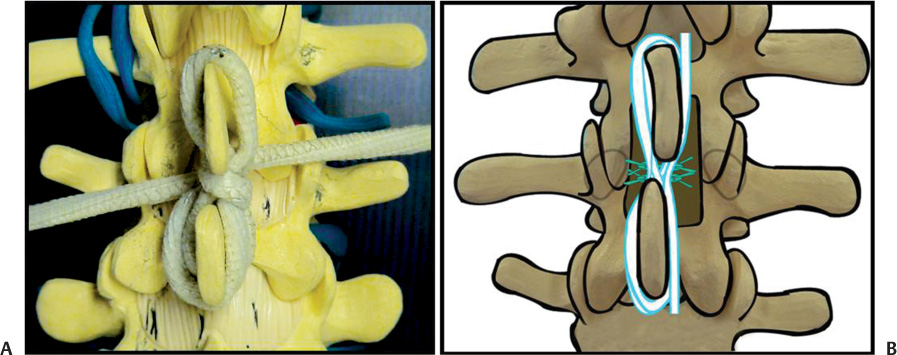
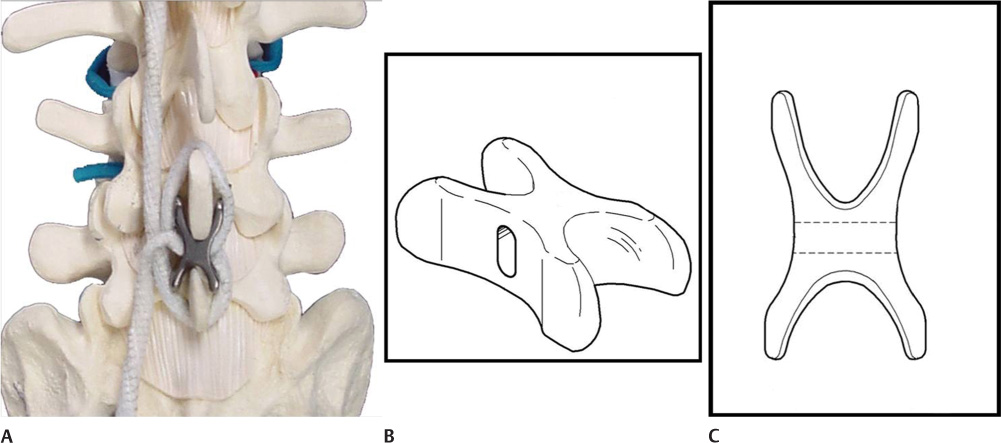
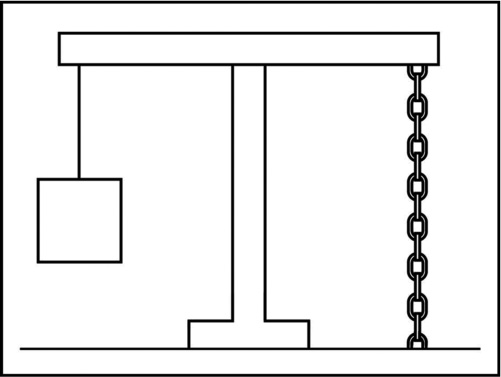
36 Artificial Ligament with Metal Interspinous Locker Biomechanics of the Tension Band System Fixing the Artificial Ligament and Interspinous Locker Decompressive Laminotomy and Interspinous Locker Degenerative Spondylolisthesis and the Tension Band System Combination of Tension Band System and Other Soft Stabilization The spine can be considered a flexible, multicurved column. It has four major interrelated and somewhat disparate functions: to support, provide mobility, protect, and control. Mobility is required for the physical tasks of daily living, which tend to compromise the spine structures. The basic functional unit of the spine is termed the motion segment. The motions of the individual segments contribute to the total motion of the lumbar spine. A motion segment, also called a functional spinal unit, consists of two adjacent vertebrae with their shared intervertebral disk and facet joints. The spine can be unstable. Instability may be a very specific diagnosis. Myriad biomechanical and clinical definitions have been developed to describe spinal instability.1,2 At the most simplistic level, instability is a lack of stability, referring to decreased stiffness of the motion segment, excessive motion, abnormal motion, or, in some circumstances, simply painful motion. Instability of a motion segment is often called segmental instability. These descriptors are implicit in the definition given by the American Academy of Orthopaedic Surgeons, which states: Segmental instability is an abnormal response to applied loads, characterized by motion in motion segments beyond normal constraints.3 Segmental instability seems to be the cause of most of the problems that affect the vertebral column, whether they are fractures, fracture-dislocations, infections, tumors, spondylolisthesis, kyphoscoliosis, degenerative instability, or iatrogenic instability after decompressive surgery.4 The goals of surgical management of segmental instability include stabilization of the spine, prevention of neurological injury, and relief of pain. Spinal fusion is the current gold standard in surgical management for lumbar spinal instability.5–9 However, fusion with or without instrumentation has been shown to cause complications, such as damage to the spinal root caused by the pedicle screw, instrumentation failure, loss of lumbar curvature, new lesion development just above the area of fusion, and a higher incidence of wound infection.10–14 In addition, the surgical procedure itself is complex and expensive. Motion preserving techniques will offer the opportunity to achieve intersegmental stabilization coupled with retained intersegmental mobility, a goal that is unattainable in fusion surgery. Dynamic posterior stabilization technologies have been reported in clinical studies since the 1980s.15 Current dynamic posterior stabilization technologies fall into two main categories: interspinous process spacers and pedicle screw–based systems. The tension band system is an interspinous process spacer. There are two tension band systems: interspinous ligamentoplasty, originally documented by Senegas et al16 and the artificial ligament with metal interspinous locker, developed by Lee et al. This chapter reviews the biomechanics of the tension band system, its indications, and surgical techniques used in tension band fixation. The tension band system is composed of an artificial ligament and interspinous spacer. Descriptions of the two tension band systems are described in the following sections. The artificial ligament (Bio–Tex Ligament Artificial de Renfort Vertebral, Textile Hi-Tec, Montpelier, France) is composed of polyethylene terephthalate (polyester) and barium-platinum radiopaque silicone. It is 40 cm in length and 5 mm in diameter. Its extremities are prolonged with a traction thread and a needle. The artificial ligament is soaked in antibiotics mixed with saline before use. Both upper and lower spinous processes are surrounded with an artificial ligament as a figure eight at the base of each spinous process. The waist of the figure eight is sutured several times just inferior to the upper spinous process and just superior to the lower spinous process with traction of the artificial ligament. This multiply sutured waist acts as an interspinous spacer (Fig. 36–1). Figure 36–1 (A) Both upper and lower spinous processes are surrounded with an artificial ligament as a figure eight at the base of each spinous process. (B) The waist of the figure eight is sutured several times just inferior to the upper spinous process and just superior to the lower spinous process with traction of the artificial ligament. This multiply sutured waist acts as an interspinous spacer. This system combines artificial ligament with a metal locker. The interspinous locker is made of titanium. It is composed of four U-shaped flanges, a central hole, and a clip. The flanges enclose the spinous process, restricting the migration of the locker. The flanges also prevent the lateral translation of the locker. The artificial ligament passes through the central hole and surrounds both the upper and the lower spinous process as a figure eight. The clip tightens the artificial ligament to prevent loosening (Fig. 36–2). The spinal column complex consists of ventrally located vertebral bodies and intervening intervertebral disks that collectively assume most of the axial load–bearing responsibilities of the spine. The pedicle connects the ventral and dorsal components of each spinal segment. The laminae provide the roof for the spinal canal; the facet joints limit rotation, flexion, extension, lateral bending, and translation. The ligaments provide for and limit torso movement. The ligaments also provide varying degrees of support for the spine.17 The effectiveness of a ligament depends on the moment arm through which it acts.18 Although the interspinous and supraspinatus ligament are not substantial, their attachment to a bone with a relatively long lever arm (spinous process) allows the applications of a significant flexion-resisting force to the spine by virtue of the significant distance between the instant axis of rotation and the point of the attachment of the ligament to the spinous process. Figure 36–2 (A) Artificial ligament and metal interspinous locker. (B,C) The locker is composed of four U-shaped flanges, a central hole, and a clip. Many instability-definition schemes are based on a column concept to quantitate the extent of spinal integrity and to ultimately determine the presence or absence of spinal instability. The three columns of Denis19 are conceptually useful. Denis’s three-column theory, which adds the concept of a middle column to the anterior and posterior columns, allows specific assessment of that component of the spinal column in the region of the neutral axis. The neutral axis is the region of the spinal column about which spinal element distraction or compression does not occur with flexion or extension. Usually, the neutral axis is located in the region of the midposterior aspect of the vertebral body and the intervening disk; that is, the middle column. The principle of the tension band system is borrowed from engineering (Fig. 36–3). If the spinal column is subjected to eccentric loading on the anterior column, we have not only the axial compressive stresses but also additional bending stresses that give rise to further compressive stresses on the anterior column and tensile stresses on the posterior column, which may contribute to the anterior sliding of vertebrae in degenerative conditions. These bending stresses can be neutralized by a chain (the posterior interspinous and supraspinatus ligaments) prestressed to exert a force equal and opposite to the weight. The tension band system can place an artificial ligament and its blocks in the posterior column, maintaining equilibrium when the anterior sliding is present. In some cases, degenerative changes of the intervertebral disk may result in the subsidence of the posterior part of the disk, which causes the posterior sliding of vertebra, referred to as retrolisthesis. In retrolisthesis, a repositioning of facet joints has occurred and the facet joints bear abnormal loading. In the tension band system, an artificial ligament and its blocks in the posterior column can restore segmental alignment and unload the facet joints. Figure 36–3 Tension band principle. The axial load, which gives rise to tensile stress on the opposite side, can be neutralized by a chain. Voydeville et al studied the biomechanics of a similar type of artificial ligament in vitro on six functional human L4–L5 spinal units. They reported on a flexible, soft type of stabilization with artificial ligament–limited flexion-extension, axial rotation, and lateral flexion.20,21 In addition, the artificial ligament corrected the narrowing of the spinal canal and stabilized the motion segment such that the canal remained at the appropriate width.21,22 Papp et al studied the biomechanical effects of a flexible polyester artificial ligament.22
Tension Band System
 Components of Tension Band Systems
Components of Tension Band Systems
 Indications and Contraindications of the Tension Band System
Indications and Contraindications of the Tension Band System
Components of Tension Band Systems
Artificial Ligament
Artificial Ligament with Metal Interspinous Locker
Biomechanics of the Tension Band System
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Surgical Techniques
Surgical Techniques Conclusion
Conclusion