Stage
GFR*
Description
Treatment stage
1
90+
Normal kidney function but urine findings or structural abnormalities or genetic trait point to kidney disease
Observation, control of blood pressure. More on management of stages 1 and 2 CKD
2
60–89
Mildly reduced kidney function and other findings (as for stage 1) point to kidney disease
Observation, control of blood pressure and risk factors. More on management of stages 1 and 2 CKD
3A
45–59
Moderately reduced kidney function
Observation, control of blood pressure and risk factors. More on management of stage 3 CKD
3B
30–44
4
15–29
Severely reduced kidney function
Planning for end-stage renal failure. More on management of stages 4 and 5 CKD
5
<15 or on dialysis
Very severe, or end-stage kidney failure (sometimes call established renal failure)
Treatment choices. More on management of stages 4 and 5 CKD
Xerosis: beginning with dehydration and reddening, prevalently in the areas of the extensor muscles of the limbs, progressively evolving into oedema and fissures. In the most advanced stages, there may be areas of lichenification and/or contact erythema. The fissured areas may allow bacteria to enter with consequent cutaneous infections. This form afflicts from 50 to 70 % of patients in dialysis.
Pigmentary disorders: these are directly correlated to the duration of the renal insufficiency. They range from hyperpigmentation to a yellowish colouring, prevalently in the areas exposed to the sun. Pallor is associated with frequent anaemia in such patients. This form afflicts from 20 to 70 % of patients in dialytic treatment.
Itching: frequent in such patients, it may be minimal but is found to be non-remittent and serious in 8 % of cases. It leads to a net deterioration in the quality of life.
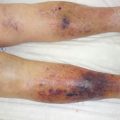
Another clinical situation of a dermatological type is NDF (nephrogenic dermal fibrosis). It was described in 2000 [2] and currently classified as systemic [3]. It is a pathology that is prevalently cutaneous and characterised by being associated with renal damage. Patients present oedemas and retractions prevalently in the lower limbs; the main symptoms are burning pain and itching. On a cutaneous level, there is the appearance of papules or plaques that are red or brown in colour and which, on rare occasions, may become ulcerous (Fig. 24.1). Around 5 % of these forms may exhibit aggressive and sudden worsening with the involvement of muscles, possibly leading to paralysis. As of now, the cause remains poorly defined: possible causes may include the use of gadolinium as a means of contrast [4], erythropoietin and the stages of hypercoagulability. Under X-ray inspection diffuse calcifications are noted on a subcutaneous level (Fig. 24.2).

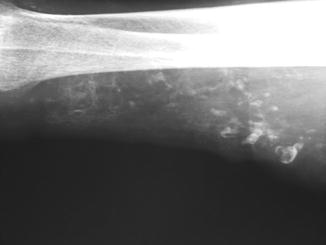

Fig. 24.1
NDF (nephrogenic dermal fibrosis)
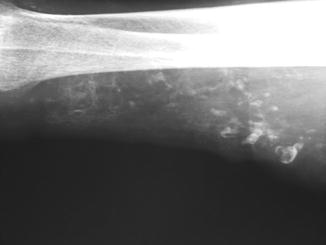
Fig. 24.2
Subcutaneous calcification in NDF
End-stage renal disease (ESRD) in itself behaves as a form of comorbidity in pre-existing situations causing complications that lead to the formation of necrotic tissues, as well as exacerbation in the appearance of cutaneous ulcerous lesions. Lastly, as a direct cause, it leads to complications that progress to ulcers.
24.1 Comorbidity
ESRD in itself leads to a state of fragility in the patient, with reduction of the immune system defences and consequently a greater incidence of infective phenomena. The reduction in renal clearing leads to an accumulation of catabolites that in themselves have an inflammatory action. A situation of increased phlogosis means healing times are lengthened, with a slowing down both of the retraction and the re-epithelialisation phenomena. Some examples: the frequent association with diabetes leads to a prognostic deterioration with an increase in the number of amputations and the evolution in a necrotic direction of the diabetic foot [5, 6]. Patients who have been in dialysis for long periods present a high rate of arterial disease which, with the phenomena of vascular calcinosis, may lead to the development of cutaneous necrotic ulcers of an arterial type [7]. Al Ghazal [8] also suggests a correlation with the development of forms such as pyoderma gangrenosum. Yates [9] has noted an increase in infections from MRSA in patients who have ulcers with ESRD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree