Functional complaints are common among patients who have had a previous rhinoplasty, and they are an integral part of surgical planning during revision rhinoplasty. Not infrequently, patients present with both aesthetic and functional issues that may be conflicting; that is, the external nose is still too wide in certain areas, but there is new onset “congestion.” Regardless of the cosmetic outcome, most patients will be unsatisfied with persistent nasal obstruction and collapse. Maintaining a sound nasal framework during nasal surgery, therefore, remains of paramount importance. Moreover, having endured a previous surgical procedure, revision patients may bring with them a higher degree of skepticism and impatience. With this in mind, it is imperative that the plastic surgeon perform a detailed preoperative evaluation that includes not only the anatomic etiology of nasal obstruction but also the patient’s psychological expectations relating to yet another surgical procedure. Obstruction occurs from a variety of causes, including medical conditions of the nasal airway, and these should always be borne in mind by the surgeon (Table 6–1).1
Not all airway obstruction after primary rhinoplasty is correctable with spreader grafts. The precise anatomic etiology of nasal airway obstruction is a complex phenomenon that is often oversimplified. The “epicenter” of each patient’s collapse or airway narrowing may be located at a variety of points, which must be identified first, to apply the appropriate corrective maneuver. Matching the correct procedure from an array of options with each given patient remains a challenge rarely discussed.
| Cause | Examples |
| Allergic | Allergic rhinitis |
| Congenital | Nasal dermoid, glioma, encephalocele |
| Chronic rhinosinusitis | With and without nasal polyposis, asthma, aspirin triad |
| Endocrine | Pregnancy, hypothyroidism, adrenal insufficiency |
| Foreign body | |
| Iatrogenic | Atrophic rhinitis, overresection of lower lateral cartilage, excessive alar resection, saddle nose |
| Infection | Acute and chronic rhinosinusitis, septal abscess |
| Mechanical | Septal deviation, nasal valve collapse, synechiae, nasal polyps, inferior turbinate hypertrophy, concha bullosa, adenoid hypertrophy, choanal atresia, septal hematoma |
| Nasal cycle | |
| Neoplastic | Benign and malignant nasal tumors |
| Pharmacologic | Rhinitis medicamentosa |
 Anatomy
Anatomy
Many revision rhinoplasty patients have an iatrogenic source of their nasal obstruction. In a retrospective review of 53 consecutive cases involving adult patients who underwent nasal valve reconstruction over an 8-year period, Khosh et al2 found that 79% of their patients had previous rhinoplasties as the source of their obstruction. In these patients, obstruction was most often caused by collapse of the internal valve or narrowing of the external valve. The internal nasal valve refers to the cross-sectional area bordered by the junction of the caudal portion of the upper lateral cartilage and the nasal septum, circumscribing an angle of 9 to 15 degrees in the normal Caucasian nose.3 The anterior head of the inferior turbinate and the soft tissue at the piriform aperture also contribute to this “flow-limiting segment” of the nose. Aberrancies of any of the bordering anatomic structures (i.e., upper lateral cartilage, dorsal septal strut, cephalic portion of lateral crura, and inferior turbinate) can affect the normal physiology in this area. This internal nasal valve is the major flow-resistive segment of the normal nasal airway, which has an average cross-sectional area of 0.73 cm2.4 During normal inspiration, negative pressure is transmitted from the nasopharynx to the valve area, which consequently narrows in accordance with Bernoulli’s Principle. This principle describes how air flows quickly through the bottleneck of the nasal valve, creating a proportional fall in air pressure and an inward force on the nasal valve. The normal intranasal space should be of sufficient size and the side-walls of sufficient rigidity to maintain patency during inspiration. If the valve is inadequate, Poiseuille’s Law, which describes how airflow resistance is inversely proportional to the fourth power of the radius, comes into play. According to Poiseuille’s Law, a small decrease in the cross-sectional area of the nasal valve will produce a large increase in airway resistance and consequent nasal airway obstruction. In the nasal valve area, therefore, any narrowing will lead to increase airflow, then greater collapse (Bernoulli’s) and more narrowing, followed by even greater flow (Poiseuille’s) and collapse, until complete obstruction occurs.
Nasal obstruction also may result from narrowing of the external nasal valve. The external valve precisely refers to the area within the nasal vestibule, under the alar lobule, and is distinguished from the internal valve. The alar lobule is typically devoid of cartilaginous support and obtains its rigidity from the native fibrofatty tissue. To a minor degree, the central caudal border of the lateral crura contributes to this anatomic region. It is not often altered during rhinoplasty, with the exception of alar base surgery. The concave lateral crus, recently shown to be present in 40% to 50% of a cohort of Korean rhinoplasty patients,5 is an aberrancy that may directly impinge on the external valve and effect nasal airflow.
The most critical site for functional rhinoplasty, both primary and revision, is an area of the lateral nasal wall that rests between the internal and external valves, intervalve area. Structurally, it consists of the fibrofatty tissues spanning from the lateral aspect of the lateral crura down to the bony piriform aperture. It occasionally contains small sesamoid cartilages which lend it greater rigidity. Cutaneously, it corresponds to the supra-alar crease and occasionally is found to be deep and retracted. This intervalve area is extremely vulnerable to common rhinoplasty maneuvers, such as the complete strip or tip narrowing sutures, and often is the epicenter of collapse during inspiration.
 Etiology
Etiology
Iatrogenic causes of nasal obstruction may be found at many different levels of the nasal skeleton, including the internal valve, the external valve, or the supraalar crease area. Understanding the specific pathogenesis is vital both to prevent obstruction during primary rhinoplasty and to correct the problem during revision surgery.
The internal nasal valve is a common site of obstruction and can be traced to a variety of surgical interventions, including medialization of the upper lateral cartilages, excessively low lateral osteotomies, and loss of support to the dorsum (e.g., saddle nose deformity). Failure to reconstruct the middle nasal vault during hump reduction may be the single most common cause of internal valve problems. During dorsal hump reduction, particularly the cartilaginous dorsum, the upper lateral cartilages are usually disarticulated off the dorsal septum. At times, the intranasal mucosal attachments will be disrupted. In this case, the immediate postoperative exam may remain normal; however, over time, the nose undergoes continued contracture across the pyramidal nose, and the upper lateral cartilages begin to collapse medially and narrow the internal nasal valve. Examination of these patients reveals an inverted “V” deformity at the caudal border of the nasal bones or an “hour glass” deformity across the dorsum. This may take many years to develop and often appears unrelated to the primary surgery. As the cartilage falls intranasally, the narrowing of the middle vault creates a characteristic stigma of the prior reduction rhinoplasty. Prevention of this during the primary procedure involves preservation of the intranasal mucosa and a middle vault reconstruction with suspension of the upper lateral cartilages back to the dorsal septum, at times with prophylactic spreader grafts.
Tip ptosis can occur after any rhinoplasty maneuver that compromises stability and restoration of the critical tip support mechanisms, including most tip refining steps and the degloving of the nose. Its diagnosis is often self-evident, as patients will frequently volunteer the fact that simply lifting the tip of their nose just a few millimeters will provide immediate relief. This may be the long-term sequelae of a rhinoplasty as well as spontaneous tip ptosis seen in senescent patients. The drop in the nasal tip changes the relation between the laminar airflow and the internal valve and to a lesser extent the external and intervalve areas. Reprojecting the tip will often change the geometry sufficiently to rectify airflow.
A poorly placed osteotomy may lead to internal valve pathology. Although all lateral osteotomies result in a decrease in the distance between the septum and the lateral wall,6 a “low-to-low” osteotomy may lead to excessive medialization of the piriform aperture and the upper lateral cartilage, with narrowing of the nasal valve. This may be more prevalent in patients with preexisting narrow piriform apertures, hypertrophied inferior turbinates, or long nasal bones.
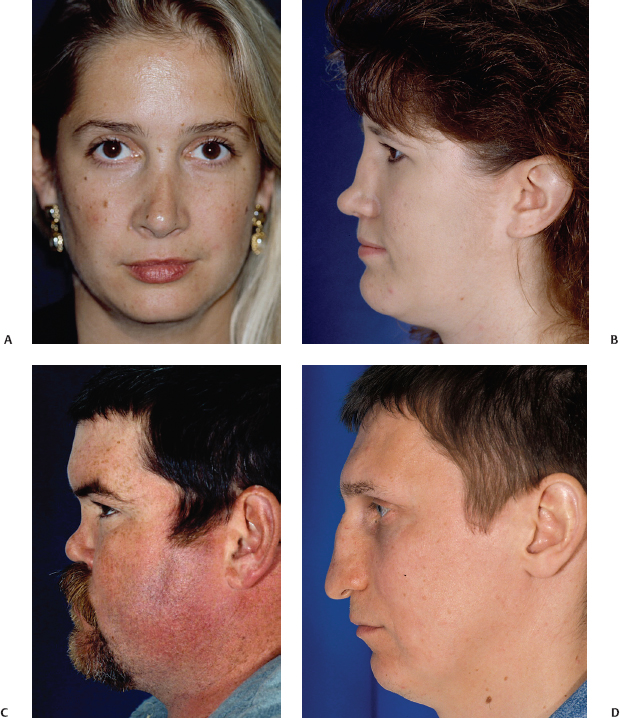
Saddle nose deformity refers to ventral collapse of the middle nasal vault while the tip and upper third remain relatively projected. The intranasal effect of this loss of support is obstruction at the internal nasal valve. The most common pathogenesis of this deformity is overresection of the dorsal septal strut or destabilization of the dorsal septal bony-cartilaginous junction (a.k.a., the “keystone” area). One also may find this problem as a consequence to granulomatous diseases, intranasal cocaine abuse, relapsing polychondritis, severe septal trauma, or untreated septal hematoma. Middle vault collapse will lead to nasal obstruction by direct narrowing of the internal valve at its medial (septum) and lateral (upper lateral cartilage) borders (Fig. 6–1).
Pathogenesis of external nasal valve obstruction includes excessive alar base resection, cicatricial stenosis from poorly placed marginal incisions, or concave lateral crus (as apposed to its normal convexity) (Fig. 6–2). Patients with a wide nasal base may present for a primary rhinoplasty in desire of alar base reduction, first described by Weir in 1892,7 and more recently modified by Sheen in 1987.8 Overresection of the alar base may, however, lead to excessive narrowing of the external valve and subsequent compromise of the nasal airway. A misplaced marginal incision, and certainly rim incisions, can heal unfavorably and lead to cicatricial stenosis. Overprojected noses with “tension” from the supratip area will have thin, slit-like, external valves that block airflow. Patients also may have narrowing of their external valve from the medial side, such as from a caudal septal deflection, splayed medial crura, or a prominent nasal spine (Fig. 6–3). Concave lateral crura can impinge on the external valve in a static manner and collapses readily during nasal inspiration in response to Bernoulli’s Principle.
The most common iatrogenic causes of collapse at the intervalve area include overresection of the lateral crura of the lower lateral cartilages (i.e., cephalic trim) and resultant scar contracture with alar retraction (Fig. 6–4). A cephalic trim is often performed during a rhinoplasty as a means to increase tip rotation and to reduce bulbosity in the supratip region. Care must be taken during this procedure to leave 7 to 9 mm of lateral crus remaining. Overresection will weaken vital support in the supra-alar area and lead to dynamic collapse with inspiration. In addition, when reducing the lateral crura, one should avoid manipulating the lateral most aspect of the lateral crura, that is, the border of the intervalve area. Disruption to this important lateral limb will not only affect tip support and rotation but also weaken the integrity of this area and predispose it to pinching of the supra-alar crease and narrowing of the airway.

Other causes for collapse at the intervalve area include patients in whom there has been a failure to recognize vertically oriented lower lateral crura (parenthesis deformity) during primary rhinoplasty. The parenthesis deformity is characterized by vertically oriented lateral crura with a slant of up to 60 degrees toward the lobule, instead of the normal 15 degrees, and a consequent lack of lateral wall support. Any resection or compromise of this little support will promptly lead to collapse and obstruction (Fig. 6–5). Recurvature of the lateral crura can be found as it curls back in toward the airway along its lateral aspect. Normal lateral crura have some curvature laterally, but it can be severe enough to enter into the vestibule or intervalve area and create airway obstruction. More importantly, the degree of recurvature may be subclinical, without associated nasal obstruction (Fig. 6–6). When this situation coexists with a broad tip that is scheduled to be refined, the narrowing procedure will often exacerbate the recurvature, pulling the lateral aspect of the lateral crura inward and creating new onset obstruction. This is especially true with dome-binding sutures (Fig. 6–7). The preoperative examination must assess for this anatomic aberrancy, with appropriate plans made to prophylax against further narrowing by reshaping the concave crura with lateral crural strut grafts. Paradoxically, concave lateral crura also are predisposed to nasal obstruction by virtue of their propensity to collapse with normal nasal inspiration. The normal lateral crus is found to be convex in multiple dimensions, thus optimally designed to resist a collapsing force and best maintain nasal patency. When they are deformed and concave, the geometry is such that it readily collapses. At times, the concavity can be dramatic and create a static obstruction at that level (Fig. 6–8).

Figure 6–3 This base view demonstrates narrowing of the external nasal valve as a result of a wide columella, prominent anterior nasal spine and wide medial crura.
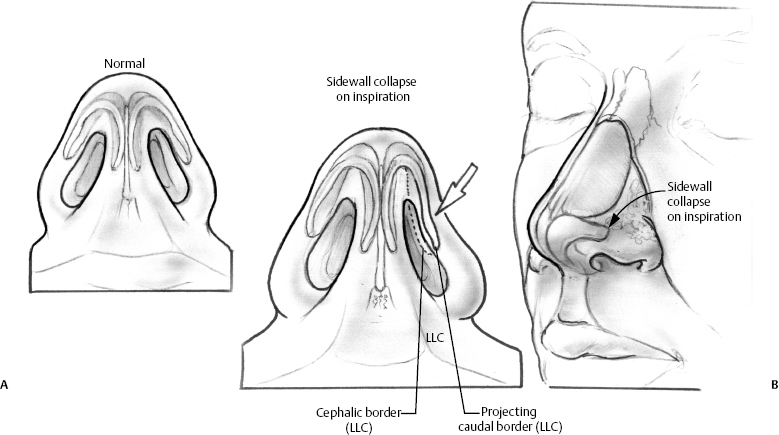
Figure 6–4 Illustrated here is collapse at the supra-alar crease intervalve area after excess resection of the lower lateral cartilage during a cephalic trim maneuver. If a sufficient amount of lateral crus is not left behind, dynamic collapse at this site will occur with inspiration. (A) Normal. (B) Sidewall collapse on inspiration.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



