CHAPTER 21 The Fully Coated Cementless Femoral Stem
KEY POINTS
 Preoperative templating with high-quality radiographs is crucial to provide the surgeon with the following information: planned leg length correction, the level of femoral neck osteotomy, and the anticipated implant size based on both the diaphyseal stem diameter and metaphyseal triangular segment size.
Preoperative templating with high-quality radiographs is crucial to provide the surgeon with the following information: planned leg length correction, the level of femoral neck osteotomy, and the anticipated implant size based on both the diaphyseal stem diameter and metaphyseal triangular segment size. A properly placed starting pilot hole is essential and is typically best positioned slightly anterior to the piriformis fossa. The hole may need enlargement to prevent deflection for the canal reamer, whose direction must be controlled by the femoral diaphysis and not by the proximal structure (e.g., the greater trochanter or femoral neck).
A properly placed starting pilot hole is essential and is typically best positioned slightly anterior to the piriformis fossa. The hole may need enlargement to prevent deflection for the canal reamer, whose direction must be controlled by the femoral diaphysis and not by the proximal structure (e.g., the greater trochanter or femoral neck). Reaming should continue until the last reamer achieves a minimum of 5 cm cortical contact—“scratch fit.” This can be estimated by inserting a reamer of the same diameter as the prosthesis and measuring the distance of the exposed reamer body above the starting pilot hole.
Reaming should continue until the last reamer achieves a minimum of 5 cm cortical contact—“scratch fit.” This can be estimated by inserting a reamer of the same diameter as the prosthesis and measuring the distance of the exposed reamer body above the starting pilot hole. During insertion, the stem should move more distally with each mallet impaction. Typically as the stem advances, the same impaction intensity will move the stem less during the final 2 cm compared with the first few centimeters. The insertion of the prosthesis should take between 50 and 80 mallet blows, with more blows in a patient with good quality cortical bone. During insertion, the surgeon should be aware of a sudden increase in prosthesis advancement with impaction of the same intensity.
During insertion, the stem should move more distally with each mallet impaction. Typically as the stem advances, the same impaction intensity will move the stem less during the final 2 cm compared with the first few centimeters. The insertion of the prosthesis should take between 50 and 80 mallet blows, with more blows in a patient with good quality cortical bone. During insertion, the surgeon should be aware of a sudden increase in prosthesis advancement with impaction of the same intensity. Femoral fracture during stem insertion can be in the proximal metaphyseal area or distal in the diaphysis. Nondisplaced fractures are treated with protected weight bearing. Displaced proximal fractures can be effectively treated with cerclage cable. Although rarely encountered, a displaced distal fracture would require a formal open reduction with plate and cable internal fixation.
Femoral fracture during stem insertion can be in the proximal metaphyseal area or distal in the diaphysis. Nondisplaced fractures are treated with protected weight bearing. Displaced proximal fractures can be effectively treated with cerclage cable. Although rarely encountered, a displaced distal fracture would require a formal open reduction with plate and cable internal fixation.Extensively porous coated femoral components for total hip arthroplasty have been widely used for nearly three decades.1 The success of the implant depends largely on osteointegration between the host bone and the prosthesis. This “biologic fixation” of the prosthesis utilizing bone ingrowth can be achieved consistently and has resulted in excellent long-term clinical results.2
The porous coated prosthesis provides a favorable substrate for bone ingrowth. When the porous surface is intimately apposed to host bone, the bone reliably grows into the porous scaffold and interdigitates with the prosthetic surface, thus providing an enduring fixation.3 Theoretically, an implant with a fully porous coating offers the greatest area for bony apposition, particularly in cortical bone, and the best possibility for bone ingrowth compared with partially or proximally porous coated implants.
The evolutionary development of the cementless femoral implants dates back to the 1960s with the introduction of the macroporous surface implants in Euorpe.4 These implants were designed as an alternative to the Charnley styled implants. Drs. Charles Engh and Emmett Lunsford pioneered an extensively porous coated implant, the anatomic medullary locking (AML) hip system (Depuy, Warsaw, IN), for elective hip arthroplasty in 1977.5 By 1983, after obtaining approval from the U.S. Food and Drug Administration, the AML system became available for general use. The initial AML had a circumferential porous coating around its cylindrical, nontapered stem covering over four fifths of its surface. In the 1990s, the porous coating was extended over the entire length of the AML stem. It has been more than 25 years since the initial introduction of the AML, and, currently, virtually every major implant company has some type of a fully porous coated, cementless femoral component available for hip arthroplasty. The recommendations and techniques described in this chapter reflect the experience at the our institution using the AML family of implants. These include AML, Prodigy, and Solution hip prostheses.
INDICATIONS AND CONTRAINDICATIONS
The porous coated hip prosthesis was initially developed for younger, more active patients undergoing total hip arthroplasty. The basic premise for a successful porous coated implant is the presence of an adequate femoral bony stability to provide initial mechanical support and healthy bone quality to allow for osteointegration, leading to bony ingrowth.1 Extensively porous coated implants have been successfully used in diverse patient populations. At 10 years’ follow-up, there is more than 96% and 98% survival in active patients younger than 50 years old and more inactive elderly patients older than 65 years old, respectively.6,7 An extensively porous coated femoral component is indicated for patients undergoing a total or partial hip replacement for the treatment of osteoarthritis, osteonecrosis, inflammatory arthritis, post-traumatic arthritis, and displaced intracapsular proximal femur fractures.
Although it is not the focus of this chapter to address revision total hip arthroplasty, it is important to mention the versatility of the extensively porous coated stem in the treatment of failed femoral component in revision surgery.8 Bone quality is often compromised in the proximal femur in revision total hip arthroplasty. An extensively porous coated prosthesis can obtain a durable diaphyseal fixation, bypassing the poor quality proximal bone.
PREOPERATIVE PLANNING
The goal of the preoperative planning is to prepare the surgeon to adequately address the various intraoperative variables to achieve an optimal outcome. Adequate preoperative templating is crucial to the success of any hip replacement; this is particularly true of the porous coated prosthesis. Placing the cementless prosthesis is more technically demanding than placing the cemented prosthesis because it is more difficult to compensate interpositionally an abnormal bony anatomy without cement.9 Templating allows the surgeon to better estimate the factors that can best restore the patient’s hip mechanics, such as leg length, offset, and hip center. The surgeons must preoperatively determine the level of the femoral neck cut and then select the prosthesis that would best fill the femoral canal at this predetermined level.
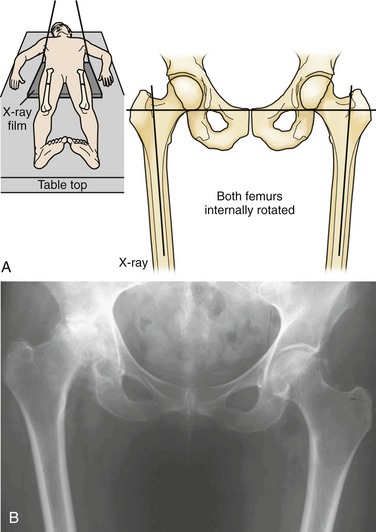
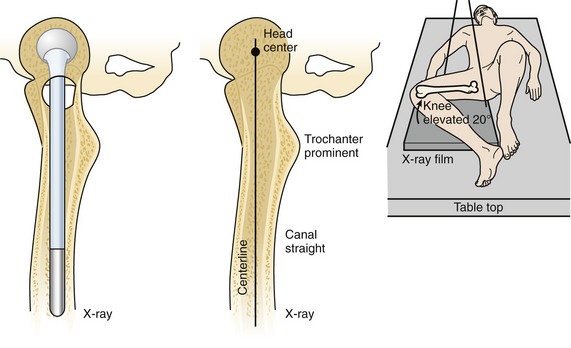
High-quality radiographs taken with specific criteria must be used for templating. Typically, two views are necessary: the anteroposterior pelvic view and the true lateral view of the proximal femur. The anteroposterior radiograph should include both the acetabulum and at least 8 inches of proximal femur. The x-ray beam and the cassette are lowered to ensure that the center of the x-ray beam is centered slightly below the pubic symphysis. The ideal position of the patient and its schematic radiographic appearance are shown in Figure 21-1A. The femur is internally rotated 20 degrees to obtain a true profile of the normally anteverted femoral neck. This is the view in which the true femoral neck-shaft angle and femoral offset can be accurately measured and thus provides the correct profile to superimpose the prosthesis template (see Fig. 21-1B). In many instances, the stiff arthritic hip cannot be rotated to achieve this view. The contralateral hip may be used if it is nondiseased, or the patient may be placed in the prone position to rotate the pelvis and the arthritic hip together to obtain the appropriate internally rotated view. The technique to take a lateral radiograph of the femur is shown in Figure 21-2. The lateral radiograph should be taken in such that the hip, knee, and ankle are all in contact with the x-ray table. This view allows for the estimation of the anteroposterior dimension of the femur, the amount of the femur bowing, and the extent of the femoral head anteversion.