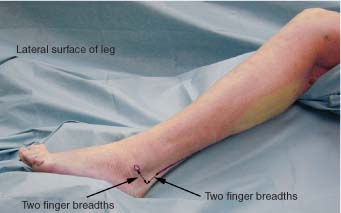
14 The sural nerve is a pure sensory nerve that supplies the lateral aspect of the foot from the heel and ankle to the small toe. For the surgeon the primary importance of this nerve is that it serves as an easily harvested source for use in cable grafting with little resultant deficit to the patient. The small, non-weight-bearing area of the foot that is left insensate is usually not bothersome to the patient. The nerve arises primarily off the tibial nerve as the medial sural cutaneous nerve. It is then joined by a contribution from the common peroneal nerve, the peroneal communicating branch. The union of these two branches then forms the sural nerve proper.1 The medial sural cutaneous nerve takes off from the tibial nerve at the middle to lower popliteal fossa. It descends in the leg between the two heads of the gastrocnemius muscle. Most commonly, just prior to piercing the deep fascia of the gastrocnemius muscle, the medial sural cutaneous nerve is joined by the communicating branch of the lateral sural nerve, itself a branch of the common peroneal nerve. This junction (of medial sural cutaneous and communicating branch of lateral sural nerve) is extremely variable, ranging from mid-popliteal fossa to 2 to 3 inches above the ankle.2 As the united sural nerve it continues to descend in the leg accompanied by the small (lesser) saphenous vein. The nerve passes over and then lateral to the Achilles tendon with small branches going to the skin and fascia on the back and lateral surfaces of the leg. In the foot, as it approaches the lateral malleolus, the sural nerve gives off lateral calcaneal branches to the skin and lateral fascia of the ankle and heel. The nerve then terminates as the dorsal lateral cutaneous nerve of the foot that travels along the lateral side of the foot and small toe supplying sensation to these areas. Positioning for exposure of the sural nerve most often depends on the reason for operation. If sural nerve exposure is required for harvesting for cable grafting and the primary nerves to be operated on require the body to be placed in a supine position (i.e., brachial plexus, femoral nerve, etc.), then the sural nerve may be harvested from a supine position. It is somewhat awkward to perform with the patient in this position, particularly because the nerve is traced more proximally, but it can be accomplished. The knee should be bent and the leg tilted medially to facilitate exposure. An incision is laid out two fingerbreadths posterior and two fingerbreadths superior to the lateral malleolus (Fig. 14-1). If sural nerve exposure is required for operations that are performed in the prone position (i.e., harvesting cable graft for sciatic nerve), then the sural nerve is easily exposed through the same incision previously outlined for a supine position (Fig. 14-2). This positioning is much less awkward for the operator, but the exposure and anatomy are identical to those encountered in the supine positioning. After the incision is marked out the skin is infiltrated with a solution of 1% lidocaine with epinephrine 1:100,000 and then incised. The nerve and muscle tendon are fairly superficial and care should be exercised accordingly in making the incision. The skin and subcutaneous tissue are incised (Fig. 14-3). If the nerve is not immediately visible, then it lies slightly anterior in the fat layer that lies just beneath the subcutaneous tissue. The nerve should be located and encircled with a vessel loop (Fig. 14-4). Care should be taken not to disrupt the lesser saphenous vein that travels with the nerve. If this vein is transected, the patient will frequently develop bothersome lower extremity edema from venous congestion. If the vein is accidentally transected, the patient should be supplied with compression-type stockings to minimize the edema. Tracing the nerve distally, it may be seen to divide off into its terminal calcaneal and dorsal lateral cutaneous nerve of the foot branches (Fig. 14-5). If traced proximally, the nerve may be followed, accompanied by the lesser saphenous vein, until its disappearance beneath the two heads of the gastrocnemius muscle (Fig. 14-6). Tracing the sural nerve more proximally for purposes of harvesting graft may offer benefit in the reduced potential for painful neuroma formation. With the proximal cut end of the nerve left deep to the gastrocnemius muscle, it is more protected and less prone to mechanical irritation.
SURAL NERVE
ANATOMY
POSITIONING AND SURGICAL EXPOSURE
< div class='tao-gold-member'>
Sural Nerve
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree