3 Taking a Hard Look: Soft Tissue Augmentation
Summary
As the number of male patients seeking cosmetic enhancements continues to rise, the need to understand the differences and similarities between both genders to tailor techniques most suitable for the male aesthetic patient is crucial for optimal results. In order to avoid feminizing a male face, it is important to appreciate the areas on the face that represent sexual dimorphism. Along with increased awareness of these key facial characteristics, injectors must understand rheological properties of injectable fillers to both preserve and create masculinity of the face, yielding strong and defined borders which are generally perceived as more attractive in men. In this chapter, we cover these principles to better help providers achieve successful outcomes with their male patients.
Keywords: dimorphism symmetry chiseled masculine
3.1 Background
According to the American Society of Plastic Surgeons’ 2017 National Plastic Surgery Statistics, 14.1 million cosmetic procedures were performed, with men making up 1.1 million cases.1 This represents 8% of the market, which has grown significantly (76%) since 2000.1 Soft-tissue fillers are one of the top five nonsurgical, minimally invasive, cosmetic procedures performed on men. In a study of over 52,000 men and women, women outnumbered men by a 9:1 ratio of cosmetic procedures performed. Interestingly, women only outnumbered men by a 2:1 ratio in their interest in cosmetic procedures,2 suggesting that there is an unmet need for the male aesthetic patient. Despite the rising demand of aesthetic procedures for men, there is limited literature available to guide clinicians in understanding treatment preferences of the male aesthetic patient as well as treatment approaches.
In a survey of treatment-naive men interested in cosmetic procedures, men were most motivated to consider injectable procedures “to look good for my age” and “to look more youthful.”3 The most concerning facial areas most likely to be prioritized for treatment were the tear troughs and crow’s feet, highlighting that the periorbital areas are most likely the primary focus of aesthetically oriented men. The least concerning facial areas and least likely to be prioritized for treatment included lip volume and perioral lines. Respectively, this may be due to concerns of feminization and because men are less susceptible to the development of perioral wrinkles due to the inherent larger numbers of skin appendages and thicker skin.4,5,6 The top reasons men would not consider an injectable cosmetic procedure were, in the following order: thinking they did not need it yet, concerns of side effects/safety, concerns about injecting a foreign material into their body, cost, maintenance of procedures, and concerns about not looking natural.3
The survey suggested that many of the barriers to trying aesthetic treatments such as dermal fillers are rooted from a low level of awareness and lack of education about the procedures. As a cosmetic physician, it is crucial to educate the male cosmetic patient, understand their interests and needs, and approach treatments with attention to the unique facial dimorphisms between genders.
Volumetric changes are a key component of male facial aging and the aforementioned areas of concern, and there are numerous options available to revolumize the male face. Poly-L-lactic acid (PLLA) is a biostimulatory nonhyaluronic acid filler that produces a natural look by stimulating collagen production and in the authors’ opinion helps maintain and imitate the architecture of the bone when properly placed.7 PLLA has both rejuvenative and prejuvenative properties, which are ideal for male aesthetic patients concerned with looking “overdone or feminized” or feeling they “do not need it yet.”
To achieve a masculine look, one that is more chiseled, angulated, and squared, the cosmetic physician must choose the appropriate filler products. An understanding of rheological properties of fillers is essential to understanding each fillers personality.8 One of the most highly referenced and used measurement of fillers is G prime (G′). G′ is most often used to describe the fillers’ hardness and ability to cause tissue projection. High-G′ fillers such as calcium hydroxylapatite (CaHA) or hyaluronic acid (HA) when properly placed can correct and enhance masculine features. An exception would be fillers placed in the tear trough or lip region, which require a low-G′ HA filler. Fat transfer presents an autologous option for revolumization that can offer similar variation in characteristics based on harvest and preparation, allowing specific structural properties for use in specific areas. Soft-tissue augmentation with volume is a balance between anatomy and aesthetic goals. With an understanding of facial dimorphism between genders along with age-related changes, the proper placement and volume can be used to achieving a masculine and natural look.
3.2 Facial Dimorphisms
The dimorphic features that characteristically differentiate a man’s face from a woman’s face are a result of the hormonal influences that occur during puberty.9 In an adult male, differences can be seen in the skin, subcutaneous tissue, and bone structure. The epidermis and dermis in men are overall thicker compared to women and are largely due to increased collagen density in men.6 This is likely influenced by androgens since skin collagen density is increased in females with primary cutaneous virilism compared to normal female controls.10 However, men have less facial subcutaneous fat.9
As a generality, excluding ethnic variations, a man’s face is more square shaped compared to the heart-shaped or inverted triangular shape of a woman. When evaluating a male patient, the temple width should ideally line up with the lateral zygoma, which should also line up with the projection of the mandible. Balancing these three areas will help achieve a squared look, which is considered an ideal masculine feature by experts.9
3.3 The Aging Face
Keeping in mind masculine features, changes in bone structure also occur in the aging face, and failure to address these foundational changes may limit the benefits of rejuvenated procedures. Men tend to age more linearly compared to women who undergo greater age-related changes after menopause.11 Bone mineral density studies of the skulls of men and women have shown that both men and women experience a decrease in bone densities, particularly the maxilla and mandible, between young (20–40 years) and middle-aged (41–60 years) individuals.12 Bone resorption also occurs in the orbital apertures, pyriform aperture, maxilla, zygomas, and mandible, and is described in more detail below (Fig. 3.1).
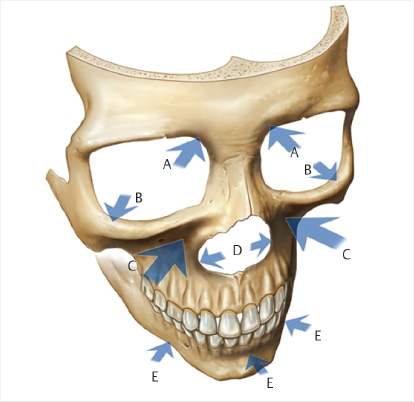
Fig. 3.1 Bone resorption of the human skull with aging. The arrows indicate areas were resorption tends to occur with aging. (A) Superomedial orbital rim. (B) Inferomedial, orbital rim. (C) Maxilla. (D) Pyriform aperture. (E) Mandible.
The orbital aperture increases with age. This is largely due to resorption that tends to occur in the inferolateral and superomedial quadrant of the orbit.13 The midface, formed by the maxilla and the zygoma, undergoes retrusion.14,15,16 Much like the orbital aperture, the pyriform aperture also increases. Resorption occurs in the inferior and lateral walls. Posterior resorption is greatest in the lower pyriform aperture, which is the major supporting structure of the lateral crura and external nasal valves.17 The anterior nasal spine, which supports the columella, also undergoes resorption. These changes manifest as a clinical lengthening of the nose, tip drooping, and a columella and lateral crura displacing posteriorly.18 Supporting this area with supraperiosteal injections in the pyriform fossa with a high-G′ filler can help soften and lift the perinasal and nasolabial folds. PLLA can be used in this area to build collagen and provide supplemental support to the soft tissues acting as a proxy where bone resorption has occurred.7 In dentate men and women, the maxilla and mandible experience resorption changes, despite it traditionally being thought to occur only in nondentulous individuals.19 An accelerating factor may be seen in patients with bruxism, an unconscious clenching and grinding of the teeth.19 The ramus height, mandibular body height, and mandibular body length decrease with age in both genders, whereas the mandibular angle increases with age.20 The increase in mandibular angle is likely due to the combination of decreasing lengths in the ramus body height and mandibular body length. CaHA along the inferior borders of the mandible can help mask these changes by maintaining mandibular proportions.
3.3.1 Upper Third
A major contributing factor to the appearance of aging in the upper one-third of the face is the frontal concavity. Brow ptosis and eventual furrowing of the brows is a result of diminished soft-tissue volume on the forehead, creating projected expressions of anger, sadness, and tiredness. Gender and genetics play a role in the presentation of variations of frontal concavity.22,23,24
The upper third of the face of the bony structures of a woman’s forehead and glabella is more curvilinear and less pronounced. The supraorbital rim of a woman is less noticeable than that of a man. A man has a more oblique forehead, a glabella that is more prominent, and a supraorbital rim that is more pronounced. The pronounced supraorbital rim establishes the position of the male eyebrow, which sits flat along the orbital rim compared to women who have a more arched brow. As a result, women tend to dominate in the upper one-third of the face with higher arched brows and a more open appearance of the eyes.25 Conversely, men dominate in the lower one-third of the face due to pronounced jaw lines, yet also present with lower set eyebrows, bossing brow bones, and less soft-tissue volume in the upper one-third of the face. Due to these combined factors, a pronounced frontal concavity is naturally more prevalent in men. Premature aging in the upper one-third of the face may also be due to genetic differences. Asian and Mestizo ethnicities specifically have deficiency in soft-tissue volume contributing to very flat or even concave frontal projection. Therefore, presence of frontal concavity appears earlier in certain populations, usually by the fourth decade.
Neurotoxins, although excellent for reducing rhytids, when used in a frontalis muscle that is already volume depleted, can lead to an exaggerated aging appearance and worsening of brow and lid ptosis.26 To circumvent this potential undesirable outcome, we hereby describe a technique utilizing a low-viscosity, low-G′ HA filler to volumize frontal concavity.
Anatomy
Understanding the anatomical boundaries and danger zones in the frontal region is of utmost importance when injecting to avoid any complications. Most important is a clear knowledge of nerves and the vascular supply of the area. The main arterial danger zones to be aware of when using this technique include the supratrochlear, supraorbital arteries, and branches of the superficial temporal artery.
The frontal branch of the superficial temporal artery courses superiorly and medially to anastomose with the supratrochlear and supraorbital arteries, which are branches of the ophthalmic artery. Bilaterally, these supply the majority of the frontal region. The glabella is predominantly supplied by small arterial branches from the supratrochlear and supraorbital arteries with limited collateral circulation.7 The veins in the frontal region accompany the arteries and drain to the angular vein and the internal jugular vein. The supratrochlear and supraorbital nerves branch off of the trigeminal nerve and provide sensory innervation to the region (Fig. 3.2).

Fig. 3.2 Injecting in the subgaleal space proves to be safe and effective when doing frontoplasty with injectable fillers.
The anatomical plane of all structures should be taken into consideration before the injection of filler to decrease complications such as vascular compromise. Vascular occlusion can occur by external compression of the blood supply by adjacent filler injection, direct intra-arterial injection of product, and by vascular injury during injection.26,27,28 Symptoms of vascular compromise are blanching of the skin, a progressive dusky color change of the skin, and eventual ulceration with eschar formation. In the glabellar region specifically, vascular occlusion may lead to blindness. Finally, in addition to vessel injury, nerve damage can occur, and may present as discomfort during the injection, headache, neuralgia, and/or paresthesia.
If adverse events are suspected, treatment protocols should be utilized.27,28 Risk of these events can be minimized by careful selection of the injection site, aspiration prior to injection, injecting in the subgaleal space, and continually monitoring for signs and symptoms of vessel occlusion.
Frontoplasty Technique
Always keeping in mind important vascular landmarks (Fig. 3.3a), find the temporal crest as a landmark and demarcate this area. Depending on how wide and deep the frontal concavity of the individual is, mark two to four entry points on each side of the temporal crest (Fig. 3.3b). Prior to injections, the face is cleansed (e.g., hypochlorous acid or chlorhexidine) to promote an aseptic and sterile technique. A 21-gauge needle can be used to create the openings and a 25- or 22-gauge, 2-inch cannula can be used to fill the frontal concavity in the subgaleal plane by lifting the frontalis muscle between the thumb and the forefinger and sliding the cannula into the subgaleal space (Fig. 3.3c). HA can be deposited in a linear retrograde fashion. Using small-gauge cannulas (i.e., 25- or 22-guage cannulas), knowing where the tip of the cannula is at all times, moving at least 1 to 2 mm retrograde before beginning to deposit small aliquots of the product, knowing the trajectory of the important arteries, and making sure to always inject perpendicular to them can help prevent canalization of the artery and will help reduce the risk of intravascular occlusion. The end point of each injection occurs when visualization of the deficit is no longer appreciated (Fig. 3.3d). Of note, it is important to encourage patient feedback while injecting to assess for nerve impingement or compromise. Most patients show a great improvement with small volumes such as 1- to 2-mm syringe of product. When using HA, it is important to choose a product with the right consistency that allows for easy flow (i.e., low viscosity) through the subgaleal space, but with enough lift capacity (i.e., low G′) to volumize the forehead. When utilizing fat transfer for this region, one author (C.C.) prefers to use a moderately structural, less homogenized, or emulsified microfat graft with the objective of a smooth, durable correction, as the overlying frontalis muscle and skin overlie a deeper plane with which to structurally graft and provide such contour correction.

Fig. 3.3 (a) Important vascular landmarks to be considered when preparing to treat frontal concavity. (b) Entry points marked here with an X may vary according to the size and location of the frontal concavity defect. A small bolus of lidocaine 1% with epinephrine is injected until blanching is noted at each marked entry site. (c) Prior to injections, the face is cleansed with a chlorhexidine sponge or hypochlorous acid and the pencil markings are removed to promote an aseptic or sterile technique. The entry points are injected with lidocaine 1% with epinephrine for anesthesia. A 21-gauge needle is used to create the openings and a 25-gauge, 2-inch cannula is used to fill the frontal concavity in the subgaleal plane. (d) Patient treated with a total of 1.8 mL of hyaluronic acid to alleviate moderate frontal concavity.
In summary, injection of a cohesive, low-viscosity, low-G′, HA filler, or structural fat graft via the use of a safer subgaleal cannula injection technique allows for the effective rejuvenation of frontal concavity. A filler placed appropriately in the mid-forehead brings a more youthful and fresh appearance to the face and patients indicate a high level of satisfaction with the treatment outcome. Most treated patients observe a durability of this diluted HA filler technique of about 2 to 3 years.
3.3.2 Midface (Middle Third)
In the middle third of the face, women’s cheeks are rounder and fuller with an apex more anterolateral. This is due to a combination of more subcutaneous fat in the cheeks29,30,31 along with a more curvilinear zygoma.32 Men have an apex that is more anteromedial and subtle with a broader based malar prominence.33 This is largely due to zygomatic processes that are wider and zygomatic arches that are larger in men.11 Men also have less superficial subcutaneous fat in the midface/cheeks.30,31,34 Injecting fillers in the cheeks of men should be done with a high-G′ filler balancing a 1:1 ratio between the medial and lateral cheek.11 In comparison, the medial-to-lateral cheek thickness ratio is 1.5:1 in women.35 A cosmetic physician injecting a filler in this region should be aware of these differences to not cause feminization when injecting in the cheeks.
Revolumizing the midface and augmenting the zygomatic arch is safe and effective. This technique addresses flattening and sagging of the midface, which naturally occurs due to aging, and in many cases also enhances overall facial attractiveness. Studies have shown that a larger bizygomatic width-to-facial height ratio as measured from the upper lip to the upper eyelid or brow is perceived as being more attractive.25
Anatomy
Several anatomical structures must be considered in the appropriate use of all filler injections. When using a product that is harder to dissolve such as CaHA, this is imperative. With surgical procedures, it is of paramount importance to be mindful of the danger of transection of nerves and vessels. With filler injections, the same awareness applies. Focus should be intently on the underlying vasculature, since occlusion from injection of a product into a vessel lumen or external compression is the most fundamental complication to avoid. Vascular occlusion is fortunately rare, and the potential is further minimized when injecting a product in the periosteal region as described with this technique.36
Due to the variable nature of facial anatomy, while working around primary named arteries and nerves, extra caution is warranted. In the midface region, these include the infraorbital artery arising from the infraorbital foramen, the transverse facial artery that traverses just inferior to the lower border of the zygomatic arch, and the torturous facial artery with its anastomosing angular artery (Fig. 3.4). The primary nerve to pay attention to in this region is the infraorbital nerve, which also emerges from the palpable infraorbital foramen. Injury to this nerve can result in intractable neuralgia for a prolonged period, and therefore extreme caution is to be applied when injecting around the foramen.
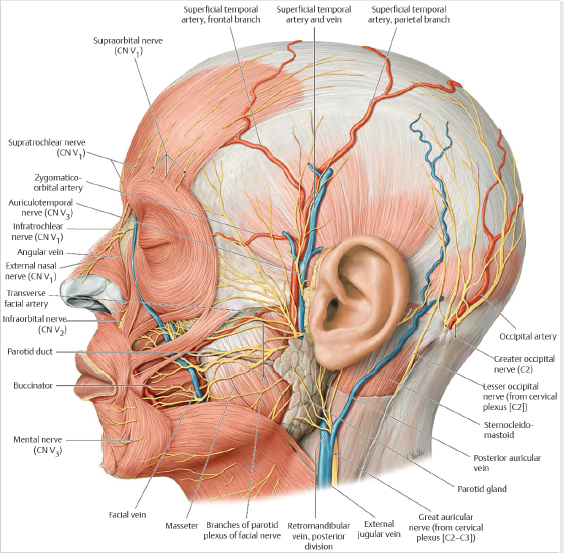
Fig. 3.4 Superficial arteries and veins of face and scalp. (Reproduced with permission from Schünke M et al., ed. Thieme Atlas of Anatomy, Volume 3: Head, Neck, and Neuroanatomy. 3rd Edition. New York: Thieme; 2020.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree