and Mauricio de Maio2
(1)
RZANY & HUND Privatpraxis für Dermatologie und Ästhetische Medizin, Kurfüstendamm, Berlin, Germany
(2)
Clínica Médica Dr Mauricio de Maio, São Paulo, São Paulo, Brazil
3.1.1 Introduction
3.1.2 Documentation
3.1.3 Charts
3.1.4 Photographs
3.1.5 Consent
3.1.6 Treatment Plan
3.1.7 Staff
3.2.1 Room
3.2.2 Chair
3.2.3 Mirror
3.2.4 Small Things
3.2.5 First Aid Kit
3.3.1 Introduction
3.3.4 Rule 3: Talk About Money
Abstract
Benign asbestos-related pleural diseases are the most common pathologic and clinical abnormalities related to asbestos exposure, with a greater prevalence than asbestosis. Solomon et al. [1] emphasized that the pleural manifestations of asbestos exposure include four specific benign pleural reactions: (1) benign asbestos effusion, (2) parietal pleural plaques, (3) diffuse pleural fibrosis, and (4) rounded atelectasis, or an area of collapsed, airless lung adjacent to an area of visceral pleural fibrosis. Notably, there is considerable overlap among these four disease processes (Fig. 6.1), with various combinations manifesting simultaneously or sequentially in a single individual. For example, a patient with benign asbestos effusion may subsequently be found to have diffuse pleural fibrosis, or a patient with parietal pleural plaques may develop rounded atelectasis.
3.1 General Requirements
3.1.1 Introduction
To ensure a safe and efficient procedure, several requirements must be met. The following list is not intended to give a complete overview, but to give some tips on preparations that might be helpful.
3.1.2 Documentation
A thorough documentation of all treatment-related data is highly recommended. This not only is advisable for legal and billing reasons but will help to improve your own performance and consequently the patient’s satisfaction.
3.1.3 Charts
The patient’s chart should include all necessary information. It does not matter if the chart is paper based or electronic. The only thing that counts is that the information in the chart is complete and accurate.
As with every chart, the patient’s identification data, gender, and age need to be documented first. In the next step, the reason for the patient’s visit should be documented. Furthermore, at this step, the history of relevant concomitant diseases (e.g., autoimmune diseases), present relevant drug intake (e.g., the intake of acetylsalicylic acid!), and previous aesthetic procedures should be documented. In particular, all previous injections of fillers should be thoroughly assessed.
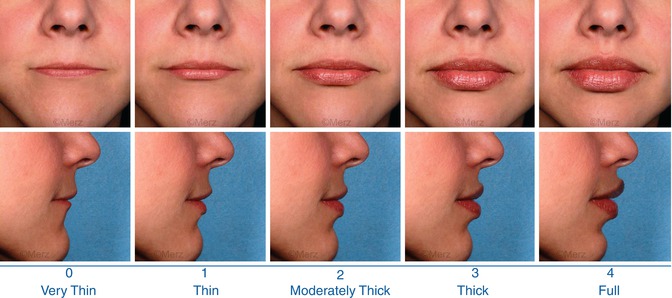
Patients must be thoroughly examined. Clinical severity can be assessed by using clinical wrinkles and volumes scales as the Merz Aesthetics Scales™ (Carruthers et al. 2008a, b, c, d, e (several publications) and 2012; Flynn et al. 2012) (Fig. 3.1).
Besides that, the treatment itself needs to be documented. The product used, the dilution (if any), the injected areas, the depth of injections, and the injected volumes should be logged. A graphical sketch might be helpful, too. Special attention should be given to the “lot” number of the filler used because this identifies the production batch and, in the event of adverse effects, might allow the manufacturer to trace an entire batch.
Last but not least, the chart should always include the informed consent of the patient. If you use electronic medical records, the consent should be scanned. For legal reasons, however, it might be necessary to keep the original in a specific binder.
3.1.4 Photographs
It is advisable to document the status of the patient before the treatment. If possible, the photographs should be standardized. Patients should be photographed frontal and at 90° and/or 45°. Standardization requires some effort, such as using a fixed setting or following standard procedures. In addition to being useful as legal documentation, these photographs will help to improve your communication with the patient (see Chaps. 2 and 4).
If you already have incorporated standardized photographs in your practice, you may also consider taking the full set of photos in selected cases. There are five traditional positions as described above (frontal view, right and left oblique, right and left full profile) in variable situations such as angry, surprised, kissing, full smile, chin down, and chin up depending on the type of treatment that is being carried out on the patient (Fig. 3.2).
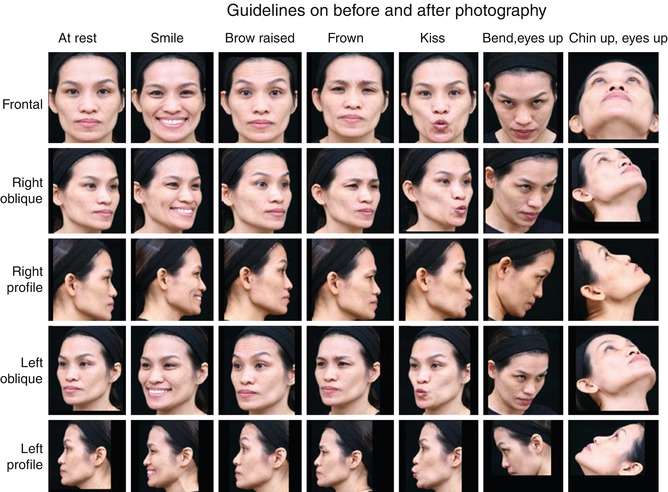
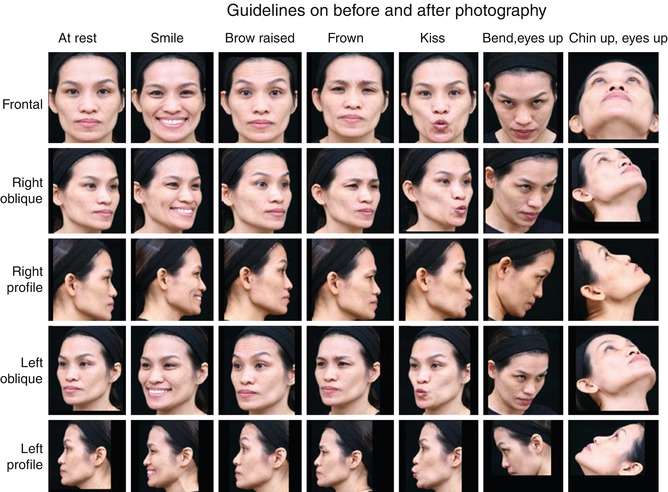
Fig. 3.2
Ideal baseline documentation of a patient’s full face (© de Maio and Allergan)
Do’s
Do take photographs! You need them anyway for the first consultation when the first steps of the treatment plan are laid out.
Don’ts
Do not worry if the photographic quality is not as good as you want it to be. This is not a photography contest but a tool for patient communication and documentation. A photo from your smartphone might be sufficient enough.
3.1.5 Consent
The consent of each patient should be thoroughly documented. Patients should date and sign a consent form for each new filler substance. A patient information brochure that includes all of the necessary information on the estimated efficacy and possible adverse events should accompany the consent form.
Don’ts
Do not forget to also get the photographic consent if you would like to use the photos for educational purposes.
3.1.6 Treatment Plan
3.1.7 Staff
Staff needs to be trained in marketing, quality control, and assistance. They should be aware of the aesthetic procedures offered and should be able to provide some information about the fillers used. They are responsible for monitoring the patient’s chart and for ensuring that all necessary documents are available and signed by the patient. And finally, the staff may help to apply topical anesthesia, massage the area after the injection of the filler, or add cooling before or after the injection to reduce pain and swelling. Staff might also assist with, makeup after the treatment, so that the patient leaves the clinic with no or little visible signs of the procedure performed.
3.2 Technical Requirements
3.2.1 Room
The procedure room should be brightly lit. Light from above might be helpful to detect even the tiniest areas to be corrected.
Do’s
Do provide good light for result evaluation. Make sure your patient leaves the office assured that expectations have been met.
Key Points
It is not uncommon that patients complain about results when they evaluate themselves at home under improper light conditions.