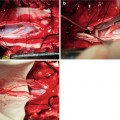
Fig. 6.1
Schematic diagram of selective sacral rhizotomy (a) group A; (b) group B; (c) group C; (d) group D
6.2.2.2 Operation Procedure
Proceed with intravenous anesthesia with 25 mg/kg 3 % barbitone sodium. Cut off the spinal cord of a dog at incision T8, and wait 10–20 days for the spastic bladder model to form (Fig. 6.2). Thereafter, anesthetize the dog with the same method as above. Then cut it open in the middle of the hypogastrium and put a No. 12 catheter in the bladder through the incision in the posterior urethra. Penetrate the receiving electrode of the Cantata 2000 electromyographic instrument (Dantec, Denmark) into the detrusor and sphincter’s sutured incision. The catheter is connected to a urodynamic pressure gauge, which measures the bladder capacity and urethral pressure. Then cut the L3–S4 nerve roots in the middle, resect the vertebral lamina on both sides so that the bilateral S2–4 nerve roots are revealed, and locate the nerve root anatomically (Fig. 6.3). Cut open the dural sac and carefully separate the sacral anterior root. Use an insulating rubber sheet to isolate the S2–4 nerve roots on both sides from the surrounding tissue to prevent bias caused by electrical stimulation.



Fig. 6.2
Cut off the spinal cord of a dog at incision T8 for the spastic bladder model to form

Fig. 6.3
Locate the nerve root of the dogs anatomically
6.2.2.3 Experimental Test Method
Before cutting off the nerve root, record urine flow mechanics and electrophysiology data from which will serve as the control. Selective cutting of the S2 anterior nerve root is marked as Group A, and carry out urodynamic testing to determine the urinary bladder capacity and urethral pressure. Stimulate the retained sacral nerve root with the single-phase square wave (115 mV, 1.0 ms) electric current of the same strength as that used in the control group. Use the Cantata 2000 electromyographic instrument to record the evoked potentials of the detrusor and sphincter’s motor nerve, and calculate the average of the wave crests. Stimulate the retained sacral nerve root with an electric current (1,200 mV, 10 Hz, 25 ms) of the same strength, and observe and record the bladder emptying and penile erectile function. Thereafter, sequentially cut off half of the S3 anterior nerve root, the rest of the S3 anterior nerve root and the S4 anterior nerve root. Conduct the same tests on Group B, Group C and Group D as those on Group A.
6.2.2.4 Statistics
Use a paired t test to analyze the urodynamic measured value and changes in electric potential wave crests evoked by muscular movement.
6.2.3 Results
6.2.3.1 Urodynamic Test
As more of the sacral nerve root was cut, bladder capacity increased gradually, bladder compliance obviously improved and urethral pressure was gradually reduced (Table 6.1). For these tests, the measured value of Group B was close to normal (180 ± 30 ml and 60 ± 10 cm H2O) and there was a significant difference between each group’s results (p < 0.05).
Table 6.1
Bladder capacity and urethral pressure test result (mean ± standard deviation)
Control group | Group A | Group B | Group C | Group D | |
|---|---|---|---|---|---|
Bladder capacity (ml) | 50 ± 20 | 150 ± 50 | 180 ± 30 | 230 ± 50 | 400 ± 40 |
Urethral pressure (cm H2O) | 90 ± 20 | 80 ± 10 | 60 ± 10 | 50 ± 10 | 30 ± 10 |
When the retained sacral nerve root is stimulated with a single-phase square wave of the same intensity, there was no obvious difference in the detrusor-motion-evoked electric potential wave crest between the control group and Groups A and B (Table 6.2) (P > 0.05), while results in Groups C and D obviously decreased and exhibited remarkable differences from the other three groups.
Table 6.2
Detrusor sphincter peak potential, examination results (mean ± standard deviation) (mV)
Control group | Group A | Group B | Group C | Group D | |
|---|---|---|---|---|---|
Detrusor | 11.5 ± 3.2 | 11.3 ± 2.62* | 11.2 ± 2.52* | 8.6 ± 1.45 | 3.5 ± 1.23 |
Sphincter | 11.2 ± 2.3 | 10.5 ± 2.78 | 8.32 ± 2.34 | 6.5 ± 3.14 | 3.13 ± 1.34 |
6.2.3.2 Urination and Erectile Function Test
With the electric current of same intensity stimulating the sacral nerve root of the sample from each group, the bladder voiding volume result (Table 6.3) illustrates that appropriately cutting off a certain number of sacral nerve roots can significantly increase the bladder urine output, while cutting off too much significantly reduces the urine output. The Group B urine volume increased significantly. Differences in micturition volume between those groups were significant (p < 0.05). Penile erectile function was lost by 1 dog each and maintained in the rest of the dogs in Groups A and B, reduced or weakened in Group C, and completely lost in Group D.
Table 6.3
Voiding of the bladder and erectile function (mean ± standard deviation) (ml)
Control group | Group A | Group B | Group C | Group D |
|---|