CHAPTER 28 Rupture of the Anterior Tibial Tendon
A very reasonable alternative is to insert the tendon into the navicular. For some years I performed a rerouting of the ATT (a modified Young procedure) for management of the adult flatfoot deformity. This was particularly useful if previous surgery for a flexible flatfoot deformity had failed. In this procedure, the ATT is not detached distally but is rerouted under the navicular to support the medial arch of the foot. What I observed is that there is no loss of dorsiflexion strength, and the transfer takes advantage of the slight inversion function of the ATT. Therefore, in the presence of a rupture of the ATT, and particularly if the foot is flat, I am inclined to insert the tendon into the navicular. This repair is very effective in cases in which retraction of the tendon is minimal but not enough length is available to reattach it distally into the cuneiform (Figure 28-1).
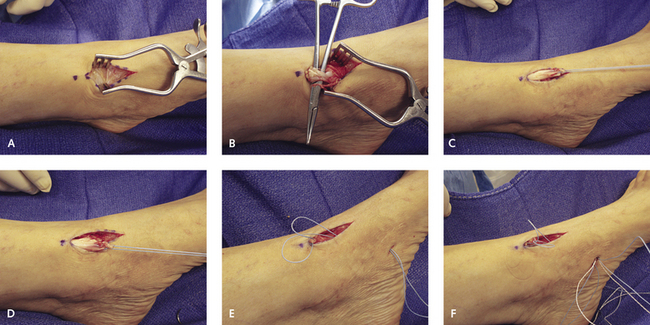
With this technique, I make a 2-cm incision over the dorsum of the midfoot in order to retrieve the stump of the anterior tibial tendon. A puncture is then made over the navicular to insert a suture anchor, which is done under fluoroscopic guidance to ensure correct positioning of the anchor. The sutures at the tip of the stump of the tendon are then passed subcutaneously out of the puncture incision used for the anchor. The sutures from the anchor are then passed subcutaneously into the longitudinal incision, with needles attached, and through the tendon. The tension on the tendon is maximized by simultaneously pulling the sutures on the stump out distally through the puncture (see Figure 28-1).
If fixed clawing of the hallux is present as a result of accessory use of the EHL and extensor digitorum longus (EDL) tendons, then an arthrodesis of the hallux interphalangeal joint is ideal, and the EHL tendon can be used to augment the repair (Figure 28-2). A tendon graft works well in this instance, but it should be supplemented possibly with an EHL tenodesis to strengthen the repair. Positioning the foot in at least 10 degrees of dorsiflexion at the completion of the repair regardless of the technique is important.
The main problem with the final repair is the potential for wound dehiscence. Bowstringing of the repair always occurs, and because the extensor retinaculum is potentially deficient at the completion of the repair, the underlying skin is subjected to increased pressure from the repaired tendon. For this reason, I make the skin incision more lateral than the underlying repair and then raise the skin flap so that with closure, no pressure from the tendon is on the actual incision (Figure 28-3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree