10
Skin Rejuvenation
Steven J. Pearlman and Monica Tadros
Advances in medicine have fostered a healthier, longer life span. With this, individuals are conscious that their changing outward appearance no longer matches their physical wellness. The concept of aging with grace has been transformed to convey an image of seasoned beauty with youthful preservation. Positive self-image with advancing age and an appreciation for the effects of photoaging on the skin are at the forefront of popular culture. Skin rejuvenation continues to be a rapidly expanding discipline encompassing medicine, technology, and the beauty industry. Our patients seek more youthful skin through ever-improving skin care and laser technology. In the United States, cosmeceuticals represent a $5.4 billion per year industry that is propelled by a stream of new products offering age-defying and other appearance-enhancing benefits and is predicted to grow 8.5% annually.1 According to the 2005 survey of the American Academy of Facial Plastic and Reconstructive Surgery, laser skin rejuvenation has increased by 64%, microdermabrasion by 103%, and botulinum toxin use for facial wrinkles has increased 162% since 2001.2
Improved surgical techniques have facilitated a more natural, aesthetic appearance in the treatment of the aging face. However, it is important to understand that complete facial rejuvenation must include skin restoration in addition to surgical facial rejuvenation. The three targets for reversing skin aging are (1) skin color and texture, (2) loss of skin elasticity and collagen degradation, and (3) dynamic lines from hyperactive facial muscles acting on the overlying skin. Skin products can now target aged skin with several ingredients that stimulate collagen production, increase epidermal turnover, and reverse photoaging. Skin peels have been used for centuries to restore more youthful skin. Botulinum toxin treatment complements skin care regimens by relaxing facial muscles that cause overlying wrinkles.
Laser skin resurfacing technology has also paralleled the growing quest for more youthful skin. What was the mainstay for cutaneous exfoliation a decade ago—the CO2 laser— has been eclipsed by less invasive techniques. Several lasers with shorter or even no healing time have been developed. Minimally invasive lasers, otherwise known as nonablative lasers and laser-like devices, when coupled with skin care are slowly approaching results once only achievable with ablative lasers or deep chemical peels. With such a variety in treatments, the cosmetic surgeon must properly evaluate the patient’s needs and select an appropriate treatment plan.
Skin type, extent of photoaging, associated dynamic wrinkles, and facial aging must all be taken into account (Table 10.1). As with all of medicine, treatment for facial aging starts with proper diagnosis. Therapy can range from home topical products to minimally invasive office procedures to aggressive, ablative resurfacing. Treatment can then be directed at the diagnosed problems and tailored according to the patient’s tolerance for minimal to invasive treatment. Comprehensive care for the aging face often encompasses treating patients with several skin care modalities. Combination treatments can then address multiple causes for the aging face for superior results.
♦ Facial Skin Aging
The primary goal of skin rejuvenation is to combat aging, photodamaged skin. Years of exposure to the sun causes significant skin changes and accelerates natural skin aging (Table 10.2). Skin changes manifest as facial lines, irregular pigmentation, erythema and telangiectasias, and textural changes. Facial aging is most often equated with the appearance of wrinkles. Wrinkles, rhytides, creases, folds, and furrows come from several causes and are only a part of what makes a face appear older. Aging changes within the skin make wrinkles more prevalent. Wrinkles have been found to have no distinguishing histologic features.3 They may occur from redundant skin, muscular expression, or loss of skin support. These changes are only minimally affected by resurfacing. Another interpretation divides them into fine wrinkles that are present at rest and may be less evident with facial expression.4 Medium wrinkles, which we call dynamic wrinkles, are accentuated by facial expression and may have alteration in the elastosis of the surrounding skin. Coarse, deep wrinkles are visible at rest, too. These are accentuated by facial expression, such as nasolabial folds and areas of fat herniation and tissue redundancy. Medium and deep wrinkles may be better treated by other or combined modalities such as facial fillers and surgery.
|
|
Aging skin is accelerated by photodamage, resulting in coarser texture, pigment changes, telangiectasias, actinic keratoses, and even epidermal malignancies (Table 10.3). The skin ages by thinning of the epidermis and flattening of the junction with the dermis.5 Photoaged skin (a more common finding in patients seeking resurfacing) actually has a thicker epidermis, but the outer keratin layer is irregular. There is increased water loss from the skin and a decrease in the sebaceous glands lubricating the skin. More abnormal cells accumulate in aged skin, especially if there is chronic sun damage, leading to precancerous and cancerous lesions. Photoaging also causes chronic inflammation within the skin. There is an increase in elastin that clusters into thick bundles with sun damage. Collagen decreases as we age, and the bundles of collagen become looser and lose strength. Capillaries and small blood vessels regress from the skin, reducing blood flow. The more superficial vessels can thicken from sun exposure, also reducing their capacity to nourish the skin. Telangiectasias (spider veins) appear on the surface of the skin, which are too superficial to provide nourishment. Loss of blood supply can also contribute to thinning of the hair and paler skin.
|
The skin becomes less able to resist stretching with loss of elasticity. When coupled with gravity, muscle pull, and tissue changes beneath, wrinkling occurs. The skin is also less able to resist mechanical damage and heals more slowly from insult. Water loss and breakdown of bonds between the cells reduces the barrier function of the skin. Pore size increases as well. It becomes more evident that maturing skin comprises only two of the five components that contribute to facial aging.
♦ Skin Evaluation and Diagnosis
Analysis of the aging face with proper diagnosis of the dominant causes is necessary for appropriate treatment. Facial aging occurs by five independent yet interactive components: inherent skin changes, dynamic lines, loss of tissue elasticity, effects of gravity, and soft tissue loss. Understanding these changes, how they manifest and what promotes them, is the first step in proper pretreatment analysis (Fig. 10.1).
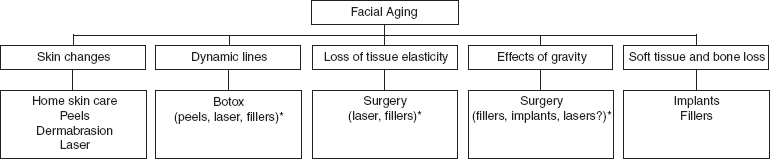
Fig. 10.1 Facial aging: classification of the five causes and treatment for each (alternative treatments are in parentheses; *less effective alternatives).
Patient Selection
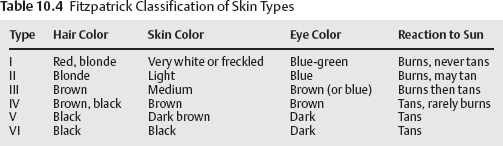
Patient selection begins with a careful skin history. One must inquire about skin care routines, sun habits, smoking, medications that may increase photosensitivity, and general medical conditions. Included in the history is use of the Fitzpatrick classification of skin types (Table 10.4).6 This classification helps us predict the reaction to photoenergy from laser treatments and medium to deep chemical peels. The Fitzpatrick classification quantifies the amount of inherent melanin in the skin as a primary chromophore. This system is then used in determining appropriateness for ablative treatments as well as laser settings for more predictable results.
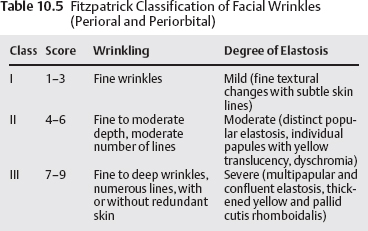
The extent of photodamage should be determined by skin inspection. A scale is used to record skin changes to aid in planning and provide a tangible description of the skin. Both Fitzpatrick7 and Glogau8 described useful classifications for photodamaged skin (Tables 10.5 and 10.6). Proper diagnosis and classification is then used to plan treatment. Photographs are taken in the frontal (full face), oblique, and lateral (profile) views with close-ups of any areas of particular interest. Uniform lighting and camera exposures are necessary to document the often-subtle changes in skin tone and texture. Less commonly used diagnostic techniques for pretreatment evaluation include digital photography that allows skin magnification for closer skin inspection, ultraviolet exam, high-resolution dermal diagnostic ultrasound, and three-dimensional microtopography.9
|
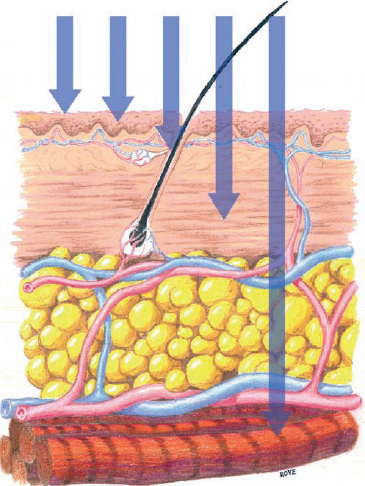
Fig. 10.2 Depth of penetration of skin treatments. Left to right (arrows): (1) home skin care treats superficial epidermis; (2) superficial peels and microdermabrasion to deep epidermis; (3) laser and medium-depth peels treat pigment in papillary dermis and vessels in papillary/reticular dermis, superficial collagen; (4) ablative and nonablative lasers and deep chemical peels treat collagen to depth of hair follicles; (5) botulinum toxin and surgery affect full-thickness skin. (From Pearlman SJ, Chernoff WG. Laser resurfacing of the face: analysis and diagnosis. Facial Plast Surg Clin 2003;11:335–347. Reprinted with permission.)
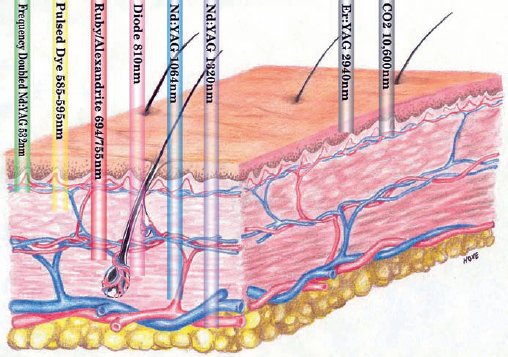
Fig. 10.3 Depth of penetration of (left) non-ablative and (right) ablative lasers. (From Pearlman SJ, Chernoff WG. Laser resurfacing of the face: analysis and diagnosis. Facial Plast Surg Clin 2003;11:335–347. Reprinted with permission.)
Treatment Planning
Facial skin rejuvenation ranges in complexity and depth of penetration from home topical cosmeceuticals to office procedures such as microdermabrasion and medium-depth chemical peels to ablative laser resurfacing and deep chemical peels. Topical skin products rejuvenate, and some exfoliate, the skin. They penetrate the stratum corneum and can reach the superficial papillary dermis. Superficial peels remain within the epidermis or granular layer with a depth of penetration of ˜0.06 mm. Medium-depth peels (both laser and chemical peels) extend into the papillary or upper reticular dermis at a depth of ˜0.45 mm. Deep peels extend into the midreticular dermis with a depth of ˜0.6 mm (Fig. 10.2).10 Although superficial chemical peels do not produce dramatic results, they are safe to use in all skin types. Laser resurfacing and medium-depth and deep chemical peels may be more effective but given their depth of penetration carry an increased risk of pigmentary complications in patients with Fitzpatrick skin types III through VI.11 Nonablative lasers can penetrate to variable depths in what will later be described as “subsurface” skin rejuvenation (Fig. 10.3). Ablative lasers rejuvenate to the papillary-reticular junction with deeper thermal effects.
♦ Chemical Peels
Superficial
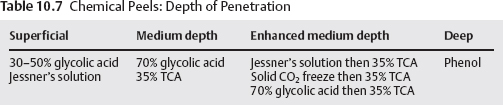
The depth of penetration from superficial peels remains at the level of the epidermis. A light superficial peel removes only the stratum corneum, whereas a full superficial chemical peel destroys the entire epidermis. Progression beyond the epidermis into the papillary dermis constitutes a medium-depth peel, whereas a deep chemical peel results in further penetration into the reticular dermis (Table 10.7).11
Glycolic acid peels with concentrations in the range 30 to 50% and Jessner’s solution are popular superficial chemical peels for the treatment of acne and photoaging that produce deeper epidermal exfoliation. Jessner’s solution is composed of 14% resorcinol, 14% salicylic acid, and 14% lactic acid usually formulated in 100 mL ethanol.12 Trichloroacetic acid (TCA) peels in the range 10 to 30% and salicylic acid at concentrations of 20 to 30% can also be used to achieve a superficial peel.13,14 The clinical efficacy of these peels is variable and dependent on the clinical scenario and desired outcome. Studies have shown that superficial peeling agents help exfoliate the skin but do not diminish sebum production, one of the main etiologic factors resulting in acne formation.15 They are safe to use in the majority of skin types, but it is always prudent to initiate treatment with the lowest concentration superficial peel to survey sensitivity in patients with Fitzpatrick skin types IV through VI.
Microdermabrasion
Microdermabrasion was first described in Italy in 1985. Its relative ease, safety, and lack of down-time have fostered its current popularity in the United States. Treatments are so gentle that they are offered in spas and salons without direct medical supervision. Microdermabrasion is a gentle abrasive procedure that uses the assistance of a closed-loop vacuum apparatus to mechanically débride the thickened keratin layer of epidermis. Skin is exfoliated by the projection of a stream of aluminum oxide crystals at a controlled intensity generated by a vacuum compressor. Greater treatment depth is created by increasing the pressure of the jetted crystals, increasing the suction to stretch the skin tautly, and decreasing the speed of each pass.12 As the suction removes dead epidermal skin cells and stretches the skin, it stimulates blood flow to the skin surface and may result in a transient hyperemia. This improved microcirculation in response to superficial intraepidermal injury presumably stimulates local collagen production by fibroblasts in the papillary dermis and improves lymphatic drainage of the deeper structures.
Microdermabrasion has gained popularity in treating photoaging, dyschromia, acne, mild scarring, and, to a lesser degree, fine wrinkles. Conservative treatments can be performed by microdermabrasion in a series of treatments at weekly intervals until desired results are achieved, followed by monthly maintenance therapy with no down-time. Microdermabrasion is touted to rejuvenate skin, soften fine wrinkles and stretch marks, and treat hyperpigmentation and acne scars. Results from these latter claims are minimal. It is safe to use on all skin types at all ages and has minimal if any recovery time. Adjustments in settings and technique can be tailored to the sensitivity of the individual. If deep erosion of the epidermis is attempted in patients with less sensitive skin, more marked desquamation a few days after treatment should be anticipated.
Clinical improvement after serial treatments is attributable to chronic stimulation of a low-grade reparative process at the level of both the dermis and the epidermis. The stratum corneum is buffed and compacted with flattening of the rete pegs after a single microdermabrasion procedure.16,17 After serial procedures, comparative histopathologic analysis reveals epidermal and dermal hyperplasia, decreased pigmentation, perivascular inflammation, and hyalinization of the papillary dermis with a small increase in dermal collagen and elastin.18,19
The results of microdermabrasion for facial rejuvenation remain subjective and patient dependent, but studies suggest that short-term improvements in texture and skin tone are observed.16 Because microdermabrasion is effective in exfoliation and refining pore size, it is best considered an adjunct to skin care in patients with sebaceous skin or large pores that frequently plug with keratin debris.
Whereas superficial peels and microdermabrasion both provide epidermal exfoliation, microdermabrasion additionally stimulates fibroblasts and dermal collagen deposition through an unidentified mechanism. The efficacy of superficial peels and microdermabrasion is dependent on patient compliance with routine skin care regimens and the continuation of maintenance procedures. The frequency of maintenance procedures is patient specific but in many cases is required monthly.15 Concurrent topical therapy may include tretinoins, hydroxyacids, bleaching agents, and sunscreens. For example, mild photoaging can be addressed with microdermabrasion combined with an α-hydroxyacid skin care regimen, and acne scarring or melasma can be optimized with the concurrent use of retinoid therapy.13
In an era of widespread availability and technological advancements, the importance of simple skin care adjunct procedures cannot be underestimated. Even where more invasive procedures are indicated, final outcomes are improved by taking the time to address skin tone and texture. The safety profile and minimal down-time of superficial peels and microdermabrasion are their most attractive features, but their outcomes are often criticized with regard to facial rejuvenation. The practitioner must appreciate that superficial resurfacing strictly achieves skin rejuvenation by improving tone and texture, which is only one component of complete facial rejuvenation. For this reason, patient selection and informed consent are critical to maintaining satisfaction with superficial procedures.
Darker-skinned individuals have more complaints of pigmentary dyschromia and acne when compared with Caucasians who more commonly complain of photodamage and rhytides. With this variability, the requirements for skin rejuvenation are often different for darker skin types. Darker skin types have thicker skin with increased layers of stratum corneum and a tendency to produce exaggerated responses to cutaneous injury.13 These patients benefit most from epidermal exfoliation procedures that do not result in dermal penetration or melanocyte activation. Appreciation of this fact highlights the utility of superficial skin resurfacing, especially in this population of patients. Pretreatment with 4% hydroquinone or 20% azelaic acid for 2 weeks is recommended to diminish melanocyte activity and minimize posttreatment hyperpigmentation.13
Dermabrasion
Dermabrasion dates back to 1500 BC, when Egyptians first used sandpaper to smooth scars. The use of sandpaper progressed to motorized dermabrasion in 1905 when Kromayer, a German dermatologist, demonstrated that ablation into the reticular dermis could be used to treat various skin conditions without scar formation.20 Throughout the 20th century, dermabrasion remained the gold standard to which all new deep skin resurfacing modalities were compared.
Dermabrasion removes the epidermis and dermis by use of a rotary abrasive motorized hand-piece. The depth of injury is at the level of the middermis near the junction of the papillary and reticular dermis. Wound healing is lengthy and requires reepithelialization by the remaining dermal adnexal structures. Because scars and keloids lack adnexae, they do not respond as favorably to dermabrasion.21 Dermabrasion has been used to successfully treat postacne scarring, melasma, rhinophyma, and a variety of lesions including actinic and seborrheic keratoses. Tattoo removal can be addressed with dermabrasion, but given the advent of lasers that treat pigment directly without scarring, dermabrasion has fallen out of favor for this purpose except where cost is a prohibitive factor.12,20
Deep
The Baker phenol peel is a deep peel that has been used for decades to reliably improve heavy rhytides (Figs. 10.4 and 10.5). The Baker formula phenol may be applied with or without occlusion. Occlusion deepens penetration to the midreticular dermis by the application of waterproof zinc oxide tape as soon as the agent is applied to each subunit. With deeper penetration comes the increased risk of scarring should the reticular dermis be breached.

Fig. 10.4 Deep chemical peel with Baker-Gordon formula (before treatment).

Fig. 10.5 Deep chemical peel with Baker-Gordon formula (after treatment).
In 1961, the Baker-Gordon modification reduced the concentration of phenol from full strength to 55% phenol. Whereas full-strength phenol caused immediate coagulation blocking further penetration by the agent, dilution enabled keratolysis to improve depth of penetration.11 The addition of croton oil facilitates deeper penetration of the phenol.
Phenol is absorbed through the skin and causes concentration-dependent toxicity. This procedure requires preoperative hydration and intravenous sedation. Typically, 1 L of fluid is given preoperatively, and 1 L is given during the procedure to dilute serum concentrations. Additional precautions include the use of supplemental oxygen and treatment of facial units at 15-minute intervals extending the time of application of a full face peel to 90 minutes. EKG monitoring for cardiac arrhythmia is performed, and the procedure is stopped if any signs of premature ventricular contractions or premature atrial contractions are encountered. The peel is contraindicated in patients with a history of cardiac disease or hepatic or renal compromise. In the event of an adverse reaction, mineral oil can be used as a diluent of phenol.11
With the availability of numerous alternatives, despite its efficacy, phenol has fallen out of favor for most practitioners given its rare but life-threatening complication of cardiac arrhythmia. Stronger concentrations of 50% or greater TCA alone are also less commonly used, given the poor control of injury and high risk of scarring at concentrations of 50% or greater.22
Enhanced Medium-Depth
TCA may be used alone in the concentration of 35% to achieve a standard medium-depth peel. Enhanced medium-depth peels are the preferred technique to deepen a medium-depth peel with less risk of complication than with a true deep peel. Pretreatment with other agents such as freeze technique using solid CO2 followed by 35% TCA,22 Jessner’s solution followed by 35% TCA,23 or 70% glycolic acid followed by 35% TCA24 first removes the epidermal barrier with a superficial peel to achieve a stronger, more even medium-depth peel in the same setting. These alternative enhanced 35% TCA peels achieve results comparable with 50% TCA with fewer complications.11 In the event that an inappropriate concentration of an acidic formulation is used, saline and bicarbonate of soda can be used as a diluent.
Enhanced medium-depth chemical peels are suitable for patients with Glogau type II or III photoaging including pigmentary changes, lentigines, epidermal growths, actinic keratosis, dyschromia, and rhytides. They are safest to use in Fitzpatrick type I or II patients; many type III patients may also qualify depending on their skin type. Thicker skin types in patients reporting a low propensity for scar formation or pigmentary abnormalities are better candidates.11
Enhanced medium-depth peels are relatively safe, single-stage procedures with a recovery time of approximately 7 to 10 days. Patients do not require intravenous sedation; mild sedation and pain medication are generally sufficient. Antiviral medications are initiated on the day of resurfacing and are continued until the skin is fully reepithelialized in patients with a history of herpetic infection.25 The use of prophylactic antibiotics remains controversial. Patients with Fitzpatrick skin types IV through VI are pretreated with 4% hydroquinone or 20% azelaic acid for 2 weeks to diminish melanocyte activity and minimize posttreatment hyperpigmentation.
The technique is as follows: the patient is positioned upright at 30 degrees with his or her eyes closed. Degreasing the skin with cleanser and gauze to débride the stratum corneum is critical to ensure uniform penetration of the agent. Preparation with a cleanser such as Septisol (STERIS Corporation, Mentor, OH) followed by acetone to remove residual oil and debris is recommended for this purpose. A commonly used enhanced medium-depth peel (preferred by the authors) was first described by Monheit23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








