Chapter 15 Rotational and Free Flap Closure of the Abdominal Wall ![]()
1 Preoperative Considerations
1 Comorbidities
 Skin and subcutaneous fat may be of varying thicknesses and qualities in patients because of body habitus, scarring, steroid use, malnutrition, advanced age, and other factors.
Skin and subcutaneous fat may be of varying thicknesses and qualities in patients because of body habitus, scarring, steroid use, malnutrition, advanced age, and other factors.2 Open Wound Management
 Appropriate dressings should be applied to the wound before surgery to prevent desiccation of the soft tissues and intraabdominal contents.
Appropriate dressings should be applied to the wound before surgery to prevent desiccation of the soft tissues and intraabdominal contents. Negative pressure dressings allow for easier management of large abdominal wounds, but the wound must be monitored closely when the dressing is applied over exposed bowel.
Negative pressure dressings allow for easier management of large abdominal wounds, but the wound must be monitored closely when the dressing is applied over exposed bowel. Some wounds require frequent debridements to determine the extent of viable tissue and clearance of infection.
Some wounds require frequent debridements to determine the extent of viable tissue and clearance of infection.3 Timing
 Optimize the patient before closure of the abdominal wall in regard to nutrition, cardiovascular status, and pulmonary function. The closure may lead to prolonged intubation, and this risk is increased in patients with chronic obstructive pulmonary disease (COPD) and smokers.
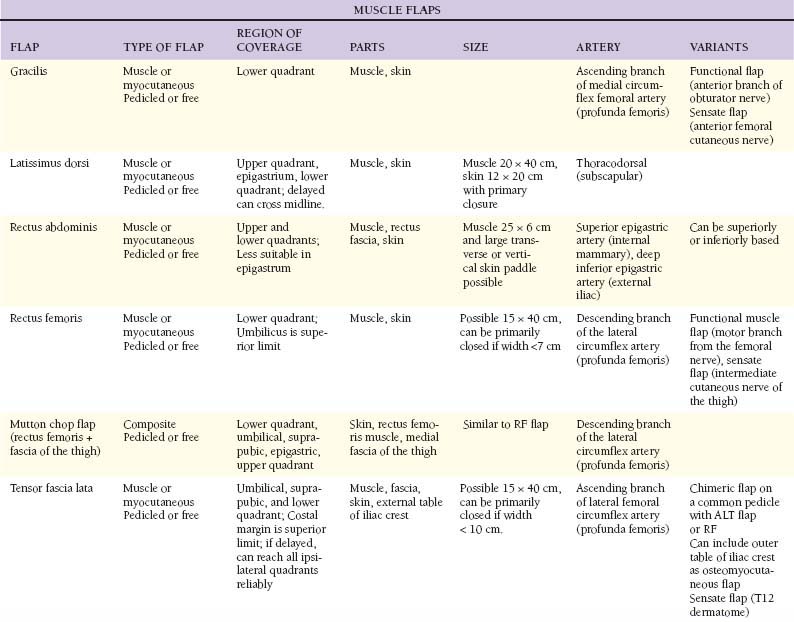
Optimize the patient before closure of the abdominal wall in regard to nutrition, cardiovascular status, and pulmonary function. The closure may lead to prolonged intubation, and this risk is increased in patients with chronic obstructive pulmonary disease (COPD) and smokers.2 Muscular Flaps (Table 15-1)
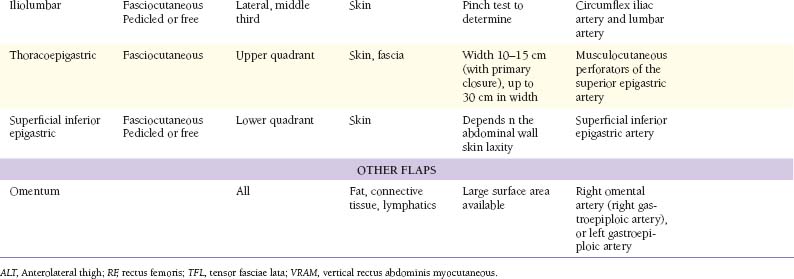
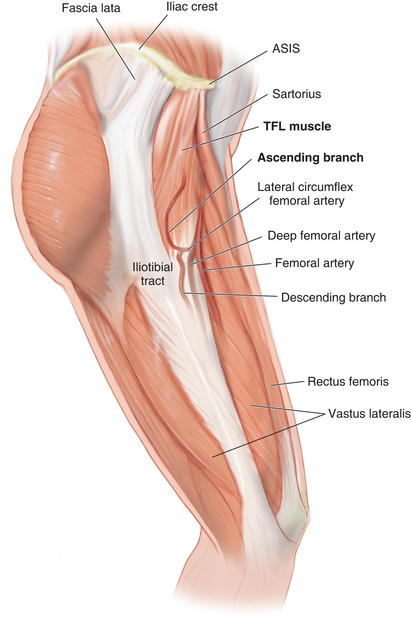
 Figure 15-1 shows the cross-sectional anatomy of the thigh demonstrating the possible muscles for coverage of abdominal wall defects
Figure 15-1 shows the cross-sectional anatomy of the thigh demonstrating the possible muscles for coverage of abdominal wall defects1 Tensor fascia lata
 Anatomy
Anatomy
 Sensory innervation includes the lateral cutaneous branch of the twelfth thoracic nerve and the lateral cutaneous sensory nerve of the thigh (L2 and L3). Motor innervation is supplied by the distal branch of the superior gluteal nerve (L4 and L5).
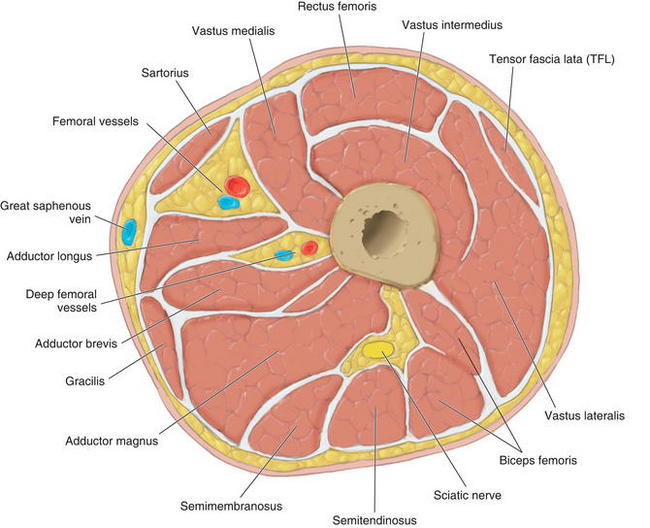
Sensory innervation includes the lateral cutaneous branch of the twelfth thoracic nerve and the lateral cutaneous sensory nerve of the thigh (L2 and L3). Motor innervation is supplied by the distal branch of the superior gluteal nerve (L4 and L5). Arterial blood supply is from the ascending branch of the lateral femoral circumflex artery, which is 1.5 to 2.5 mm diameter. The vein is slightly larger than the artery when traced to the origin on the lateral femoral circumflex.
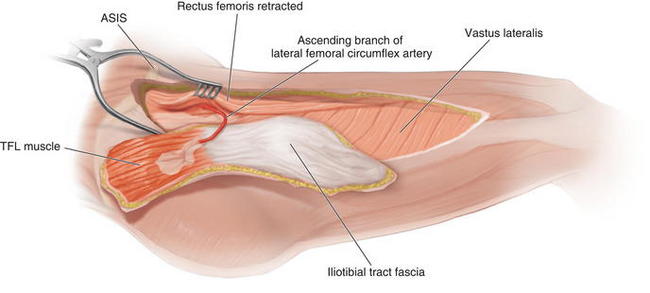
Arterial blood supply is from the ascending branch of the lateral femoral circumflex artery, which is 1.5 to 2.5 mm diameter. The vein is slightly larger than the artery when traced to the origin on the lateral femoral circumflex. Pedicle length can be up to 10 cm. The pedicle enters the tensor fasciae lata (TFL) muscle at the level of the junction of the proximal and middle thirds of an axis drawn from the anterior superior iliac spine (ASIS) to the lateral aspect of the patella. It emerges from beneath the rectus femoris muscle, anterior to the vastus lateralis and enters the muscle via the deep surface medially 6 to 8 cm from the ASIS.
Pedicle length can be up to 10 cm. The pedicle enters the tensor fasciae lata (TFL) muscle at the level of the junction of the proximal and middle thirds of an axis drawn from the anterior superior iliac spine (ASIS) to the lateral aspect of the patella. It emerges from beneath the rectus femoris muscle, anterior to the vastus lateralis and enters the muscle via the deep surface medially 6 to 8 cm from the ASIS. The descending branch of the lateral femoral circumflex artery continues beyond the TFL muscle to supply the skin of the anterolateral midthigh and the lower thigh. It can be harvested with the anterolateral thigh skin to enlarge the perfused vascular territory.
The descending branch of the lateral femoral circumflex artery continues beyond the TFL muscle to supply the skin of the anterolateral midthigh and the lower thigh. It can be harvested with the anterolateral thigh skin to enlarge the perfused vascular territory. The TFL muscle (Fig. 15-2) is a short, flat muscle that is approximately 12 to 15 cm long. It acts as an accessory flexor and medial rotator of the thigh. It originates from the anterior iliac crest and the deep surface of the fascia lata. At the origin, it lies between the gluteus medius and sartorius, and superficial to the vastus lateralis. It inserts into the iliotibial tract, which inserts distally on Gerdy’s tubercle on the lateral aspect of the tibia.
The TFL muscle (Fig. 15-2) is a short, flat muscle that is approximately 12 to 15 cm long. It acts as an accessory flexor and medial rotator of the thigh. It originates from the anterior iliac crest and the deep surface of the fascia lata. At the origin, it lies between the gluteus medius and sartorius, and superficial to the vastus lateralis. It inserts into the iliotibial tract, which inserts distally on Gerdy’s tubercle on the lateral aspect of the tibia. The fascia lata is the deep fascia of the thigh. It thickens to form the iliotibial tract laterally and attaches distally to the lateral condyle of the tibia. The TFL muscle is enclosed by the fascia lata, and distally, the muscle fibers coalesce with the iliotibial tract in the middle third of the thigh. The thickness of the fascia lata over the TFL muscle makes it a strong fascial donor site suitable for reconstructing abdominal wall defects.
The fascia lata is the deep fascia of the thigh. It thickens to form the iliotibial tract laterally and attaches distally to the lateral condyle of the tibia. The TFL muscle is enclosed by the fascia lata, and distally, the muscle fibers coalesce with the iliotibial tract in the middle third of the thigh. The thickness of the fascia lata over the TFL muscle makes it a strong fascial donor site suitable for reconstructing abdominal wall defects. Flap Design
Flap Design
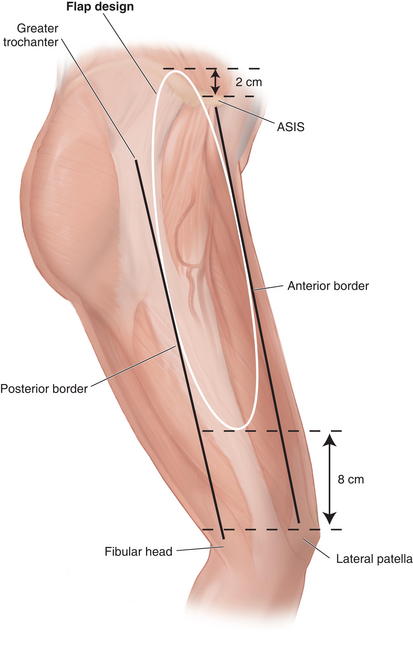
 Skin territory can be up to 15 × 40 cm. A line from the ASIS 10 to 15 cm posteriorly marks the origin of the TFL muscle, with the skin territory extending 2 cm cranial to this line (Fig. 15-3). The lower skin territory is 8 cm above the lateral femoral condyle. Posterior skin territory is a line drawn from the greater trochanter to the fibular head or approximately along the axis of the femur. The anterior border is a line drawn from the ASIS to the lateral aspect of the patella.
Skin territory can be up to 15 × 40 cm. A line from the ASIS 10 to 15 cm posteriorly marks the origin of the TFL muscle, with the skin territory extending 2 cm cranial to this line (Fig. 15-3). The lower skin territory is 8 cm above the lateral femoral condyle. Posterior skin territory is a line drawn from the greater trochanter to the fibular head or approximately along the axis of the femur. The anterior border is a line drawn from the ASIS to the lateral aspect of the patella. The entry point of the pedicle is at the level of the junction of the proximal and middle third of the line or 6 to 8 cm from the ASIS.
The entry point of the pedicle is at the level of the junction of the proximal and middle third of the line or 6 to 8 cm from the ASIS. The rotation arc of the pedicled flap reaches the costal margin if the tensor muscle is completely detached from its origin and raised as an island flap.
The rotation arc of the pedicled flap reaches the costal margin if the tensor muscle is completely detached from its origin and raised as an island flap. Marking and Dissection
Marking and Dissection
 The flap is marked as an ellipse over the axis of the TFL muscle and to incorporate the pedicle proximally.
The flap is marked as an ellipse over the axis of the TFL muscle and to incorporate the pedicle proximally. As dissection proceeds cranially, the space between the rectus femoris and vastus lateralis is retracted with a self-retaining retractor to identify the descending branch of the lateral femoral circumflex artery.
As dissection proceeds cranially, the space between the rectus femoris and vastus lateralis is retracted with a self-retaining retractor to identify the descending branch of the lateral femoral circumflex artery. Postoperative Care
Postoperative Care
 The donor site can be closed primarily if planned appropriately. Skin graft may be needed for larger flaps including skin.
The donor site can be closed primarily if planned appropriately. Skin graft may be needed for larger flaps including skin.2 Latissimus dorsi
 The latissimus dorsi is the largest muscle in the body (up to 20 × 40 cm), but it is quite thin (<1 cm thick). It acts as a humeral adductor and internal rotator, and no significant functional deficit results from harvest. It has six origins, from the lower six thoracic spines and supraspinatus ligaments, posterior layer of lumbar fascia, tendinous attachments of the iliac crest, strips of muscle interdigitating with the external oblique, muscular slips from lower four ribs, and muscular slips from the scapula. The upper and anterior borders are free. The latissimus is deep to the trapezius. It inserts at the floor of bicipital groove of the humerus behind the tendon of the long head of the biceps. The latissimus forms the posterior fold of the axilla with the subscapularis tendon.
The latissimus dorsi is the largest muscle in the body (up to 20 × 40 cm), but it is quite thin (<1 cm thick). It acts as a humeral adductor and internal rotator, and no significant functional deficit results from harvest. It has six origins, from the lower six thoracic spines and supraspinatus ligaments, posterior layer of lumbar fascia, tendinous attachments of the iliac crest, strips of muscle interdigitating with the external oblique, muscular slips from lower four ribs, and muscular slips from the scapula. The upper and anterior borders are free. The latissimus is deep to the trapezius. It inserts at the floor of bicipital groove of the humerus behind the tendon of the long head of the biceps. The latissimus forms the posterior fold of the axilla with the subscapularis tendon. Blood Supply
Blood Supply
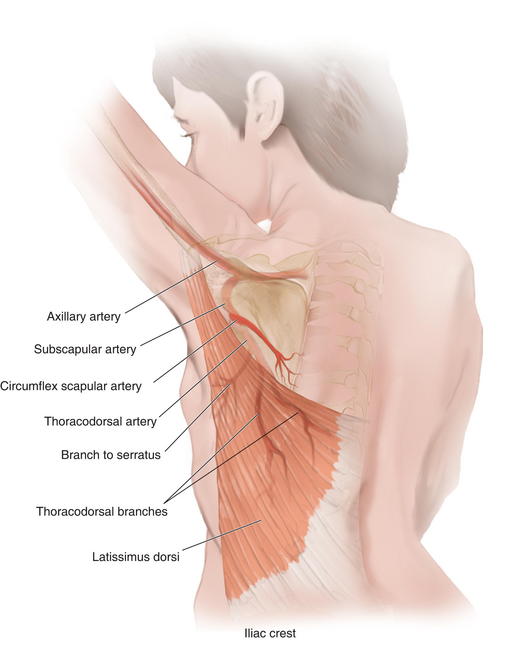
 Arterial blood is supplied through a terminal branch of the subscapular artery (2 to 5 mm diameter), a branch of the axillary artery.
Arterial blood is supplied through a terminal branch of the subscapular artery (2 to 5 mm diameter), a branch of the axillary artery. After 5 cm, the subscapular artery gives off the circumflex scapular branch posteriorly and the thoracodorsal artery (2 to 4 mm diameter) (Fig. 15-5).
After 5 cm, the subscapular artery gives off the circumflex scapular branch posteriorly and the thoracodorsal artery (2 to 4 mm diameter) (Fig. 15-5). The thoracodorsal artery courses along the posterior aspect of the axilla for 8 to 14 cm and gives off 1 to 2 branches to the serratus before it enters the latissimus dorsi muscle on its deep surface. The serratus branch can be kept to include the serratus as part of a chimeric flap. The artery divides in the substance of the muscle into vertical and transverse branches and can facilitate a split flap.
The thoracodorsal artery courses along the posterior aspect of the axilla for 8 to 14 cm and gives off 1 to 2 branches to the serratus before it enters the latissimus dorsi muscle on its deep surface. The serratus branch can be kept to include the serratus as part of a chimeric flap. The artery divides in the substance of the muscle into vertical and transverse branches and can facilitate a split flap. Thoracic intercostal and lumbar perforating arteries enter the deep surface of the muscle 8 cm from the posterior midline at the level of the seventh, ninth, and eleventh vertebral spines. They perfuse the inferior and medial latissimus.
Thoracic intercostal and lumbar perforating arteries enter the deep surface of the muscle 8 cm from the posterior midline at the level of the seventh, ninth, and eleventh vertebral spines. They perfuse the inferior and medial latissimus. Flap Design
Flap Design
 The flap design can cover ipsilateral abdominal defects. If raised as an “extended” variant, it can cross the midline by incorporating the rim of supragluteal fascia.
The flap design can cover ipsilateral abdominal defects. If raised as an “extended” variant, it can cross the midline by incorporating the rim of supragluteal fascia. If based at the muscle insertion, the pivot point is at the level of the midposterior axillary line.
If based at the muscle insertion, the pivot point is at the level of the midposterior axillary line. If the insertion is incised, the island flap pivot point is 1.5 to 2 cm inferior to the pectoral humeral junction.
If the insertion is incised, the island flap pivot point is 1.5 to 2 cm inferior to the pectoral humeral junction. The skin paddle can be as large as 5 cm anterior and inferior to the muscle without delay and can be made larger with a delay procedure.
The skin paddle can be as large as 5 cm anterior and inferior to the muscle without delay and can be made larger with a delay procedure. Marking and Dissection
Marking and Dissection
 The outline of the anterior and superior edges of the muscle is made. This can be facilitated by having the patient contract the latissimus.
The outline of the anterior and superior edges of the muscle is made. This can be facilitated by having the patient contract the latissimus. If a muscle only flap needed, the incision is marked extending from the posterior axillary fold, then inferiorly and posteriorly over the anterior boarder of the latissimus muscle as dictated by the length of the muscle.
If a muscle only flap needed, the incision is marked extending from the posterior axillary fold, then inferiorly and posteriorly over the anterior boarder of the latissimus muscle as dictated by the length of the muscle.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree