27 Preparation and Surgical Approach Diskectomy and End Plate Preparation Distraction (Disk Height Restoration) Establishing Proper Implant Size Repositioning (or Extracting) the FlexiCore Closure and Postoperative Care Degenerative disk disease (DDD) represents a significant morbidity in our health care system. Back pain, the clinical manifestation of DDD, results in major disability, time lost from work, and a significant effect on quality of life for the patient. It is estimated that a significant episode of back pain will affect 80% of the U.S. population at least once in their lifetime.1 More than $50 billion in annual health care expenditures for both direct and indirect costs will be spent in the treatment of back pain. This unfortunately makes back pain a significant problem for society. Treatment strategies for back pain initially begin with an exhaustive course of nonoperative therapy. Most back pain can be treated with rest, medication, and physical therapy. When this has failed, surgical treatment is indicated. Spine surgeons generally agree that surgical treatment for DDD typically involves some type of fusion of the lumbar spine. The rationale for fusion is that immobilizing the degenerated segment can eliminate painful motion of that joint while also eliminating the disk as a pain generator. Historically, posterolateral fusion was the most common technique used to fuse the lumbar spine, but as our clinical skills and technology have improved, newer techniques have been developed. Today DDD can be treated with lumbar interbody fusion, posterior spinal fusion, or a combination of the two procedures. As newer techniques have been developed our success at achieving radiological fusion has increased. Unfortunately our improvement in clinical results has not equaled the radiological results.2,3 Mobility of the spine is a result of interconnected motion between each intervertebral level. Fusing one segment of the spine results in increased load across other levels. This leads to adjacent level degeneration, which can result in further morbidity. In addition there could be an alteration in sagittal balance due to graft collapse, and stress shielding/disuse osteoporosis.3–6 For this reason spine surgeons have begun to investigate and use newer techniques to treat DDD while still restoring motion across the segment. The total disk replacement (TDR) represents a new generation of devices that can preserve motion in the spine while removing the painful degenerative disk. Currently there are four TDRs that are undergoing investigational trials in the United States. The FlexiCore Lumbar Intervertebral Disc Replacement (Stryker Spine, Allendale, NJ) represents a metal-on-metal device. The FlexiCore disk is a cobalt-chromium-molybdenum highly polished ball and socket metal-on-metal prosthesis. The device is designed as a tension-bearing device that prevents separation and potential dislocation of the superior and inferior baseplates. There is also a rotational stop in the device that prevents the facets from being overloaded. A unique design feature of the FlexiCore disk is the central dome shape of the baseplate. This shape enables the prosthesis to match the normal end plate concavity of the vertebral body. This helps both to facilitate bony fixation and to optimally locate the device’s center of rotation slightly posterior to the spinal midline. The domes are flanked by short spikes to establish initial fixation and are coated with a titanium plasma spray to encourage long-term fixation. The two baseplates are joined by a central ball and socket joint that establishes the device’s center of rotation. This provides a range of motion that does not limit the natural range of motion of the intervertebral segment. In addition, it prevents any translation of the baseplates that would mimic subluxation. The device provides 15 degrees of flexion-extension and lateral bending. This exceeds the natural range of motion of an intervertebral segment but does not lead to the baseplates sliding anteriorly-posteriorly, or laterally, relative to one another. There is an internal rotational stop that is designed to minimize pathological facet loading by preventing axial rotation beyond 5 degrees, which is just outside the natural range of motion. The bearing surfaces of the ball and socket components are highly polished cobalt-chromium. This has been shown in the joint replacement literature to have a lower coefficient of friction and generates a decreased amount of wear debris compared with bearing surfaces that include polyethylene. Further, metal-on-metal bearing surfaces are not subject to the “creep” seen in metal-on-polyethylene interfaces.7,8 The ball of the joint is captured in the socket during the manufacturing process before delivery to the surgeon. This prevents the device from separating under tension loads and permits it to be held, manipulated, and inserted into the disk space as a single unit. This, combined with the implantation instrumentation, not only permits the device to be inserted from multiple anterior angles but also minimizes the implantation misalignments and other errors associated with multipiece assembly and implantation. Some repositioning is also possible even after the device is seated in the disk space. The FlexiCore intervertebral disk is currently under investigation in the United States. It is indicated for implantation in patients with DDD who are between ages 18 and 60. Other indications include: The FlexiCore intervertebral disk is contraindicated for study in patients having: The components of the FlexiCore intervertebral disk implantation system include: Figure 27–1 Distraction spacers. Figure 27–2 Static distractors.
The FlexiCore Disk
 Description of System Components
Description of System Components
FlexiCore Disk Design
Indications
 Back pain of diskogenic origin with degeneration of a single disk (L1–S1)
Back pain of diskogenic origin with degeneration of a single disk (L1–S1)
 Axial back pain greater than leg/radicular pain
Axial back pain greater than leg/radicular pain
 Radiographic evidence of decreased disk height by 2 mm compared with adjacent (cranial) disk height and/or1: Translational instability (≥ 3 mm translation)2; angular instability (5 degrees)
Radiographic evidence of decreased disk height by 2 mm compared with adjacent (cranial) disk height and/or1: Translational instability (≥ 3 mm translation)2; angular instability (5 degrees)
 A preoperative visual analog scale (VAS) score for back pain of at least 40/100
A preoperative visual analog scale (VAS) score for back pain of at least 40/100
 A preoperative Oswestry score of at least 40/100
A preoperative Oswestry score of at least 40/100
 Failed conservative treatment for back pain for a minimum of 6 months
Failed conservative treatment for back pain for a minimum of 6 months
Contraindications
 DDD at more than one level
DDD at more than one level
 Previous lumbar fusion or bilateral open decompressive procedures
Previous lumbar fusion or bilateral open decompressive procedures
 Compromised vertebral body structure
Compromised vertebral body structure
 Degenerative spondylolisthesis/retrolisthesis > 25%
Degenerative spondylolisthesis/retrolisthesis > 25%
 Spondylolysis with or without spondylolisthesis
Spondylolysis with or without spondylolisthesis
 Lumbar scoliosis > 15 degrees
Lumbar scoliosis > 15 degrees
 Facet joint disease or degeneration
Facet joint disease or degeneration
 Poor bone quality
Poor bone quality
 Medications that interfere with bone/tissue healing
Medications that interfere with bone/tissue healing
 Infection, hepatitis, rheumatoid arthritis, autoimmune diseases, or malignancy
Infection, hepatitis, rheumatoid arthritis, autoimmune diseases, or malignancy
 Obesity, pregnancy, or allergy to implant materials
Obesity, pregnancy, or allergy to implant materials
Description of System Components
 Distraction spacers (Fig. 27–1)
Distraction spacers (Fig. 27–1)
 Static distractors (Fig. 27–2)
Static distractors (Fig. 27–2)
 Static distractor handle (Fig. 27–3)
Static distractor handle (Fig. 27–3)
 Dynamic distractor (Fig. 27–4)
Dynamic distractor (Fig. 27–4)
 Inserter/impactor (Fig. 27–5A–C)
Inserter/impactor (Fig. 27–5A–C)
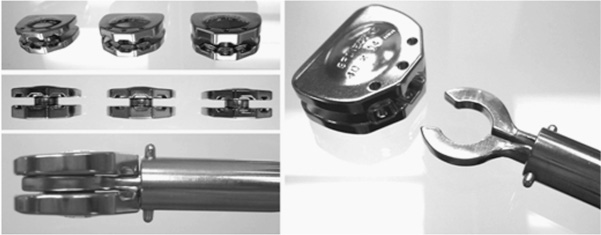
 Repositioner/extractor (Fig. 27–6A,B)
Repositioner/extractor (Fig. 27–6A,B)
 Leveling tool (Fig. 27–7)
Leveling tool (Fig. 27–7)
 Wedge-ramp distractor (Fig. 27–8)
Wedge-ramp distractor (Fig. 27–8)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 FlexiCore Disk Design
FlexiCore Disk Design Indications
Indications Contraindications
Contraindications Operative Techniques
Operative Techniques Complications
Complications Conclusion
Conclusion Caution
Caution