Fig. 12.1
Posteroanterior flexion weightbearing (a) and lateral (b) X-rays of a left knee 11 years after ACL reconstruction showing vertical placement of the ACL tunnels with proximal positioning of suspensory fixation hardware and slight tunnel widening (arrows)
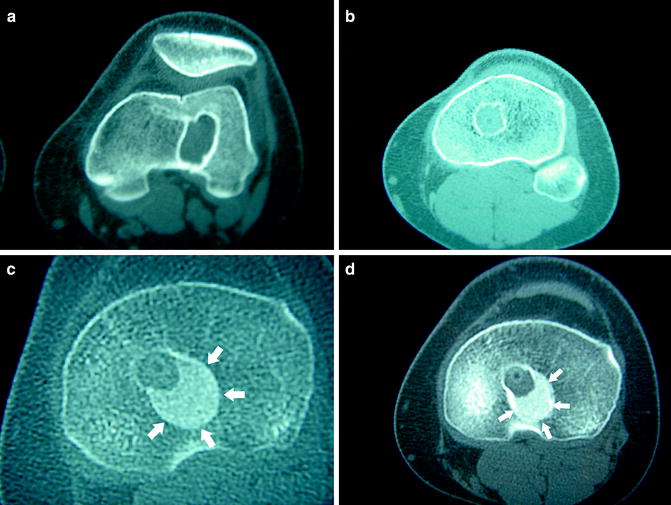
Fig. 12.2
Selected axial computed tomography images showing pre-revision tunnel widening in the femur (a) and tibia (b), the tibia at 2 months (c) and 5 months after revision ACL reconstruction (d). White arrows show allograft bone dowel incorporation into tibia used during revision reconstruction
The patient must be aware of possibilities and appropriately counseled regarding expectations and outcomes. Setting realistic goals and describing the unpredictability of revision ACL surgery is key for the patient to understand. They should be counseled that they will have a more conservative rehabilitation program following the revision surgery. Patients should be aware that return to their original pre-injury level is variable, if not unlikely. Often times, it is not possible to fully determine if a single stage or multiple stages are necessary for successful revision preoperatively, and the patient should give consent for possible additional surgery if necessary [5].
Preoperative discussions should also include graft choice. A review of previously used graft from the index procedure and a menu of available choices for autograft should be obtained. The patient should understand the morbidities associated with autografts and the risks associated with allografts, including disease transmission and a potentially higher risk of failure.
Timing of revision surgery has also been shown to be a significant factor for the development of radiographic apparent arthritis [3]. It is hypothesized that the continued instability of the knee may lead to further chondral injury and meniscus damage. Thus, avoiding activities that may lead to knee instability is prudent and operating earlier to restore stability is optimal.
Finally, the hospital or surgery center should be stocked with the necessary implants and have access to the necessary equipment for revision surgery. Allograft tissue should be available, even if only as a backup for planned autograft procedures. Custom-sized materials should be ordered in advance, and specific instrumentation for removal of implants should be available. Always have a universal screw removal set available. Fluoroscopy can be an extremely useful tool intra-operatively to assist with hardware removal or the avoidance of prior tunnels.
Treatment Options
The decision for single staged ACL revision surgery should be made on an individualized basis for each patient. The surgeon must have multiple options available to him/her at the time of surgery. Again, a thorough workup is necessary to determine cause of failure and to correct these at the time of revision surgery. The surgeon must be prepared for meniscal work (i.e., repair or partial meniscectomy), cartilage treatment, reconstruction of other ligaments, or the correction of malalignment issues at the time of revision surgery.
Decisions regarding tunnel placement, graft choice, and fixation must be made prior to surgery. The revision surgeon must make the decision both preoperatively and ultimately intra-operatively about previous tunnel placement whether to retain these tunnels or to make new ones. When tunnel expansion has occurred beyond the point at which adequate fixation of the graft is possible, then the two-stage approach must be undertaken. Tunnels that are 16 mm or less can generally be reused in one stage, whereas larger tunnels are generally best treated with bone grafting and a two-stage reconstruction. Backup secondary fixation should be utilized if primary fixation is not optimal.
If the previous tunnels are accurately placed, the surgeon must remove all of the previous graft and be sure to have a healthy base of tissue for the new graft to incorporate (Fig. 12.3a–c). This may require increasing the size of the tunnels with curettes and reamers to remove granulation tissue formed at the periphery of the old tunnel. Larger fixation devices may be necessary to achieve stable fixation of the graft.
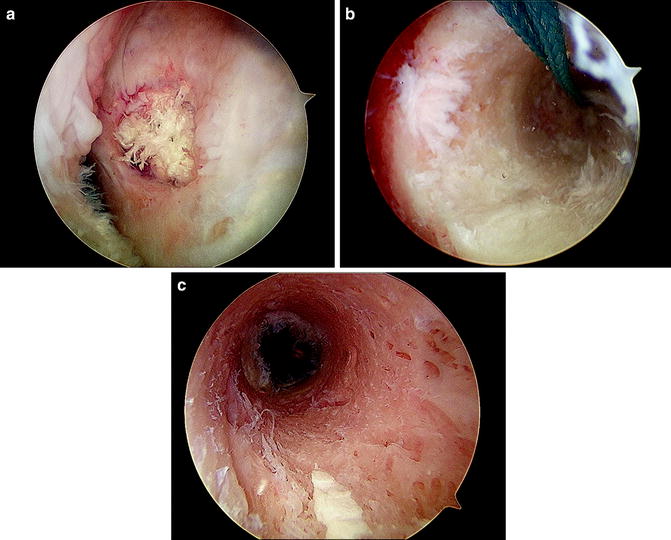
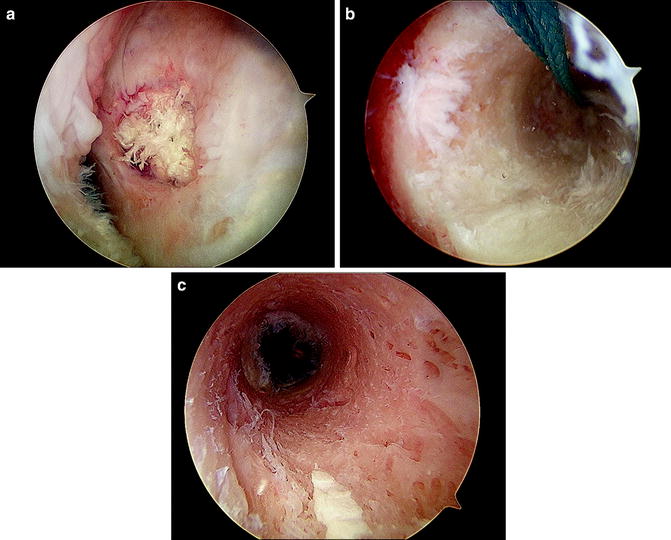
Fig. 12.3
(a) Arthroscopic view of ACL femoral tunnel in anatomic position, in which it is possible to re-use tunnel for revision. “Arthroscopic tunnel view” of femoral bone tunnel (b) and tibial tunnel (c) used to assess for adequate bony walls
If the tunnels are deemed to be sufficiently inaccurate and out of the range of anatomic insertion (Fig. 12.4), then the options include leaving previous hardware in place and working around the hardware to place the new tunnels in the anatomic position (Fig. 12.5). Removing the previous hardware would be the other option, but this may destabilize the new tunnel wall, leading to inadequate fixation of the new graft.






Fig. 12.4
Lateral X-ray showing a malpositioned femoral tunnel placed too anteriorly. If the tunnels are out of anatomic range, hardware may be retained and a new tunnel may be safely placed in an anatomic position
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree