Amezinium methylsulfate [25]
Anagrelide [36]
Barbituric acid [32]
Diltiazem [4]
Erythropoietin [16]
Estrogen combinations [40]
Furosemide [39]
Hydralazine [24]
Nifedipine [28]
Pentamidine [17]
14.2 Medications
14.2.1 Hydroxyurea
Hydroxyurea, synonym referred as hydroxycarbamide, is a hydroxylated urea derivative which inhibits as an S-phase-specific inhibitor of ribonucleotide reductase the DNA synthesis. It is clinically used for the treatment of patients with chronic myelogenous leukemia, essential thrombocythemia, and polycythemia vera.
In a retrospective study, 41 patients were presented in which a leg ulcer was caused by hydroxyurea. In these patients with a mean age of 67 years, it came after an average treatment period of 5 years with hydroxyurea to the onset of ulceration. In total, 80 % of patients with ulcers healed after discontinuation of the medication. Clinically, in most patients, multiple ulcerations in the area of the malleoli could be found [41]. Comparable data have been presented by Best et al. in a study of 14 patients [2].
Hydroxyurea is the most widely publicized medication that is associated with the development of leg ulcers. It has been described that the first appearance of this extremely painful ulcerations is usually 1–10 years after starting treatment with hydroxyurea [10, 11, 14]. Hydroxyurea-induced ulcers are manifested in particular symmetrically in the area of the malleoli, dorsum of the foot, or heel (Figs. 14.1, 14.2, 14.3, and 14.4). The underlying pathogenesis is so far not fully understood. It was discussed that a graft-versus-host-like reaction with degeneration of the basal keratinocytes and an epidermodermal gap formation could be directly related to cytostatic effects of hydroxyurea on the basal keratinocytes. In addition, a disturbance of microcirculation by effects on erythrocytes with decrease in their number, increase of their mean volume, and thus reduced deformability has been described [41, 44]. The atrophie blanche was discussed to be a clinical indicator for an underlying disturbed microcirculation (Fig. 14.5). Several of these lesions are not reversible, so that despite discontinuation of therapy in some patients, recurrence of ulcerations can be found [23].



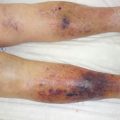
Figs. 14.1, 14.2, 14.3, and 14.4
Extremely painful ulcerations of the lower legs in different patients after long-term intake of hydroxyurea

Fig. 14.5
Livid erythema with clinically typical atrophie blanche in a patient after many years of taking hydroxyurea
14.2.2 Anagrelide
Anagrelide is an imidazoquinazoline derivate, which is used for the treatment of patients with myeloproliferative diseases such as essential thrombocythemia. The inhibitory effect of anagrelide on human platelets is mediated by formation of a delay of maturation of megakaryocytes by inhibiting cyclic AMP phosphodiesterase III.
In a case report, our group reported a 38-year-old patient with extremely painful ulcers with atrophie blanche on both outer ankles, which occurred 6 weeks after starting treatment with anagrelide (Figs. 14.6 and 14.7). Despite an intensified advanced wound therapy, the wounds were refractory. A complete healing of the ulcer was achieved after stopping of the medication. An underlying disturbed microcirculation comparable to hydroxyurea effects was discussed [36].


Figs. 14.6 and 14.7
Patient who developed 6 weeks after he starts taking anagrelide an atrophie blanche (Fig. 14.6) and shortly later very painful ulcerations in the area of both lateral ankles (Fig. 14.7)
14.2.3 Coumarins
Coumarins derived from 4-hydroxycoumarin compounds are well known as drugs with an inhibitory effect on coagulation. Coumarins have a structure similar to vitamin K. They are used clinically as for the treatment and prophylaxis of thrombosis and embolism. The effect as anticoagulants is based on the inhibition of plasmatic coagulation. Coumarins bind instead of vitamin K to the enzyme vitamin K epoxide reductase, block it, and thus inhibit competitively the formation of active clotting factors. The two most commonly used in medicine are phenprocoumon coumarins and warfarin.
In a case series report, three patients were described in which it came within 5 days after initiation of therapy with warfarin to painful, sharply defined erythema, which ulcerated secondary. All patients were obese. The authors discussed the fact that the coexistence and may be other individual factors are important for the development of coumarin necrosis [13]. Another case report described a 67-year-old patient with the occurrence of leukocytoclastic vasculitis of the lower limb 4 weeks after he starts coumarin therapy [42]. Skin necrosis occurred at 0.01–0.1 % of all patients after taking coumarins. This necrosis can be observed more frequently in patients with congenital protein C deficiency or rarely described association with a deficiency of protein S [31]. In addition, the affected patients may be more common in obese women. Skin necroses usually appear symmetrically on the chest, abdomen, or buttocks. Besides severe pain, often petechiae, erythema, and ecchymoses are the first clinical signs. As the condition progresses, crusts, hemorrhagic bullae, necrosis, or ulcer can be observed. As the underlying pathophysiology at the beginning of therapy with coumarins, hypercoagulative statuses by the imbalance of the various anticoagulant mechanisms have been discussed. The resulting microvascular thrombotic occlusions typically cause necroses. The first clinical symptoms start within 1–10 days, usually on day 3–6 [5]. Only in rare cases, it can also occur even after several years of the onset of necrosis [15]. The median age of onset is 54 years; about 75 % are women, and about 60 % of the necroses are localized at the legs, breasts, or buttocks [5].
14.2.4 Heparin
Heparin is a mucopolysaccharide polysulfate, which binds to among others antithrombin III, causing the inactivation of many coagulation factors. Thereby, its anticoagulant effects are enhanced. Heparin preparations are used for the prophylaxis and treatment of thromboembolic disorders. The occurrence of purpura with necrosis in the injection areas and in other parts of the body has been reported. As a potential pathogenic mechanism, a leucocytoclastic vasculitis is described.
Another pathological reaction is the heparin-induced thrombocytopenia type II (HIT II), which may lead to arterial and venous thrombosis with necrosis. HIT is caused by the formation of autoantibodies against the heparin platelet factor 4 (PF4) complexes and occurs in 0.1–2 % of all patients treated with heparin. After the beginning of heparin treatment, HIT II usually occurs within 10–14 days. If a heparin treatment has been done in the previous 100 days, the disease can manifest itself much more rapidly [18].
In a 66-year-old woman with diabetes and hemodialysis who received intravenous heparin during hemodialysis, the occurrences of ulcers of the lower legs were described [27]. Our group already described a 38-year-old patient in whom HIT II led to multiple necroses and ulcers on the mucous membrane and integument. The painful, sharply defined necroses with inflammatory surroundings were not localized at the injection sites [18].
14.2.5 Methotrexate
Methotrexate (MTX) is an analog of folic acid and competitively inhibits dihydrofolate reductase. As an antimetabolite, it inhibits DNA and RNA synthesis. The drug is dosed higher in oncologic patients as part of chemotherapy. Lower doses are widely used in the treatment of patients with rheumatoid arthritis or psoriasis vulgaris.
In the literature, a 39-year-old woman with non-Hodgkin’s lymphoma was described. Two months after starting a therapy with 15 mg MTX once weekly, painless ulcerations on the malleoli appeared. One year ago, similar ulcerations occur after a combination therapy with 7.5 mg MTX and indomethacin was initiated. After discontinuation of the therapy within 2 months, the ulcers healed completely [8]. The occurrence of generalized erosions and ulcerations of psoriatic plaques was described in a case series report in 47 patients. As a risk factor, the co-medication with NSAIDs has been described [33].
14.2.6 Leflunomide
Leflunomide is a drug from the group of immunosuppressants, which is used as a therapy for patients with rheumatoid arthritis and psoriasis. The active metabolite of leflunomide, A771726, inhibits the enzyme dihydroorotate dehydrogenase, a key enzyme for de novo biosynthesis of pyromidine [38].
Our group described a 68-year-old woman with rheumatoid arthritis who developed ulcers during treatment with leflunomide. The patient described 3 months after starting treatment with leflunomide the appearance of a purpura which ulcerated in the following days. As the result of a vasculitis, an extremely painful, sharply demarcated ulceration with livid edges above the right malleolus occurs [19, 26]. Another case report described a 78-year-old woman with rheumatoid arthritis and ulcers, which appear 6 months after starting treatment with leflunomide. It was discussed that a direct toxic effect of leflunomide on epidermal cells could be relevant, since leflunomide blocked in vitro, for example, epidermal growth factors [29]. In another case report, a 63-year-old patient who had suffered for 14 years from rheumatoid arthritis developed 10 months after initiation of leflunomide treatment on both lower legs spontaneously ulcerations. Neither serological nor histological signs for an underlying vasculitis could be found. After discontinuation of leflunomide therapy, the ulcers healed after 8 months [22].
14.2.7 Hydralazine
Hydralazine is a derivative of phthalazine. In some countries, it is used therapeutically as hydralazine hydrochloride in combination, for example, with atenolol or metoprolol and hydrochlorothiazide or for the treatment of essential hypertension.
In a 50-year-old man, very painful ulcers on the Achilles tendon were described after the intake of hydralazine for 3 years. The histology showed newly occurred autoantibodies comparable to the first manifestation of systemic lupus erythematosus. The authors discussed the occurrence of the ulcer as a manifestation of a drug-induced lupus erythematosus. After discontinuation of hydralazine, the ulcer healed ulcers quickly and completely [24].
14.2.8 Amezinium Methylsulfate
Amezinium methylsulfate is an indirect α-sympathomimetic which is used therapeutically in patients with essential and symptomatic hypotension. Amezinium methylsulfate inhibits the intra-dimensional monoamine oxidase, thus causing decreased norepinephrine degradation. Furthermore, it inhibits norepinephrine reuptake in the sympathetic neuron. Through these mechanisms, the noradrenalin amount increases in the peripheral receptors. This leads to vasoconstriction and the blood pressure rises.
A case report described a 52-year-old patient, who suffered for 22 years from a chronic glomerulonephritis, had hemodialysis, and had already developed a generalized vascular calcification. One year after starting treatment with amezinium methylsulfate, he developed painful leg ulcers which were refractory to different treatments for over 7 months. After discontinuation of the drug, the ulcers healed within a few weeks. The authors discussed that the vasoconstrictive effects of the drug can be an important cause for the ulceration [25].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree