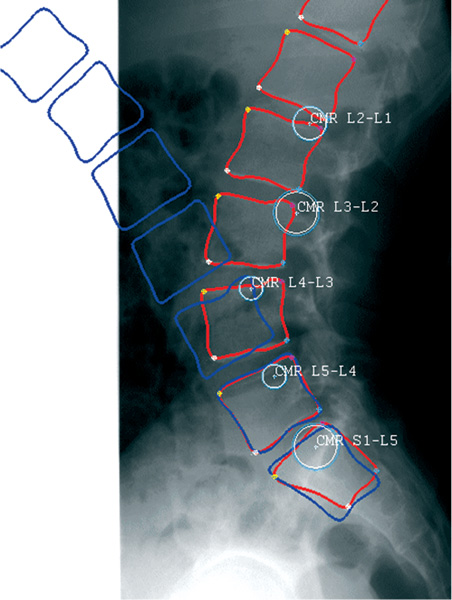
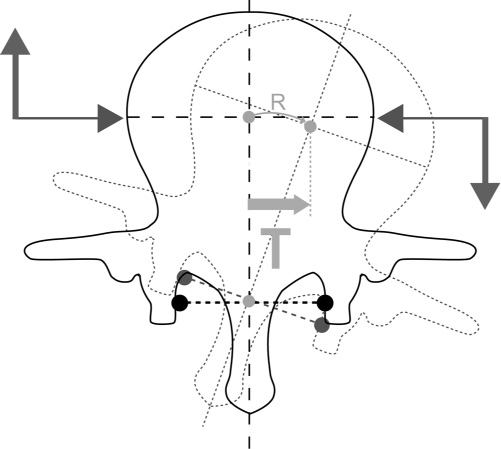
25 Spine surgery is in relative infancy within the scope of orthopedics. As with the hip and the knee, spine surgery started with arthrodeses and osteotomies, which were immobilized by plasters and then by osteosyntheses. Today, hip and knee prostheses, or other articulations, achieve considerable excellence and the functional results speak for themselves. But while there are only two hips and two knees, there are multiple vertebral levels. Each level is triple with two posterior articulations and one anterior articulation: the disk. Spinal mobility is concentrated on the lordotic segments (cervical and lumbar). Working segments—crucial to quality of life—worsen with time with the loss of the anatomical ratios, lordosis, and movement. The replacement of the disk is logical from the point of view of reconstructive surgery. The first disk prostheses appeared in the 1950s and ’60s. They were made of cement or steel balls placed inside the disk.1,2 Today we find nucleus prostheses, such as the PDN (prosthetic disk nucleus; Raymedica, Inc., Minneapolis, MN), serpentine of Husson, hydrogel injection,3,4 and total disk prostheses (TDPs).5 The TDPs are semiconstrained or nonconstrained depending on whether their center of rotation is fixed or mobile. They adopt the same principles: superior and inferior metal plates with or without an intermediate polyethylene element. Since 1987, the date of the first implantation of the Charité prosthesis (DePuy Spine, Raynham, MA),6 more than 14,000 total disk prostheses have been implanted. The prosthesis Mobidisc (LDR Spine, Austin, TX) is a nonconstrained total disk prosthesis with a mobile polyethylene core. There are three axes and 6 degrees of freedom in a spinal mobile segment7: flexion-extension (horizontal frontal axis), lateral bending (horizontal sagittal axis), and rotation (vertical axis). These movements are controlled by “guides” (articular facets) and “brakes” (ligaments, capsules, and muscles).8 Nearly 80% of the load supported by the spine9 is on the anterior part of the disk which, due to its elastic distortion/deformation, adapts itself to the movement. The “wear-and-tear” effect will degrade the disk, which will be at the very origin of lumbago, even of lumbago-sciatica. Spinal movements are characterized by the center of rotation. The centers of rotation of the movement in flexion-extension are determined by geometrical construction based upon the shape and spatial position of the posterior articular processes.10,11 This center of rotation is located one third posterior to the intervertebral space and underneath the surface of the superior plate of the inferior vertebra, a location that was confirmed by models in finite element analysis12 and through the use of software applied to radiographs in flexion and extension (Fig. 25–1). It is, in fact, a median center of rotation. This median center of rotation is resultant of the instantaneous centers of rotation (ICR). These ICR are defined as being, at a given moment T, the distribution of speeds of the points of a mobile plan compared with a fixed plane. The ICR is the I point where speeds are canceled. The ICR and their spatial evolution make it possible to know and to measure the mechanical solicitations at a precise spot of the studied solid or two solids, one compared with the other. The center of rotation of the flexion-extension movement is thus not single and moves within a physiological area. The ICR in lateral flexion and torsion are still different. Pure rotation around the axis of the vertebral body is impossible because of the anatomical shape of the posterior articular facets. This rotation is thus a torsion12 resulting from a frontal translation on a circle, the center of which is at the level of the spinal processes and of a slight rotation on the axis of the vertebral body (Fig. 25–2). This physiological movement varies from 3 to 6 degrees depending on the age and the morphotype.8 The majority of the physiological movements are combined movements and the ICR are very variable. At the time of growth, one can think that there is harmony between the development of the disk and posterior articular facets with adapted ICR. With the aging process and the degeneration of facets and disk, instability moves the ICR away from the physiological areas. The articular facets especially will undergo abnormal strain in torsion.8 Under the influence of the proprioceptive nervous system, the evolution proceeds toward the progressive expulsion of the degenerated disk and the transfer of the loads behind on the articular facets by loss of height and by putting lordosis on the intervertebral space (evolution in the three stages of Kirkaldy-Willis and Farfan).13,14 The evolution of the ICR is thus closely related to the function and dysfunction of the intervertebral mobile segment. Figure 25–1 Spine view: flexion-extension. Figure 25–2 Rotation of the intervertebral segment. A total disk prosthesis must restore the intervertebral height and standard mobility with adapted ICR. The current semiconstrained prostheses have an average posterior and inferior center of rotation corresponding to the Median Center of Rotation (MCR) in flexion-extension. The absence of lateral movement does not favor a physiological rotation of the intervertebral segment. Nonconstrained prostheses respect displacements of the ICR, particularly in rotation. The combined movements are favored and the wear of the posterior articulations and of the prosthesis is reduced.5
The Mobidisc Prosthesis
 Biomechanics of the Spine and of the Intervertebral Space (Junghanns)
Biomechanics of the Spine and of the Intervertebral Space (Junghanns)
 Operative Technique: Anterior Approach
Operative Technique: Anterior Approach
Biomechanics of the Spine and of the Intervertebral Space (Junghanns)
The Mobidisc Prosthesis
Principles
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 The Mobidisc Prosthesis
The Mobidisc Prosthesis Clinical Results
Clinical Results Conclusion
Conclusion