Fig. 14.1
Diagram showing possible causes for anterior cruciate ligament (ACL) failure. An overlapped area represents greater chance of failure
Many factors must be considered while formulating a treatment plan for the management of a failed ACL including the type and etiology of graft failure, patient symptoms and complaints, and timing and possible staging of procedures in the case of surgical revision.
Physical Examination
Specific tests for ACL laxity should be performed. It is noteworthy that in DB reconstruction, an isolated bundle graft failure can occur. Therefore, the Lachman test, anterior drawer test, and pivot shift test results should be jointly analyzed. A positive Lachman and anterior drawer with a negative or a slightly positive pivot shift may indicate an isolated AM bundle tear, while a positive pivot shift with a negative Lachman and anterior drawer test point to an isolated PL bundle tear.
The specific tests for ACL laxity described above address antero-posterior (AP) or rotational laxity, however they are subjective in nature. The KT-1000 (Medmetrics, San Diego, USA) provides an objective measurement in millimeters on the antero-posterior translation. On the other hand, portable and simple methods to reliably quantify the pivot shift phenomenon are still being developed.
Imaging
Radiographs
A complete radiographic series including Merchant view for patellar evaluation, weight-bearing antero-posterior (AP) view in 45° of flexion, lateral radiographs in 45° of knee flexion, and full extension AP radiographs are appropriate in the initial imaging analysis of a reinjured knee. These films allow evaluation of hardware position, degenerative changes, previous deformities, and associated fractures or avulsions. In addition, femoral and tibial tunnel widening, angle, and position can be assessed. Illingworth et al. showed that in AP radiographs a femoral tunnel angle less than 30° is non-anatomic and more than 30° is most probably located in the anatomic position [14] (Fig. 14.2).


Fig. 14.2
Femoral tunnel angles of an anatomic double bundle ACL reconstruction
In cases of valgus or varus extremity malalignment, a weight-bearing long-cassette radiograph is obtained for objective quantification of the lower limb axes.
Magnetic Resonance Imaging
MRI has been used as the gold standard exam to confirm ACL graft tear and identify concomitant intraarticular pathology. In addition to the regular MRI views (sagittal, coronal, and axial), special sequences such as oblique coronal and oblique sagittal, with sections at the same anatomic alignment of the ACL, should be obtained to allow a complete visualization of the ligament [15]. In addition to the diagnosis of graft rupture, MRI also allows for additional data on the previous surgery such as associated injuries, tunnel positioning, and graft orientation. Tibial insertion site size, ACL length, ACL inclination angle, and quadriceps and patellar tendon thickness on sagittal views are routinely obtained to assist in ACL revision technique and graft source decision. These measurements are even more meaningful if the primary injury MRI is available, allowing a direct comparison of the native insertion sizes, estimation of ACL length, and inclination angle (Fig. 14.3). This evaluation provides information on the initial restoration of native ACL anatomy, which is of fundamental importance for the preoperative planning of revision ACL reconstruction.
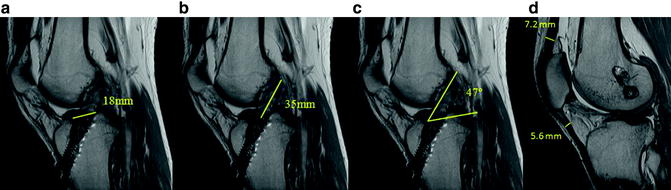
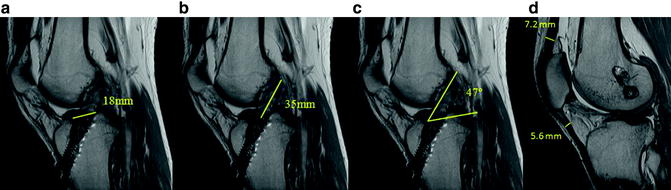
Fig. 14.3
Magnetic resonance imaging (MRI) preoperative measurements
3D-CT Scan
We routinely utilize a CT scan with three-dimensional reconstruction for evaluation of failed ACL reconstruction to identify previous tunnel placement and bony deficiencies irrespective of prior technique (Fig. 14.4). After a primary DB reconstruction, this exam is even more important as numerous tunnels are present and single-stage or two-stage revision procedures must be meticulously planned.
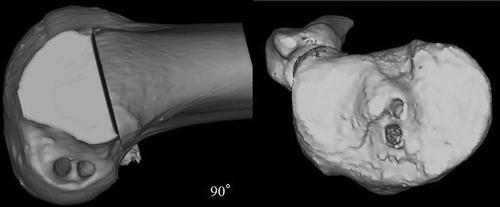
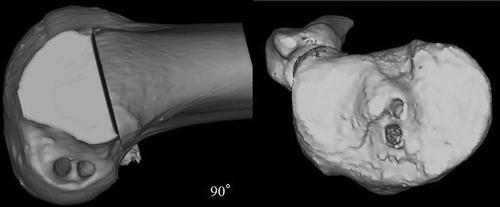
Fig. 14.4
Three-dimensional reconstructed CT scan of an anatomic double bundle ACL reconstruction
Indications and Contraindications
Overall, the indications and contraindications for a revision after double bundle ACL reconstruction follow the same principles as the primary surgery. Patients with recurrent instability after double bundle ACL reconstruction are better treated with revision reconstruction. Patients who participate in cutting, jumping, and pivoting sports are also appropriate candidates for surgical treatment.
On the other hand, asymptomatic, low demand, or elderly patients should have nonoperative treatment. Similarly, patients that have had multiple ACL reconstruction failures must be analyzed carefully before indicating another surgery. Individual anatomic, biomechanical, and behavioral factors that may have contributed to the previous failures must be addressed to increase the likelihood of a successful outcome.
Preoperative Planning
In order to develop an adequate preoperative plan for a revision ACL reconstruction, the primary cause of failure should be known. History, physical examination, and imaging should provide the necessary elements. The first decision to be made is if the revision surgery is going to be performed in only one or two stages.
A single-staged procedure is preferred when the previous tunnels are anatomically placed with no evidence of widening. In this case, tunnels may be reused and a DB revision is performed (Fig. 14.5). Another option for previous anatomically placed tunnels is converting the two tunnels’ entrances into one and performing SB revision ACL reconstruction by creating a single tunnel between the two. This is a particularly good option when one of the tunnels has evidence of widening with the other one remaining well preserved (Fig. 14.6).
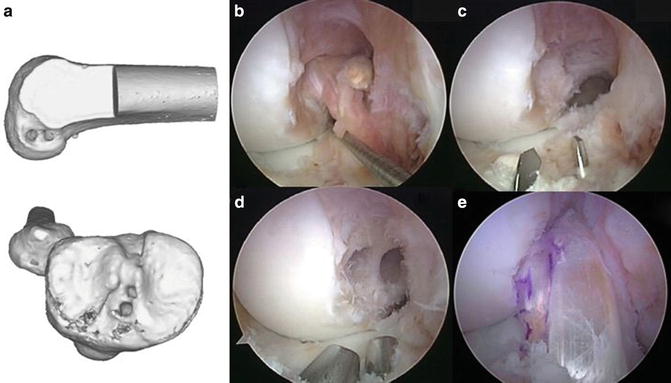
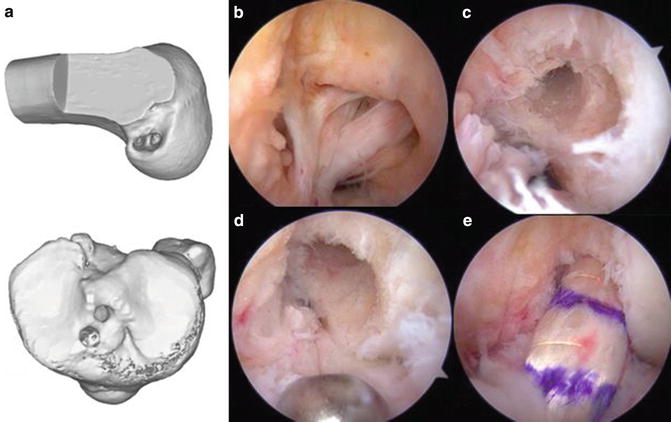
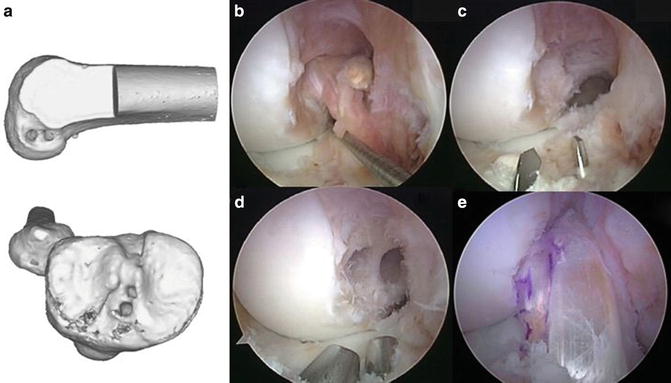
Fig. 14.5
Anatomic double bundle revision surgery after a primary anatomic ACL double bundle reconstruction. (a) 3D-CT scan showing double bundle anatomic placement. (b) Central portal visualization of the injured graft. (c) AM and PL tibial tunnel drilling. (d) All tunnels (two femoral and two tibial) prepared for graft passage. (e) Final aspect
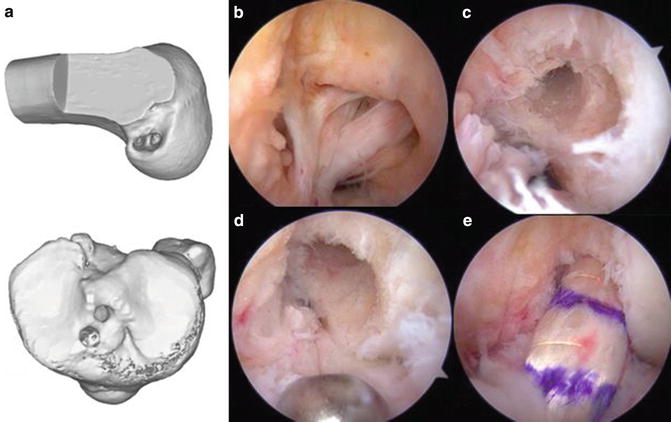
Fig. 14.6
Anatomic single bundle revision surgery after a primary anatomic ACL double bundle reconstruction. Both tunnels in each insertion site were converted into one. (a) 3D-CT scan showing double bundle anatomic placement. (b) Central portal visualization of the injured graft. (c) Femoral AM and PL tunnels separated. (d) AM and PL femoral tunnels converted into one tunnel. (e) Final aspect
For a previous non-anatomic primary DB reconstruction there are several alternatives to perform a single-staged surgical intervention.
1.
Non-anatomic placement of both the tibial and femoral tunnels: A complete non-anatomic DB is rare. However, in this scenario an anatomic SB revision procedure is our preferred technique. A DB reconstruction, even if possible, may increase the risk of condylar fracture due to the presence of multiple tunnels; although, a safe DB reconstruction can still be performed with the AM bundle placed in the over-the-top position (Fig. 14.7). In the tibial side, the PL and AM are usually anatomic or very close to the anatomic position and can be reused. If a SB procedure is planned, the closest tunnel to the tibial anatomic position should be prepared.
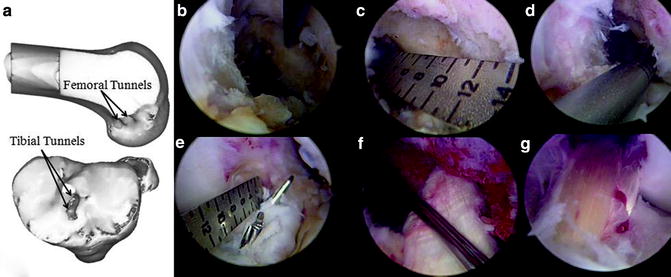
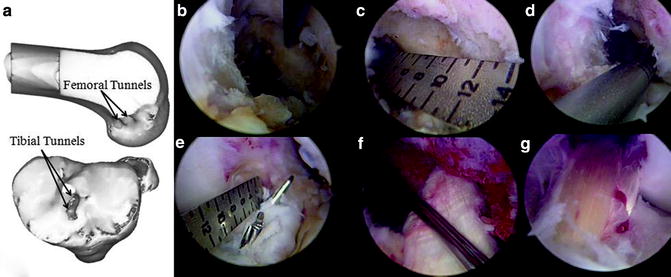
Fig. 14.7
Double bundle revision surgery after a non-anatomic primary double bundle ACL reconstruction. (a) 3D-CT scan showing femoral non-anatomic tunnels and anatomic tibial tunnels. (b) Old femoral tunnel probing. (c) Femoral insertion site measurement. (d) New PL femoral tunnel drilling. (e) Tibial tunnels drilling and measurement to confirm necessary space between them. (f) Femoral PL graft and “over-the-top” AM graft passage preparation. (g) Both AM and PL grafts final aspect
2.

If one tunnel is anatomically placed and the other is completely non-anatomic and:
Get Clinical Tree app for offline access
(a)
The anatomic tunnel is placed in the central portion of the insertion site: This tunnel may be prepared and reused for a SB revision reconstruction (Fig. 14.8). The tunnel edges may need to be freshened or dilated to allow for graft passage. This preserves condylar bone stock and simplifies the revision procedure.
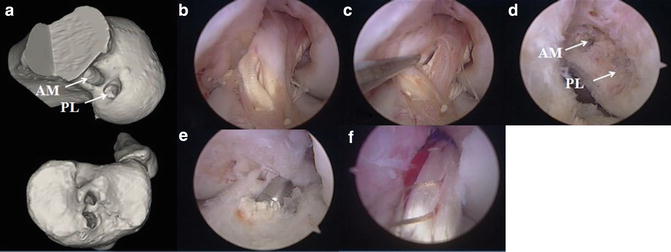
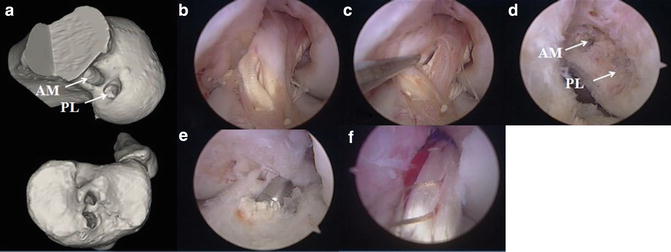
Fig. 14.8
ACL single bundle revision surgery after a non-anatomic primary double bundle ACL reconstruction. (a) 3D-CT scan showing PL tunnel within the ACL insertion site and a high AM tunnel in the femur. Tibial tunnels adequately positioned. (b, c) Central portal arthroscopic view of the stretched grafts. (d) Lateral intercondylar wall showing the aperture of both AM and PL tunnels. (e) Tibial tunnel dilation. (f) Final aspect
(b)
The anatomic tunnel is placed in either the PL or AM position (Fig. 14.9




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








