Sebaceous and sweat glands – Acne, rosacea and other disorders
Acne
 increased sebum excretion – seborrhoea (greasy skin)
increased sebum excretion – seborrhoea (greasy skin)
 pilosebaceous duct hyperkeratosis and comedone formation
pilosebaceous duct hyperkeratosis and comedone formation
 colonization of the duct with Propionibacterium acnes
colonization of the duct with Propionibacterium acnes
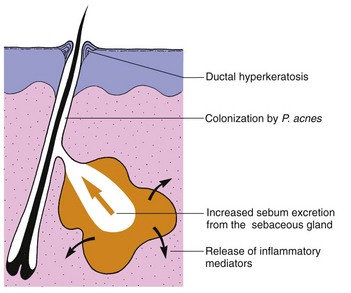
In acne, the androgen-sensitive pilosebaceous unit (p. 4) shows a hyper-responsiveness that results in increased sebum excretion. Factors in sebum induce comedones, and P. acnes initiates inflammation through chemical mediators inducing enzymes (e.g. lipase) and prostaglandins (Fig. 1).
Clinical presentation
Comedones are either open (blackheads: dilated pores with black plugs of melanin-containing keratin) or closed (whiteheads: small cream-coloured, dome-shaped papules). They appear at about the age of 12 years and evolve into inflammatory papules (Fig. 2), pustules or cysts (Fig. 3). The sites of predilection – the face, shoulders, back and upper chest – have many sebaceous glands. The severity of acne depends on its extent and the type of lesion, with cysts being the most destructive.
Acne usually persists until the early twenties, although in a few patients, particularly women, the disease continues into the fifth decade. Scars may follow healing, especially of cysts or abscesses. Scars may be ‘ice-pick’, atrophic (Fig. 4) or keloidal.
Some variants of acne are seen:
 Acné excoriée: due to squeezing, affects depressed or obsessional young women.
Acné excoriée: due to squeezing, affects depressed or obsessional young women.
 Chloracne: caused by systemic toxicity of certain aromatic halogenated industrial chemicals.
Chloracne: caused by systemic toxicity of certain aromatic halogenated industrial chemicals.
 Conglobate: a mass of burrowing abscesses and sinuses with scarring.
Conglobate: a mass of burrowing abscesses and sinuses with scarring.
 Cosmetic: pomade and cosmetic-induced comedonal and papular acne (mainly seen in the USA).
Cosmetic: pomade and cosmetic-induced comedonal and papular acne (mainly seen in the USA).
 Drug-induced: by systemic steroids, androgens and topical steroids.
Drug-induced: by systemic steroids, androgens and topical steroids.
 Infantile: mostly found on the faces of male infants; cause unknown.
Infantile: mostly found on the faces of male infants; cause unknown.
 Physical: occlusion by the back of a wheelchair or on a violinist’s chin.
Physical: occlusion by the back of a wheelchair or on a violinist’s chin.