CHAPTER 10 Role of Surgery in the Treatment of Varicose Veins
Basis and Aim of Surgery
In practice the aim is twofold:
The Different Surgical Procedures
Surgery without saphenous trunk preservation
Principle and Controversies
Technical Information
Conventional surgery variants
Saphenous Trunk Stripping with Preservation of Saphenofemoral Confluence, with or without Incompetent Tributary Phlebectomy and/or Incompetent Perforator Interruption
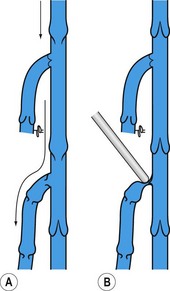
Non-flush ligation at the SFJ and/or SPJ was, until recently, described as a technical mistake responsible for in situ recurrence in all cases as reflux through the incompetent terminal valve persisted. But preoperative ultrasound investigations have proved that in GSV varices the terminal valve is competent in approximately half the patients.11,12
In this situation it looks obvious that high flush tie is not recommended as tributaries of the saphenofemoral confluence can drain in a physiologic way into the common femoral vein. Besides neovascularization, elimination of normal physiologic reflux is the main cause of recurrence after flush ligation,13 but rarely identified after confluence conservation.14
When the terminal valve is incompetent, non-flush ligation was thought to promote recurrence, as previously stated (Fig. 10.4). However, one prospective study has demonstrated that this concept is wrong. In this large series neither postoperative outcome nor clinical and diagnostic evaluation found a difference in terms of recurrence if the terminal valve was competent or not.14
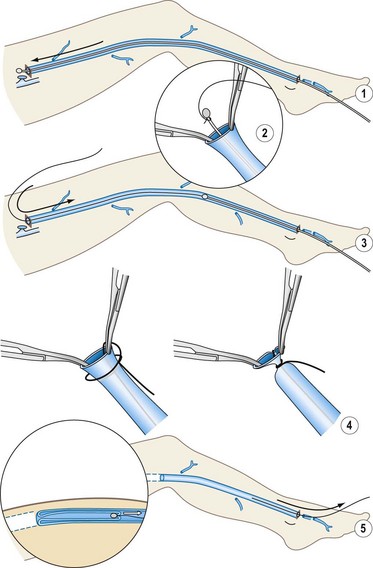
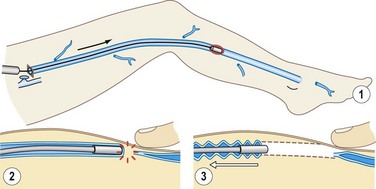
Cryostripping
The only difference with cryostripping in comparison to classical surgery is the ablation modality of the saphenous trunk. After HL, the saphenous trunk is catheterized downward with the cryoprobe until reaching the lower limit of the vein to be stripped. The generator is activated and when the vein is attached to the cryoprobe (by freezing to it) the vein is broken off easily. No distal ligation is needed and the vein attached to the probe is progressively pulled up and extracted through the groin incision (Fig. 10.5).
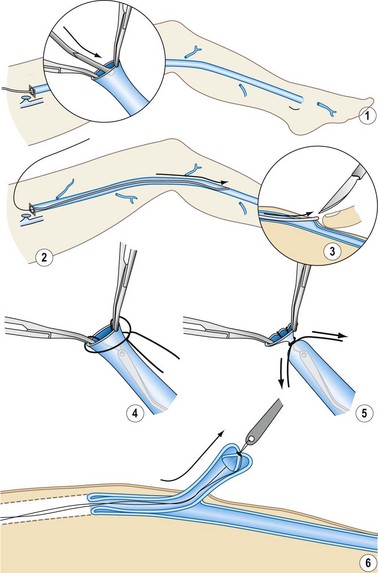
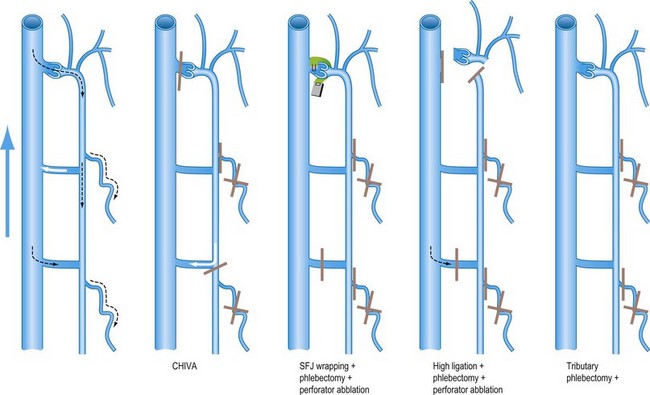
Surgery with saphenous trunk preservation
This is less invasive than other procedures, including vein stripping. The most aggressive part of vein stripping is the trunk excision. Besides, supporters claim that the preserved saphenous trunk might be used as an arterial substitute either for coronary surgery or as a bypass in femorocrural obliteration. Unfortunately there are no data on the real need for, or value of, the saphenous trunk as an arterial substitute after such surgery. Another argument in favor is the preservation of venous flow drainage, as ablation of the superficial system enhances varicose vein recurrence. The different procedures are depicted in Figure 10.6.
SFJ and/or SPJ ligation plus incompetent tributary phlebectomy with or without incompetent perforator interruption
Suppression of leak points between the DVS and the SVS combined with reservoir ablation is supposed to restore competence of the saphenous trunk.15–18 This procedure was promoted during the last two decades but is presently rarely performed, probably because the myth of compulsory HL has been discredited on account of its lack of clinical efficacy.
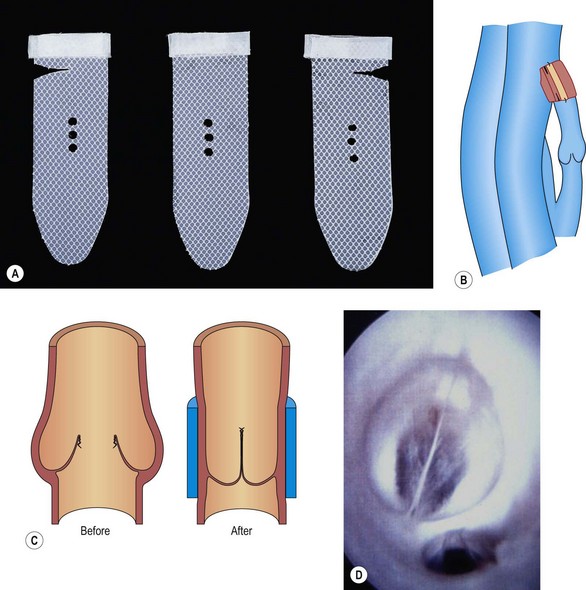
SFJ wrapping or valvuloplasty plus incompetent tributary phlebectomy with or without incompetent perforator interruption
SFJ Wrapping
The hemodynamic principle here is that by wrapping the SFJ using an external stenting technique (instead of the HL described above), the supposed restoration of competence to the valve restores valvular function (Fig. 10.7).19–21
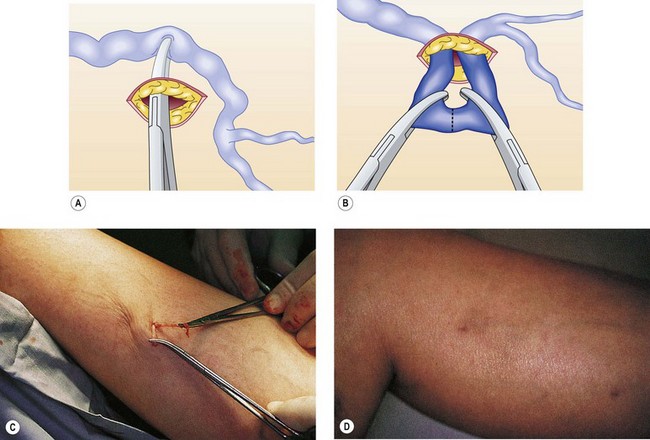
Ambulatory phlebectomy
Muller described this technique in 1956 and published it 10 years later.26 The method consists of extracting VVs in an outpatient setting under local anesthesia using small punctures and hooks, The procedure is described in detail elsewhere,27–29 but it is worth mentioning here that phlebectomy is performed by using fine-pointed blades, mini-incisions, and crochet hooks or other specialized phlebectomy hooks (Fig. 10.8).
Muller used this procedure in isolation or in combination with trunk stripping to avulse tributary varices, as reported in 1996.30
A powered phlebectomy device, the Trivex system (InaVein LLC, Lexington, Mass.), was introduced by G. Spitz in1966. Briefly, the system contains a shaver and a transilluminator coupled with an irrigator (Fig. 10.9).
Varices phlebectomy
Varices phlebectomy with conservation of the refluxing saphenous trunk is named in French ‘ablation sélective des varices sous anesthésie locale’ (ASVAL; selective ablation of varices under local anesthetic).31 This process gathers and unifies techniques of phlebectomy that were previously scattered and insufficiently systematized and is based on the demonstrated fact that varicose disease most often begins at lower leg level (see above). According to ASVAL principles, the suppression of varicose reservoirs (especially extra fascial varicose clusters) can – at least to a certain extent – improve or restore to normal (centripetal) the reflux in saphenous trunks, thus preserving them.32
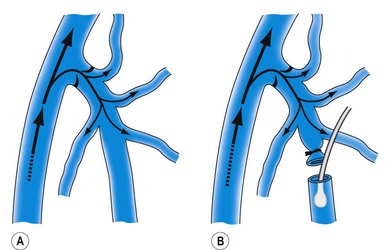
CHIVA method
CHIVA is the acronym of the French ‘Cure Conservatrice et Hémodynamique de l’Insuffisance Veineuse en Ambulatoire’.33 The pathophysiological basis of CHIVA relates to a ‘hemodynamicocentric model’ of venous insufficiency (VI).34
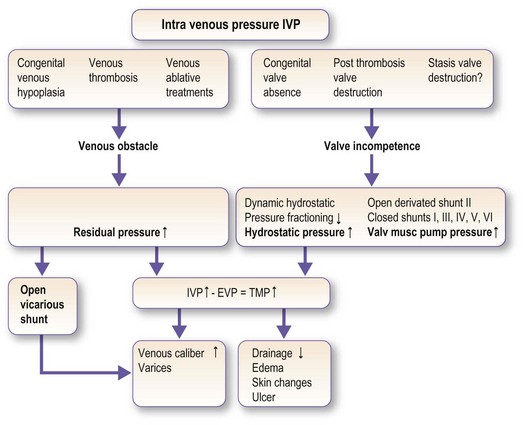
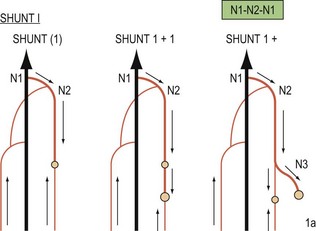
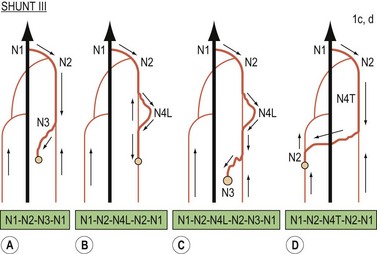
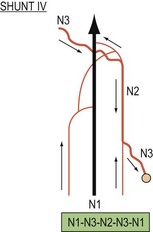
According to CHIVA all the VI symptoms are due to an obstacle to the flow and/or valvular incompetence which increases the transmural pressure (TMP). Excessive TMP dilates the veins (varices) and impairs drainage (edema, lipodermatosclerosis, and ulcer) (Fig. 10.10). The hemodynamic diagnosis consists of checking and, correcting the VI causes in order to normalize the TMP and, consequently, its clinical symptoms. According to the VI hemodynamic pattern, CHIVA involves fractioning the hydrostatic pressure, disconnecting the shunts, and preserving the draining veins in order to cure all the symptoms of VI at the same time and avoid recurrence. Open Deviated Shunts Type II (varices + segmental saphenous trunk reflux) and Closed Shunts Type III (varices + segmental saphenous trunk reflux + SFJ reflux (SFJR)) are frequent patterns of VI due to superficial valve incompetence. In these specific cases CHIVA divides the refluxing tributaries at their junction with the saphenous trunk. These divisions result in trunk reflux suppression and varices ‘remodeling’ to normal size while the drainage is preserved in order to avoid short-term side effects and long-term recurrences (in the case of Shunt III SFJR, redo due to a trunk re-entry) (Figs 10.11–10.14).
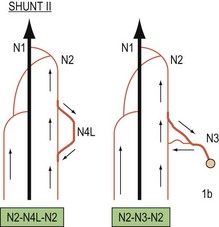
Figure 10.12 Types of ‘private circulation’ or veno-venous shunts according to CHIVA nomenclature.
(Courtesy of Dr Franceschi.)
Investigations to be Done Before VV Surgery
Systematic DUS prior to surgery for varicose veins is crucial. From a classification standpoint, DUS is used to complete CEAP sections E, A and P. In practical terms, it allows creation of a precise map that will be very useful during surgery (Fig. 10.15).
Patient’s Information
In addition, a written document is handed over to the patient (Appendix 10.1).
Anesthesia and Hospitalization
Anesthesia
Regardless of the technique used, surgery may be performed under local anesthesia (LA). Tumescent anesthesia is strongly recommended for all patients. This innovation has revolutionized surgery of varicose veins.35,36
The addition of epinephrine (adrenaline) does decrease ecchymosis, and Goldman has shown that in appropriate concentrations, epinephrine is safe when used in a tumescent anesthetic technique during ambulatory phlebectomy. It does reduce the incidence of hematoma and hyperpigmentation.37,38
Postoperative Care and Convalescence
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree