CHAPTER 15 The Dual-Incision Approach
The era of so-called minimally invasive total hip arthroplasty was catapulted into the spotlight with the introduction of the two-incision technique described by Duwelius and colleagues.1 Initial enthusiasm and aggressive marketing of the procedure led many surgeons to utilize the technique; however, subsequent reports from surgeons at other institutions sounded a warning that the technique, as initially described, could lead to potentially higher complication rates.2,3 One of the most frequently reported complications was femoral fracture. Bal and coworkers reported that a change in stem design led to a lower rate of this particular complication in a subgroup of patients.3 The dual-incision technique as described here is a two-incision technique that utilizes a mediolateral wedge femoral component design, along with appropriate patient positioning and surgical approach, to minimize complications and allow the performance of a relatively muscle-sparing surgical approach. I currently utilize computer surgical navigation in all my dual-incision hip procedures. The addition of surgical navigation addresses concerns regarding possible component malpositioning that may occur when procedures are performed with more limited visualization.4,5 The description that follows is of the surgical technique itself and does discuss the integration of surgical navigation. I suggest that interested surgeons first become familiar with surgical navigation in the setting of standard total hip arthroplasty before attempting to integrate it with less invasive surgical techniques.
PREOPERATIVE PLANNING
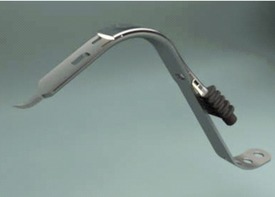
In the operating room, appropriate instrumentation to allow adequate exposure and visualization is necessary. Specialized retractors are necessary for acetabular exposure and to protect the soft tissues during the approach. Lighted retractors have been found to be very useful (Fig. 15-1). Planning ahead to have well-trained surgical assistance throughout the surgery is absolutely necessary. Having two assistants available during acetabular exposure and preparation is optimal.
TECHNIQUE
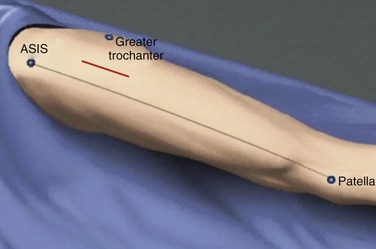
Landmarks are identified for placement of the anterior incision. The skin incision is made 2 to 3 cm lateral to a line connecting the lateral border of the patella and the anterior superior iliac spine. The skin incision starts cephalad at about the level of the tip of the greater trochanter and extends distally as far as needed, typically around 5 to 9 cm (Fig. 15-2). The incision is over the belly of the tensor fasciae latae muscle. Dissection is carried down to the fascia of the tensor fasciae latae, and blunt finger dissection is carried out medially to enter the interval between the tensor fasciae latae and the sartorius. Once the interval has been entered by blunt dissection, the surgeon’s fingertip can confirm palpation of the femoral head and neck by rotating the leg. A bolster is placed under the leg to maintain an abducted hip position, and retractors are placed above and below the femoral neck, exposing the hip capsule (Fig. 15-3). Once retractors are in place and the hip capsule is exposed, care must be taken to achieve meticulous hemostasis. Running along the inferior margin of the wound are the recurrent branches of the circumflex artery and veins. Dissection to find these vessels and cauterize them is absolutely critical. If these vessels are not identified and ligated or cauterized, bleeding throughout the remainder of the case will hinder visualization and may lead to postoperative hematoma formation (Fig. 15-4). A partial anterior and superior capsulectomy is performed to allow visualization of the femoral head and neck. Adequate superior capsulectomy is also necessary to allow later preparation of the proximal femur through the second incision. A double osteotomy of the femoral neck is performed to remove a segment of neck and allow easier extraction of the femoral head. A corkscrew is placed in the femoral head, and it is levered out of the acetabulum (Fig. 15-5).