13B “Temporary” Scalp Micropigmentation (Trichopigmentation)
Summary
Keywords: trichopigmentation temporary scalp trichopigmentation scalp micropigmentation hair thinning scar camouflage shaved effect
Key Points
•Temporary scalp trichopigmentation is a safe and effective alternative treatment for camouflaging hair loss and scars in appropriate patients. It can be a standalone procedure or an adjunct to hair transplantation.
•Reversibility is one of the main advantages of this procedure. While some see this as a limitation, proponents feel it is one of its most positive characteristics. Patients are free to decide whether to go on with the treatment or stop it in order to change their look.
•The pigment, tools, and technique were designed specifically for this technique and not adapted from other techniques.
•Trichopigments are fully compliant with the European Union requirements for the production of dyes from intradermal which has the strictest guidelines, banning more than 1,328 substances from being used.
•The pigments used are all smaller (~15 μm), which is key to their absorbability and reversibility. Although the question of nanotoxicology (a new science) has been raised, there is no evidence of the pigments and any disease.
13B.1 Introduction
Temporary scalp trichopigmentation (STP) is an innovative technique of scalp camouflage that creates the illusion of shaved hair on the head with pigment. It is different from standard scalp micropigmentation (SMP) in that it is temporary and designed to fade. Temporary STP was officially introduced to the field of hair restoration during a special session of the 14th Italian Society of Hair Restoration Congress in Capri (May 2010). It was the first time SMP of any type had been demonstrated at a hair transplant conference and it was well received. There was much excitement about its potential use as a “therapeutic” aide that can be added to the treatment plan of patients with hair loss. What followed was the beginning of the rapid spread of this technique among the hair transplant community.
Permanent SMP had been around for about 10 years before the introduction of STP. However, it was not embraced by the hair transplant community during this time, and drew a lot of criticism due to a high incidence of unnatural results, which included color change, migration, and blotchy results.
Temporary STP was developed specifically to address and solve these and other problems caused by the original permanent techniques. A unique pigment was created that was “temporary” and designed to fade over time. Other modifications were made to limit color change, migration, and allergic reaction. Equipment and protocols were designed to address the specific and unique characteristics of the scalp.
It should be mentioned that in recent years, there have been major improvements in the permanent technique of SMP and therefore a renewed interest.1
The debate between supporters of both techniques is aggressive. Looking at all the positive feedback regarding these techniques, it is clear that both solutions can be applied, provided that they are carried in a correct and skillful way. Both have their relative advantages and disadvantages. Physicians should keep an open mind to what each technique can offer a patient and make their recommendations based on the best interest of the patient.
13B.2 The Basic Principle of Temporary Scalp Trichopigmentation
STP pigment undergoes a micronization process that ensures all the particles are less than 15 μm. By injecting a pigment composed solely of particles smaller than 15 μm into the superficial dermis, we allow the macrophages to absorb it until it disappears. Usually, it takes between 1 and 2 years for the pigment to be totally reabsorbed.
However, touch-up treatments can be performed when the dots start to fade to counter reversibility if the patient desires to keep the look. Therefore, patients have the option to keep the look permanently or let it fade. It is this flexibility that proponents feel is one of the main advantages of STP. Patients can experiment with a look but change their mind in the future if they desire. This “expiration date” of the treatment, seen as a limitation by some, has turned out to be a characteristic in many situations. Although patients may be certain they want a specific look when they start the process, they may change their mind at a later date for a number or reasons. They may simply want a more conservative hairline as they age, or perhaps they have had progression of hair loss and the SMP no longer looks good. Patients are free to simply stop the treatment to change their look whenever they want without the need for a laser removal treatment to gain a “normal” appearance.
13B.3 Scalp Trichopigmentation Characteristic
STP pigments are composed solely of different colored metal oxides powders. These include titanium dioxide, which is white, and iron oxides which can be red, black, or yellow. They are mixed together to create a universal brown color, which appears ash-gray (the same color as keratin) when injected below the skin.
The pigments undergo a process of micronization in which they are centrifuged, filtered, and encapsulated. Before this process, the particles are different in shape and size. After the process, we are left with identical size microspheres, whose dimensions are smaller than 15 μm. The filtering ensures that no particles larger than 15 μm are used. This is why the pigments are temporary. Our body’s macrophages will absorb and eliminate foreign particles less than 20 μm. Larger particles become trapped in the dermis. Color change is also limited by this process because all the particles are identical in size and shape and will be absorbed at an identical rate. This prevents a dominant color being left behind, which occurs when pigments are absorbed at different rates, and is one of the causes of color change.
The pigments also encapsulated in a biocompatible silicone-like membrane during this process. This prevents contact with tissue and makes them hypoallergenic.
For many years, the field of tattooing and pigments was fairly unregulated. It was difficult to know what ingredients were in different products or their safety profiles.2,3 This is changing and the European Union is leading the way and having the strictest guidelines having banned over 1,328 substances from being used.
A few theoretical concerns have been raised about STP pigments that should be mentioned for completeness:
•One concern was that the metal in the pigment could possibly interfere with an MRI. There is no evidence this is true.
•Another concern was that the micro-silicone–like encapsulation gets eliminated and does not accumulate in the lymphatic system. There is no evidence this is a problem.
•A final concern was whether or not these pigments constituted nanotherapy and would pose a risk of nanotoxicity, which is a relatively new area of medicine. Much of the information comes from complex studies.4 There is no evidence of any specific problems, but an awareness of the issue is wise as well as early reporting of any advents that occur.
13B.4 Scalp Trichopigmentation Equipment Characteristics
13B.4.1 Micropigmentation Machine
The characteristics of the scalp vary in different areas. For example, the crown is thicker than the parietal area; and scar tissue behaves differently than virgin tissue.
The pigmentation machine developed for STP was designed with specific control buttons and settings (rpms and power) for different locations of the scalp. While these settings can be adjusted, they make the process easier to learn and more consistent. Another modification is a handpiece that limits vibration and hand tremors. This limits skin damage and injury, which in turn limits migrations of pigment.
13B.4.2 Scalp Trichopigmentation Needles
The STP needle is unique in that the inside and outside have different textures. The outside tip is smooth for easy penetration of the skin. The inside wall is rough and designed to hold on to excess pigment, protecting excessive flow of pigment. This allows for controlled deposition of pigment with a consistent amount deposited each time.
Most STP is done with a combination of single- and triple-point needles. Some feel three-point needles should be reserved for a thickening look when going in between hairs and only a single-point needle should be used for the hairline and shaved look.
The STP needles are slightly finer than other brands, enabling slightly smaller and more delicate dots. This is an advantage for creating natural looks, especially in the hairline. When trying to produce a denser look, some prefer a larger needle and there is some controversy as to the best needle size for this with respect to the trade-off of naturalness versus density.
13B.4.3 Depth Guard
The STP handpiece comes with an adjustable depth guard that allows us to accurately adjust the needle depth from 0.2 to 1.5+ mm deep. In STP, the best depth is in the upper dermis, typically between 0.5 and 1.0 mm deep. If it is too deep, it can migrate and if it is too shallow it may have poor retention. The depth changes in different areas of the scalp. Many clinics use a “sense of feel” to allow them to know when they are at the right depth. While this is doable, it takes a lot of skill and experience to get to this point. Many mistakes are made along the way. With the depth guard, it is much easier to learn and be consistent in finding the proper depth. One can also use judgment and feel as they become more skilled.
13B.5 Consultation and Patient Selection
Hair loss is actually a fairly complicated affliction with many causes and a significant psychological effect. Often a multidisciplinary approach using medical, surgical, and aesthetic approaches like SMP is required to achieve the best results. There is a high incidence of body dysmorphic syndrome5,6 with hair loss, and practitioners must be cautious with patients who do not have realistic expectations. If both surgery and STP are going to be performed, the order and timing must be determined and this will vary from case to case. Sometimes, it is best to do SMP first, as it gives the quickest result and often may be temporarily enough to satisfy a patient. In other cases, for example, in scar repair, sometimes it is better to perform the surgery first as it will improve the characteristics of the scar tissue making it more receptacle to STP later. Often, especially with repairs, a significant amount of anxiety over the decision is present. It is often wise to let some time pass before making a final decision so that a more informed and conscious choice can be made. The temporary nature of STP may be a better choice when anxiety and indecision are present.
13B.6 Scalp Trichopigmentation Procedure and Timing
Each area of the scalp can have different thickness, thus making it necessary for the technician to select correct rpms and needle depth. This is especially tricky on scar tissue. In some cases, it is advisable to carry out a test on a small area before treating the whole tissue.
The STP protocol developed by Milena Lardi uses a fairly systematic design protocol to create density and naturalness. During the first session, the technician creates a base of equidistant dots. During all the other sessions, the dots are placed in between the ones done on the first day to complete the treatment. In this manner, the technician decides how to place the dots in order to achieve the desired result focusing on the natural hair density of the patient.
This systematic approach is different from the other approaches that simply look at the treatment areas and use clinical judgment to try and fill in the spaces at a uniform density as close together as possible on the first pass. This less systematic approach can be performed successfully; however, it requires more experience and skill and is intrinsically riskier than the systematic approach.
After 28 days, at the end of a complete cellular turnover, it is possible to evaluate the outcome of the treatment and carry out additional sessions. The number of sessions needed before reaching the desired effect depends on a number of factors, including the type of procedure being done, the area and thickness of scalp being worked on, the patient’s individual immune system, skin regeneration properties, and more. On average, two to four sessions done approximately 1 month apart are needed depending on the case (Fig. 13.1a–d). Experienced technicians can vary the treatment timetable to extend the time between maintenance sessions.
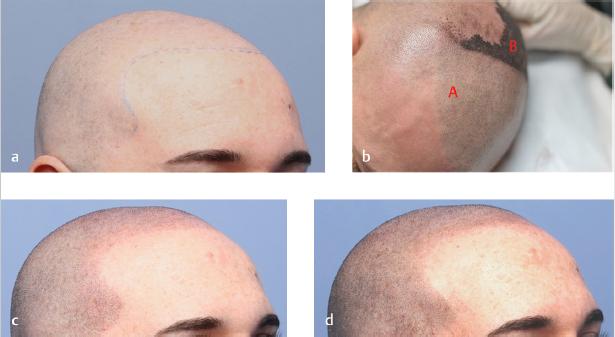
Fig. 13.1 Steps to create a shaved look. (a) Before procedure with hairline drawn in. (b) Halfway through first procedure: Area B shows the systematic first pass pattern of overlapping circles equidistant apart. Area A shows even distribution of dots once area is wiped. (c) Shaved look after first pass is finished. (d) Denser shaved look after second pass is finished.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







