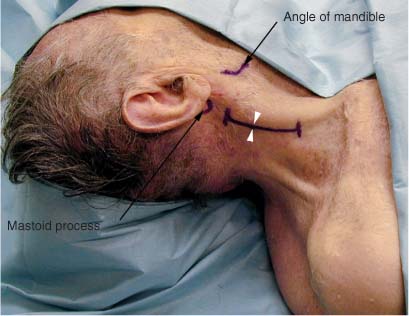
7 The fibers of the spinal accessory nerve (cranial nerve XI) are a series of rootlets that emerge from the spinal cord midway between the ventral and dorsal rootlets of the upper 5 to 6 cervical roots. They coalesce behind the denticulate ligament to form the spinal root, which then travels superiorly to enter into the cranium via the foramen magnum. Arching upward and outward, the nerve then exits the skull via the jugular foramen in the same dural sheath as the vagus nerve. Below the jugular foramen the accessory nerve passes between the internal carotid artery and internal jugular vein. It runs obliquely downward over the transverse process of the atlas and deep to the styloid process, occipital artery, and posterior belly of the digastric muscle. It then pierces the deep surface of the sternocleidomastoid muscle and supplies this muscle. Traveling lateral and obliquely, it emerges from behind the sternocleidomastoid muscle approximately one third of the way down the muscle. It then inclines inferiorly and obliquely across the posterior cervical triangle, crosses the levator scapulae, and enters the trapezius muscle ~2 to 5 cm above the clavicle. The nerve communicates with branches of the third and fourth cervical spinal nerves to form a pseudoplexus that innervates the trapezius. The spinal accessory nerve innervates the sternocleidomastoid and the trapezius muscles. The patient is placed in the supine position with the head turned to the contralateral side. A bolster is placed under the ipsilateral scapula to elevate and turn the neck slightly. The patient is moved as close as possible to the top of the table and to the side of the table from which the operator will be working. The elbows, wrists, knees, and ankles are padded for protection. The lower legs are left open for prepping and draping if sural nerve grafting is anticipated. The posterior border of the sternocleidomastoid muscle is palpated and marked. A line is imagined from the mastoid process to the clavicle along this posterior border and then divided into thirds. The spinal accessory nerve emerges from behind the sternocleidomastoid muscle approximately at the division between the upper and middle thirds of this line. The incision follows the posterior border of the sternocleidomastoid muscle (Fig. 7-1). Cervical lymph node biopsy is a common cause of iatrogenic injury to the spinal accessory nerve.1–3 If exposure of this nerve is for the purpose of repair after biopsy, the previously made biopsy incision should be used as a starting point. The ends of the existing incision may be extended superiorly and inferiorly to form a Z-shaped incision (Fig. 7-2). This allows for exposure both proximally and distally of the spinal accessory nerve. The skin and subcutaneous tissue are infiltrated with lidocaine 1% with epinephrine in a 1:100,000 solution and then divided sharply (Fig. 7-3). The operator is cautioned that the nerve lies very superficially, and once past the level of the skin the operator should proceed with caution to avoid injury to the nerve. Beneath the subcutaneous tissue the lateral border of the sternocleidomastoid muscle is located (Fig. 7-4). There are several sensory nerves that emerge from behind the sternocleidomastoid muscle; however, most of these nerves curve anteriorly over the surface of the muscle and thereby can be distinguished from the spinal accessory nerve, which does not curve over the muscle but rather heads in a posteroinferior direction. A contraction of the sternocleidomastoid muscle or the trapezius by electrical stimulation of an unidentified nerve may also help distinguish the accessory nerve, a motor nerve, from the sensory preauricular and posterior auricular nerves. At this point dissection may proceed more safely with the blunt use of a clamp to tease the nerve out of the fascial carpet rather than sharp scissor dissection (Figs. 7-5 and 7-6). The nerve may be traced proximally and distally as needed, with care being exercised to preserve the small proximal branches to the trapezius (Fig. 7-7).
SPINAL ACCESSORY NERVE
ANATOMY
POSITIONING AND SURGICAL EXPOSURE
< div class='tao-gold-member'>
Spinal Accessory Nerve
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree