Chapter 36. Senescent Ptosis
Kimberly A. Swartz, BA; Henry M. Spinelli, MD, FACS
INDICATIONS
Although there are many causes of ptosis, this chapter is limited to senescent, or involutional, causes of ptosis. It is important to confirm the ptosis is an isolated condition related to impairment of the upper eyelid retractor system, and not pseudoptosis secondary to conditions such as severe dermatochalasis, brow ptosis, hypertropia, blepharospasm, and enophthalmos. In cases of pseudoptosis, correction of the “ptosis” can often be achieved by addressing the primary cause.
PREOPERATIVE PREPARATION
To choose the correct ptosis-correcting procedure, degree of ptosis and levator function need to be assessed. Degree of ptosis is measured by assessing the distance from where the upper lid rests in primary gaze to the line bisecting the distance between the upper aspect of the papillary aperture and the iris: 1 to 2 mm signals mild ptosis, 3 to 5mm moderate ptosis, and more than 5 mm severe ptosis. Levator function is measured by subtracting the levator aperture in down gaze from the aperture in up gaze; 10 to 15 mm indicates good levator function, 6 to 9 mm fair function, and less than 5 mm poor function. Measurements of up, primary, and down gaze should be done while immobilizing the brow to eliminate compensatory brow action. If ptosis is mild and levator function is good, a procedure such as a tarsal conjunctival müllerectomy may be indicated. If ptosis is severe and levator function is poor, something more complex, such as a frontalis sling procedure, may be necessary, although such procedures are typically less satisfying than procedures that do not rely on exogenous muscle action.
ANESTHESIA
Local, monitored anesthesia care (MAC), or general anesthesia can be used for this procedure.
POSITION AND MARKINGS
Preoperatively, the endogenous lid fold is delineated. If a new lid fold is to be created, the desired fold, often chosen to match the contralateral fold, is marked. For this procedure, the patient is placed in the supine position with the ability to be sat upright.
Incision and Exposure
Local anesthetic with epinephrine should be infiltrated using a 27- to 30-gauge needle along the upper lid and the planned incision. Topical anesthetic, such as tetracaine, should be instilled. Next, a protective lens may or may not be put in place, depending on the surgeon’s preference. The incision that follows depends upon the procedure being performed and is discussed below.
DETAILS OF THE PROCEDURE
Tarsal Conjunctival Müllerectomy (Fasanella-Servat)
Tarsal conjunctival müllerectomy (Fasanella-Servat) is used for mild ptosis and is contraindicated in patients with dry eye syndrome or decreased tear production.
The upper lid is everted and the tarsal complex is clamped with 2 small, curved clamps, leaving 3 to 4 mm of tarsal plate. It is important to observe the sweeping contour of the upper lid and mimic this with the clamp placement. A monofilament suture is then passed from the skin to the conjunctiva and then woven lateral to medial below the clamps; at the end, the suture is brought back through the skin. Then, before or after the clamps are removed, the excess tissue above the suture line is resected. After the clamps have been removed, the lid is reverted, and the 2 ends of the suture are loosely tied together (Fig. 36-1).
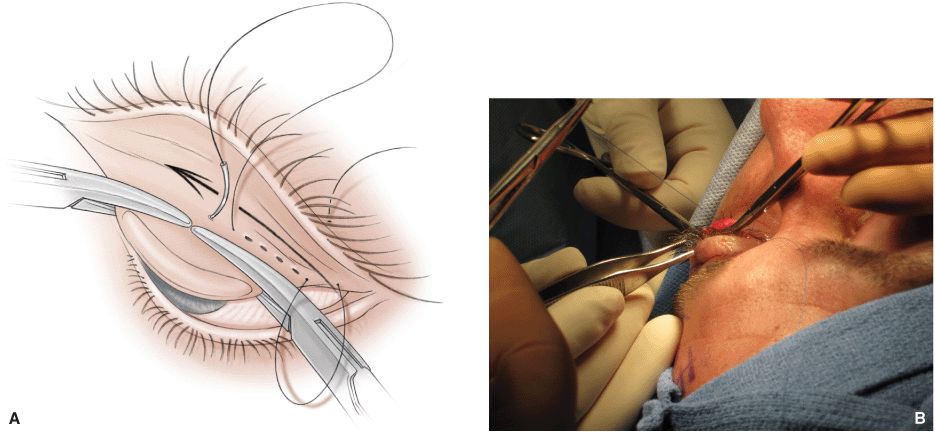
Figure 36-1 An illustration and intraoperative photograph demonstrating the clamping and suturing of the tarsal complex in a tarsal conjunctival müllerectomy.
Levator Tuck
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








