, Madan Ethunandan2 and Tian Ee Seah3
(1)
Poole Hospital NHS Foundation Trust, Poole, Dorset, UK
(2)
Department of Oral and Maxillofacial Surgery, University Hospital Southampton NHS Trust Southampton General Hospital, Southampton, UK
(3)
Orange Aesthetics and Oral Maxillofacial Surgery, Singapore, Singapore
Subunits and Anatomical Considerations
The skin of the scalp is amongst the thickest in the body and relatively inelastic. It is hair bearing and covers a convex area, which can all add up to difficulties in reconstruction. The acronym “SCALP” represents S – skin, C – subcutaneous tissue, A – galea aponeurotica, L – loose areolar tissue, and P – pericranium (Fig. 5.1). The blood vessels and nerves run within the galeal layer, which connects the frontalis and occipitalis muscles. In the temple region (below the temporal line), the terminology of the scalp layers becomes potentially confusing (Fig. 5.2). This can be more easily appreciated, if one was to consider the temporalis fascia (deep temporal fascia) to be an extension of the pericranium and the overlying galea, as the temporoparietal fascia (superficial temporal fascia, suprazygomatic SMAS). Not surprisingly, the vessels and nerves lie within the temporoparietal fascia. A few centimetres above the zygomatic arch, the temporalis fascia divides into two layers (superficial and deep layers of the deep temporal fascia) enclosing the superficial temporal fat pad. The temporoparietal fascia fuses with the superficial layer of the deep temporal fascia and the periosteum of the zygomatic arch. The frontal branch of the facial nerve, present in the temporoparietal fascia, is liable to damage, as it crosses the zygomatic arch if its location is not appreciated.
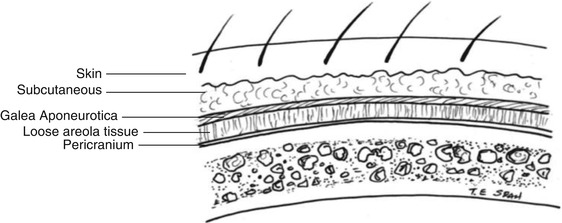
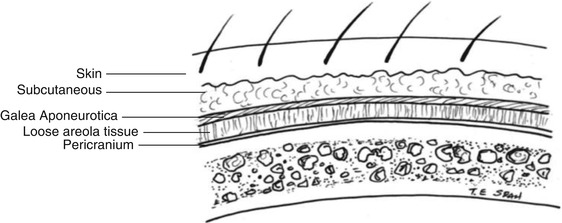
Fig. 5.1
Layers of the scalp
Fig. 5.2
Scalp layers in the central and temporal regions
The scalp covering the vertex (central) is tight and poorly distensible. This is thought to be due to the thick galea and no underlying muscle, whereas the scalp overlying the temporal and parietal regions (lateral) is relatively more loose and is thought to be due to the thin galea and the presence of an underlying temporalis muscle (Figs. 5.3 and 5.4).
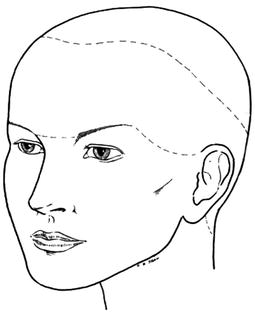
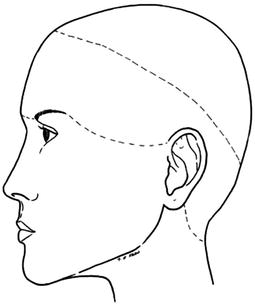
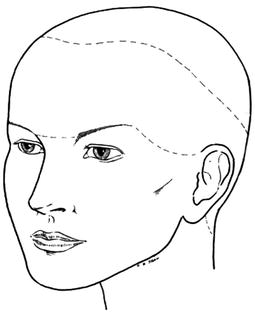
Fig. 5.3
Tight and loose regions of the scalp
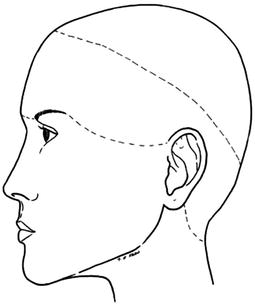
Fig. 5.4
Tight and loose regions of the scalp
The scalp has a rich vascular supply, which is provided by the superficial temporal, posterior auricular, occipital arteries (branches of the external carotid) and the supraorbital and supra-trochlear arteries (branches of the internal carotid). The sensory supply is by the supratrochlear, supraorbital, zygomaticotemporal, auriculotemporal, lesser occipital (C2), greater occipital (C2) and third occipital (C3) nerves. The vessels and nerves run within the galea/temporoparietal fascia (Fig. 5.5).
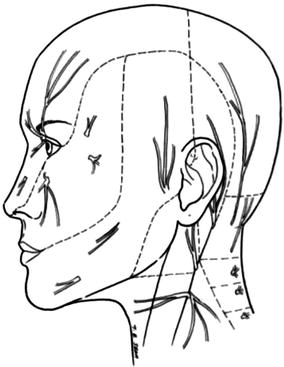
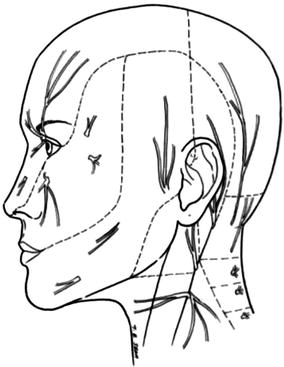
Fig. 5.5
Sensory nerve supply of the scalp
Scalp flaps can be raised easily in the subgaleal plane, which provides a relatively avascular and quick layer for dissection. Subcutaneous dissection, on the other hand, is more difficult and has to be carried out by sharp dissection, as there is no “natural” plane to work with. Incisions should be made parallel to the hair follicles and injudicious use of diathermy avoided to minimise damage to the hair follicles and risk of alopecia. Because of their relative inelasticity, scalp flaps will have to be large in relation to the defect, to achieve closure without excessive tension.
Central (Vertex) Defects
Small Defect
Small defects are amenable to primary closure. Wide undermining in the subgaleal plane is often required, to achieve closure. If necessary, small areas can be left to heal by secondary intention.
Medium-Sized Defects
The primary and secondary defects can be often closed primarily, though on occasions, the secondary defect is covered by a skin graft in a less conspicuous location.
Rotation Flap
Indications
Circular defect and defects which can be converted to a triangle.
Technique
A curvilinear incision is made, from the base of the defect, and the flap is raised in the subgaleal plane. The length of the flap is designed to be at least six times the width of the defect. The margins of the defect are widely undermined, and, if necessary, the galea is scored to gain additional extensibility of the flap. Care should however be taken, not to compromise the vascular supply, by damaging the vessels that run within the galea. A back cut can be employed to decrease the tension of closure, but again care must be taken to avoid vascular compromise. The dog-ear often settles with time and can be corrected at a later date if necessary. The wounds are closed in layers and a pressure dressing/drain employed as necessary (Fig. 5.6a–c).
Tips
For large defects, the orientation of the incision can be modified to include named vessels in the flap to improve vascularity. The distribution of hair and hairline should also be taken into account, when planning the incision. It is important to appreciate the difference in length (outer greater than inner) and thickness (raised flap thinner than native lateral margins) of the two flap margins, and this would have to be accommodated in the suturing technique. The drain is ideally placed away from the base of the flap.
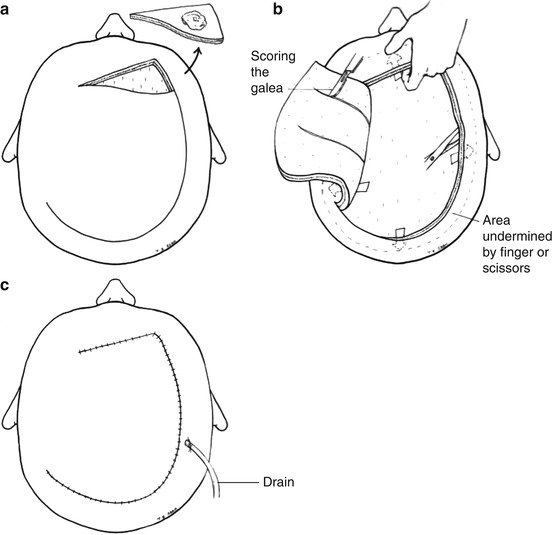
Fig. 5.6
Scalp rotation flap
O-Z Closure









