if the upper limit of this marked line is respected. Usually only topical anesthetics and/or ice packs are used. Infraorbital and zygomatic facial nerves block might be needed if working with larger cannulas and with HA products without lidocaine.


Fig. 6.22
Skin demarcation is very useful for treating the tear-trough deformity. After demarcation follows the injection. Care should be taken not to produce excessive ecchymosis
Volume replacement in the infraorbital and cheekbone areas can be performed with either needles or blunt cannulas. Deep injections touching the bone at the infraorbital foramen level must be avoided to high risks of complications. Both bolus and retrograde techniques can be performed at the cheekbone level. The accurate choice will depend on the degree of volume loss and bone projection. Flat bone and universal volume loss at this level is better treated with retrograde or small bolus injection to avoid irregularities. High volume concentrated in a single point could lead to difficulty in molding the product and higher risk for unwanted effects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








