Fig. 12.1
Kelly 1899 “transverse abdominal lipectomy”
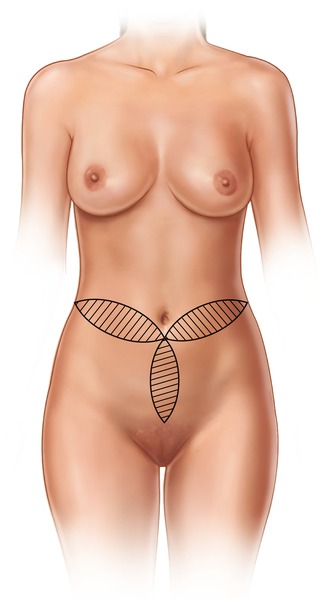
Fig. 12.2
Weinhold 1909 “cloverleaf incision”
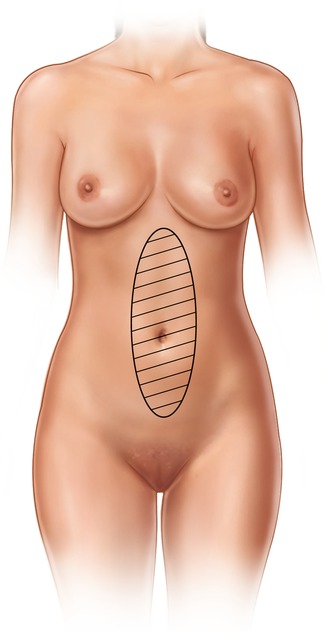
Fig. 12.3
Babcock 1916 “vertical incision”
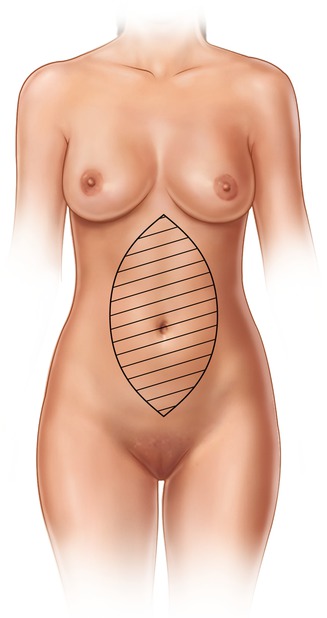
Fig. 12.4
Shepelmann 1918 “teardrop incision”
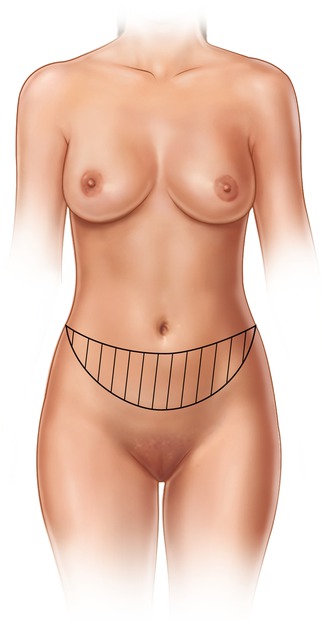
Fig. 12.5
Thorek 1923 “plastic adipectomy”
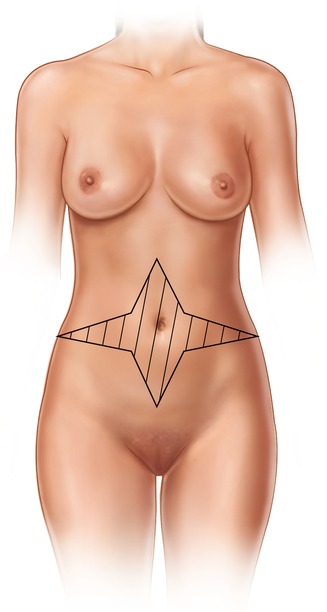
Fig. 12.6
Galtier 1955 “star design incision”
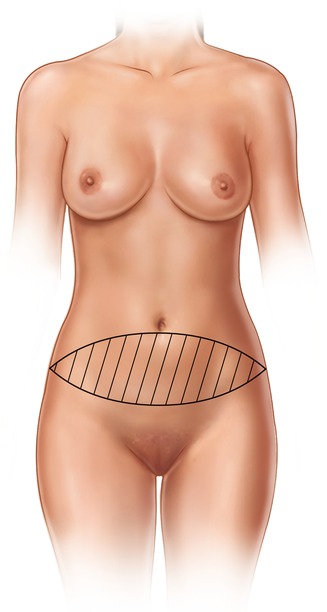
Fig. 12.7
Vernon 1957 “elliptical resection and transposition of the umbilicus”
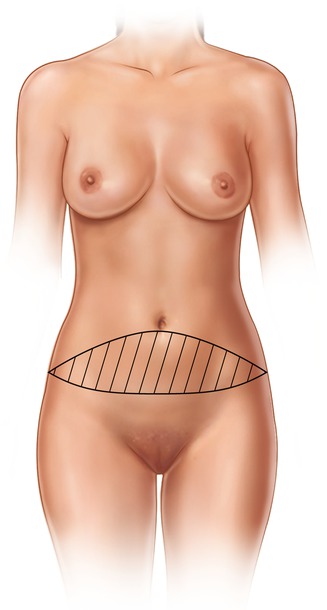
Fig. 12.8
Doufurmental and Mouly 1959 “vertical incision added to Vernon’s proposal”

Fig. 12.9
González Ulloa 1960 “circumferential lipectomy”
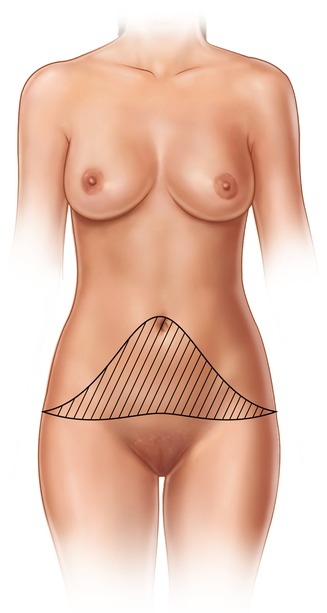
Fig. 12.10
Pitanguy 1967 “extended undermine and muscular plication”
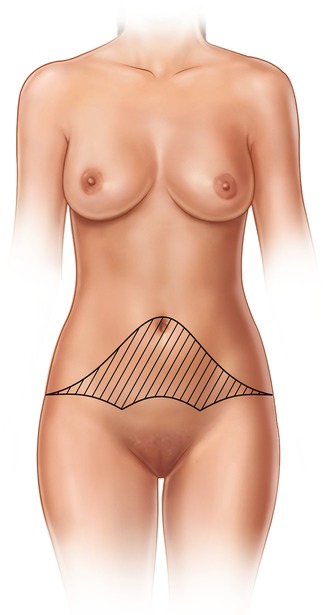
Fig. 12.11
Regnault 1972 “W shaped incision”
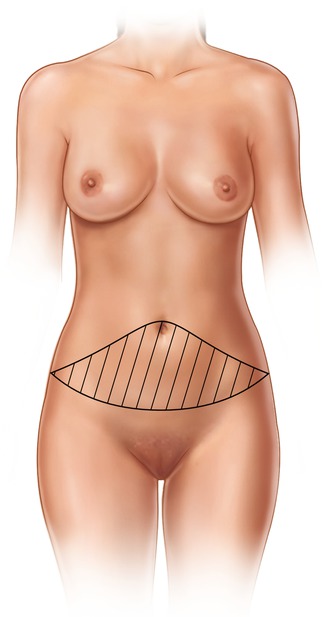
Fig. 12.12
Grazer 1973 “transverse incision follows inferior abdominal skin crease”
Fig. 12.13
Backer and Gordon 1976 “pattern follows swimwear of its time”
12.3 Anatomical Review
Knowledge of abdominal surgical anatomy including vascularity (arteries, veins, and lymphatics) and fascio-muscular planes is very important to diminish complication rate and achieve a good aesthetic result.
12.3.1 Muscles
The rectus abdominis is one of the main structures involved in abdominoplasty due to the abdominal wall weakness that diastasis recti causes and allows intra-abdominal contents to project and that is why it must be reinforced. Lateral muscles include external oblique, internal oblique, and transversus abdominis muscle converging medially forming anterior and posterior fascia.
12.3.2 Arteries
In 1979 Huger [21] described three vascular zones of the abdomen (Fig. 12.14). The main blood supply of the abdominal region comes from the deep epigastric arcade composed by superior and inferior epigastric arteries and its perforator arteries (Huger zone I); the lower abdomen receives it vascularity from external iliac artery through circumflex arteries (Huger zone II) and laterally intercostal, subcostal, and lumbar arteries (Huger zone III), but in abdominoplasty, zone III transforms in the main vascular supply.
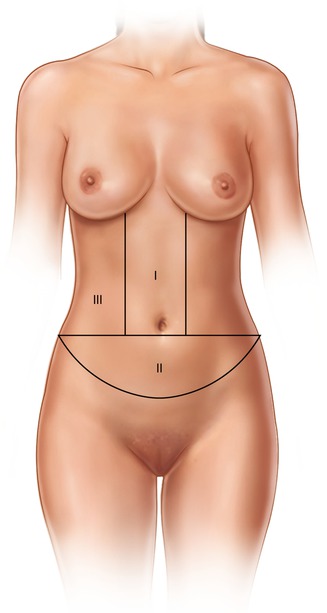
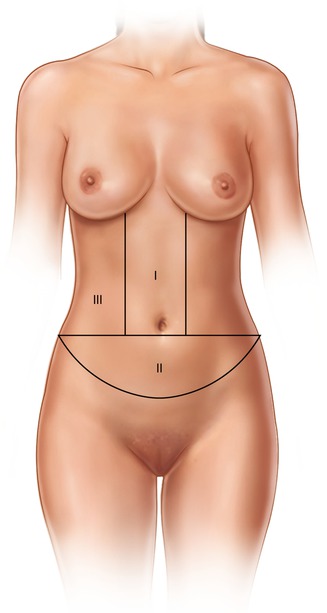
Fig. 12.14
Huger vascular zone of the abdomen
12.3.3 Veins
The venous system runs parallel with the arteries, the superior abdomen drains through the superior epigastric vein and intercostal veins toward the axillary vein, and the lower abdomen drains through superficial circumflex veins toward the inferior vena cava.
12.3.4 Lymphatics
Lymphatic drainage is divided by the umbilicus, the superior abdomen drains toward the axillary nodes, and the lower abdomen drains toward inguinal lymphatic nodes.
12.3.5 Innervation
Motor and sensitive branches originated from the last intercostal nerves, subcostal branches, ilioinguinal branches, and iliohypogastric branches (lumbar plexus) T4–L1 (Fig. 12.15).
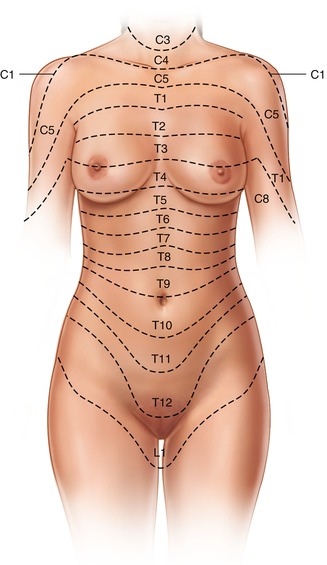
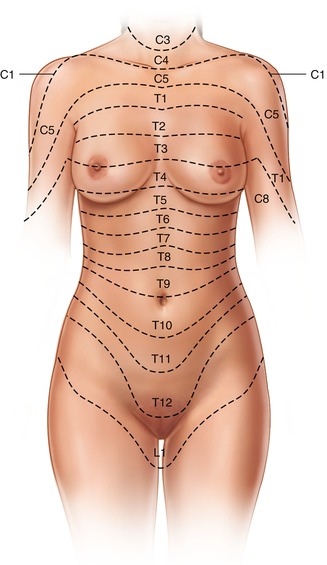
Fig. 12.15
Innervation of the abdomen
12.4 Surgical Technique
The patient is placed in supine position and the midline is marked through xiphoid appendix toward the pubis symphysis. A horizontal line is marked 5 cm to each side from the midline and extended laterally across the lower abdomen skinfold (Fig. 12.16). Infiltration with 500 mL NaCl 0.9 % plus epinephrine 1 mg (1:500,000) is injected. Incisions are made over marked lines with conventional undermining. The diastasis rectus is marked, and cross sutures of polypropylene no. 1 are placed drawing three transverse curved “SMILE”-shaped lines from the semilunaris line to the contralateral semilunaris line. A continuous suture is placed from the midline toward the semilunaris line and then back toward the contralateral semilunaris line then continuing to the midline and pulling the suture then knotted (Figs. 12.17




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







