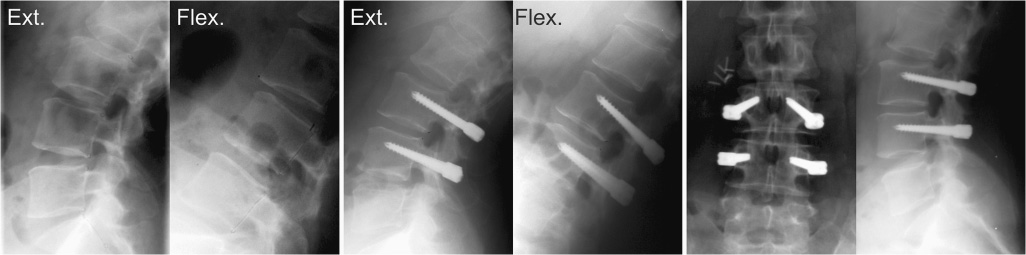
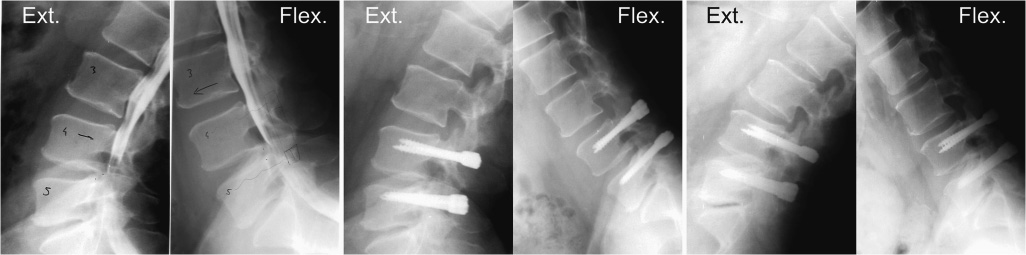
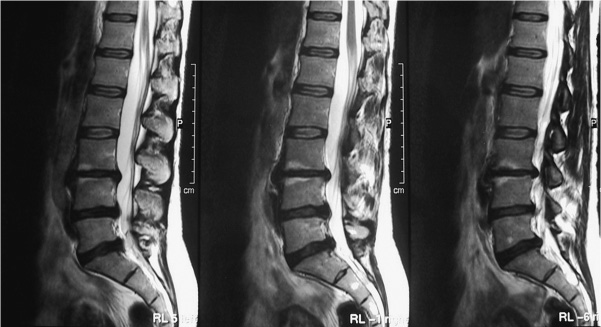
38 During the course of the natural evolution of vertebral disk degeneration starting from incipient diskopathy up to stenosis with fixed terminal deformation, the functional tripod (disk and facets) will experience a long period of destabilization with abnormal movements. Dynamic stabilization with the Dynesys Dynamic Stabilization System (Zimmer Spine, Inc., Warsaw, IN) provides distinct benefits (Fig. 38–1) in the phase of degeneration where symptoms are caused by diskovertebral dyskinesis; that is, between early stages of symptomatic degenerative changes of the spinal segment and structural deformities associated with spontaneous ossification. The goal of dynamic stabilization with Dynesys is to realign and stabilize one or more intervertebral lumbar or lumbosacral segments in a position close to the normal anatomical position, with the intent of encouraging return to improved intervertebral physiology while enabling a certain degree of range of motion. Figure 38–1 Functional model of Dynesys. At the present time, more than 15,000 surgical procedures have been performed in over 15 different countries. The longest follow-up period is 10 years. To achieve this goal, Zimmer has developed a dynamic stabilization system called Dynesys (Dynamic Neutralization System for the Spine). The Dynesys system consists of titanium alloy (Protasul 100) pedicle screws, polyester (Sulene-PET) cords and polycarbonateurethane (Sulene-PCU) spacers. The cord and the spacer meet the International Standards Organization (ISO) 10993 international standards and the pedicle screws fulfill those of ISO 5822–11. The cord controls the range of motion in flexion, whereas the spacer limits extension movements, enabling the posterior elements to be repositioned in accordance with a near normal anatomical situation. All individual components and interconnections were tested for their static as well as for their dynamic behavior to assess the safety of the system. Fatigue testing of the complete assembly was performed to 10 million cycles, which is believed to represent a time in vivo of approximately 5 years. In an initial phase (1–2 million cycles), the system showed stress relaxation and remained stable at a substantial load level afterward. Several biomechanical in vitro experiments were conducted to study the efficacy of the system. One recently published study tested six lumbar cadaver spines, loading them with pure moments in the three motion planes.1 The spines were tested intact, with a defect of the middle segment, stabilized with Dynesys, and fixed with an internal fixator. For the instrumented segment, Dynesys stabilized the spine and was more flexible than the internal fixator, particularly in extension where Dynesys restored the range of motion to the intact condition. A second in vitro study found that increased spacer length increased the mobility in the segment.2 Figure 38–2 Female patient, 40 years old at time of surgery, presenting with degenerative disk disease in combination with spondylolisthesis. Dynesys was implanted without any additional surgical procedure. X-rays show preoperative and immediate postoperative functional x-rays and anteroposterior and lateral x-rays 9 years postoperatively. These biomechanical studies have confirmed that the stiffness of an instrumented segment was close to that of an intact spinal column. It therefore reinstates stiffness of the destabilized spinal segment on an experimental basis to a degree close to that of a normal and intact spine. This internal bracing device enables the posterior elements, annulus, and posterior longitudinal ligament to be retensioned. It repositions the articulating surfaces to the areas in which they function normally, suppresses dyskinetic movements caused by loss of viscoelasticity of the disk, and restores the posterior pretensioning. It thus brings about anatomical conditions of the intervertebral joint that enable restoration of a better diskovertebral physiology, allowing a certain degree of freedom to be preserved due to the elasticity of the spacer. It limits the impact of the biomechanical stresses on the adjacent levels. This device shows some potential for healing to take place in the disk space as well as in the end plates (see Performance). The indications for Dynesys are based upon their design and biomechanical effects. Dynesys addresses instabilities of all kinds: excessive or pathological motion and gradually developing deformity, including iatrogenic instability. This may involve low back pain as well as neurogenic pain. The main goal of Dynesys is to address dynamic instability with autoreducible lesions in the early stages of degeneration as defined by Kirkaldy-Willis.3 As a result of the instability, the patient may experience several types of clinical symptoms. These include dynamic stenosis or stenosis with degenerative olisthesis as evidenced by either or both neurogenic pain and low back pain (Fig. 38–2).Other indications for Dynesys are mono- or multisegmental degenerative disk disease (DDD) causing low back pain (Fig. 38–3) as well as iatrogenic instability following decompression. In multilevel DDD, Dynesys may also be combined with a fusion procedure such as posterior lumbar interbody fusion (PLIF), depending on the severity of segmental disk disruption. Dynesys is not indicated as a primary stabilization method in lytic (isthmic) spondylolisthesis and severe degenerative scoliotic or kyphotic deformation. The surgical approach is along the median line, opening the lumbar aponeurosis, rasping the paravertebral muscles if the surgeon wishes to carry out intracanal activities aimed at associated decompression at the same time as the dynamic stabilization procedure. If no intracanal procedure is needed and if the lesion is of the dynamic stenosis type due to a soft lesion, then an intermuscular bilateral approach according to Wiltse or an intermuscular paraspinal approach can be performed. This approach does not interfere with the posterior muscles or the lumbar aponeurosis and provides direct access to the articular–transverse junction without interfering with the articulating surface and its capsule. It also enables the screw to be implanted at an angle that is almost always perfect. Figure 38–3 Male patient, 48 years old at time of surgery, presenting with permanent stenosis. Dynesys was implanted after recalibration of the affected level. Functional x-rays preoperatively, immediately postoperatively, and 6 years postoperatively. Figure 38–4 Female patient, 40 years old at time of surgery, presenting with Modic I signs at L3–L4, black disk on three levels, and positive diskogram at L3–L4 only. (Image provided by C. Crawshaw, Gloucester, U.K.) Whatever approach is used, it is important not to interfere with the articular processes and their capsule. The point of intrapedicular penetration must be located at the external junction of the articular and transverse surfaces.
Treatment of Mobile Vertebral
Instability with Dynesys
Technical Aspects
Indications
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Technical Aspects
Technical Aspects Indications
Indications Surgical Technique
Surgical Technique Performance
Performance Clinical Results
Clinical Results Discussion
Discussion Conclusion
Conclusion