Rhinoplasty is the most challenging and difficult part of facial surgery because of its complex anatomical relationship between soft tissue, cartilage, and bony parts. These anatomical relations are more or less disturbed by the surgical procedures. Even when the relation between the different parts of the nasal skeleton is restored, healing is not completely predictable. Therefore, it is of great importance to use the least traumatic approach, to respect tip support mechanisms and the integrity of the cartilaginous framework, especially in the growing nose.
The percentage of revision surgery procedures depends largely on the experience and dedication of the surgeon, the extent of the surgical procedure, and, in the case of minimal sequelae, the demands of the patient. It can be as high as 25%. However, a high percentage of revision can be decreased with adequate preoperative management, appropriate (atraumatic) surgical techniques, critical assessment of the result of all surgical steps, and a long follow-up for self-education. Concerning the timing of revision surgery, one should wait at least 1 year in which the primary process of wound healing and scar formation has taken place before a revision rhinoplasty should be performed. Preferably, revision rhinoplasty should be done by an experienced rhinosurgeon.
Iatrogenic narrowing of the nasal vestibule, causing impaired nasal breathing, is a difficult problem that requires surgical treatment in most cases. A thorough analysis of the pathologic anatomical findings causing vestibular malformation and impaired nasal breathing is a prerequisite for successful surgical treatment.1 The pathology can be situated in the internal nasal valve area (caudal end of the upper lateral cartilage, septum, head of the inferior turbinate and piriform aperture), in the external valve area (skeletal and soft tissue structure of the ala, columella and soft tissue of the vestibular floor), or in both valves (internal and external valve). If the narrowing of the vestibule is caused by pathology of the anatomical structures surrounding the vestibule (caudal septal deviation, a collapsed upper lateral, protruding lateral crus and a too broad columella), surgical correction should not be too difficult.2–4 In more severe cases in which a collapsed ala is caused by overresection of the lateral crus and stenosing scar tissue or closure of a (unilateral or bilateral) cleft lip, a more complicated surgical procedure, often with the use of composite grafts, is indicated.
However, what appears to be a good result in the immediate postoperative period can diminish in the first postoperative months because of scar tissue retraction during the wound healing process. Therefore, complicated surgical treatment of vestibular stenosis demands a rational approach in which special prolonged postoperative care with the use of a vestibulum device (nostril splint) to prevent scar tissue formation appears to be of great benefit.5
 Patient Evaluation
Patient Evaluation
It is important to examine the nose during both quiet and forced nasal breathing to determine possible alar collapse and to inspect the nose without disturbing the anatomy by using a speculum. A speculum will distort the nasal valve angle. Palpation is a valuable tool when determining pathology or absence (partial or total) of the caudal cartilaginous septum and the alar cartilage, as well as to assess tip recoil.
When analyzing iatrogenic vestibular stenosis, it is important to assess the following:
- Whether the stenosis is caused by an aberrant anatomical structure, such as a caudal septal deviation, a protruding lateral crus, or a too-broad columella, which can be corrected by reallocation and resection of redundant tissue (Fig. 12–1).
- Whether the stenosis is caused by malformation or malposition of cartilaginous and soft tissue structures, which can be reshaped, reinforced, or repositioned (Fig. 12–2).
- Whether there is a shortage of tissue (skin or cartilage), which can be replaced by local flaps, free transplants of skin, cartilage, or composite grafts (Fig. 12–3).
Although many etiological factors that result in iatrogenic vestibular stenosis (e.g., surgical excision of vestibular skin tumors, electrocoagulation, chemical cauterization, prolonged nasal packing, pressure necrosis by nasal airway tube), it appears also as a more frequent sequelae of a reduction rhinoplasty with too-abundant reduction of the vestibular skin and cartilaginous nasal skeleton or as a result of cleft lip closure.
After thorough analysis of the pathology, a rational step-by-step operative procedure should be planned. Furthermore, standard preoperative and postoperative photographic documentation (frontal, lateral, oblique and basic view) is obligatory to evaluate the postoperative results. If possible, preoperative and postoperative rhinomanometry or acoustic rhinometry tests should be performed to evaluate the functional result.

Figure 12–1 Preoperative (A) and postoperative (B) basal view of a patient with stenosis of the nasal vestibulum caused by a caudal septal deviation.
 Composite Graft Harvesting
Composite Graft Harvesting
The auricle is a very appropriate donor site for composite grafts in nasal surgery. A careful operative procedure will leave only a minimal donor site morbidity of the auricle. Depending on the type and amount of tissue needed for the reconstruction of the nasal vestibule, a partial or complete conchal composite graft can be harvested.
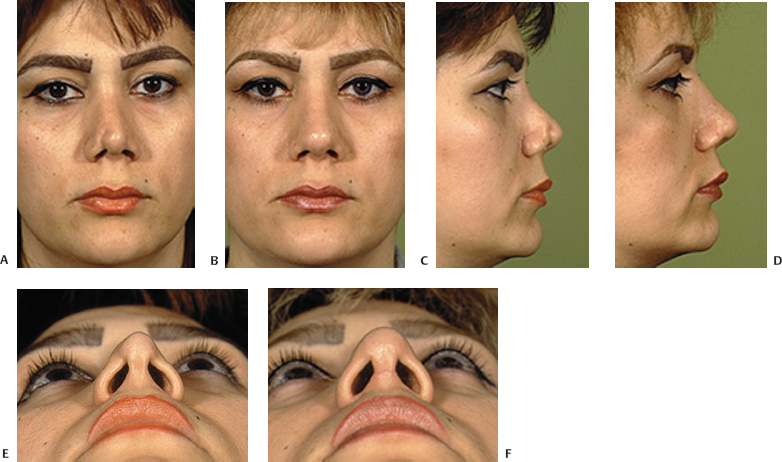
Figure 12–2 (A–F) Preoperative and postoperative views of a patient who underwent a revision rhinoplasty with the external approach to correct vestibular stenosis at the right side caused by overresection of the lateral crus and scar tissue retraction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


