7 The procedures described in this chapter are all static in design and indicated to “touch-up,” “fine-tune,” or augment the results achieved with the techniques presented in Chapters 2 through 6. There are a variety of materials used for static suspension. Tantalium and Marlex mesh have been reported in the past, and more recently Gore-Tex has been used. These alloplasts become incorporated into the tissues after being anchored with sutures. However, all these materials have a tendency to form granulomas and have a high rate of extrusion. Lyophilized dried fascia is well integrated but tends to be structurally weak and fragments easily. The patient’s own tissues are ideal for static procedures. Fascia lata and palmaris longus tendon are recommended because they are readily harvested with limited morbidity. Further, their length and tensile strength are quite suitable to suspend or lateralize the nose and corner of the mouth. The major problems encountered around the nose and mouth include nasal obstruction, upper lip droop, corner of mouth droop, asymmetry of mouth at rest and with smile, and lower lip asymmetry. To achieve the desired effect, suspension and lateralization may be combined with commissureplasty, cheiloplasty, wedge resections, muscle plication, resection, or transposition. The experience with static procedures is reviewed in Chapter 1 (see Tables 1-2 through 1-5). Details of the digastric transposition procedure to correct lower lip deformity is described in Chapter 4 (see Figs. 4-20 and 4-21). The common problems involving the nose-mouth region that can be improved with static procedures are illustrated with the following case examples.
Regional Reanimation: Nose and Mouth
Mark May, M.D.
| Special Instruments and Equipment |
| Fascia stripper (N295-Storz) (to obtain fascia or palmaris muscle tendon) |
| Extra arm table (to place arm to take palmaris muscle tendon) |
| Large, right-angle Mixner clamp (to pull disect tunnel around zygomatic arch) |
| Deschamps ligature carrier, blunt point, left and right 15-2255, 15-2256 (Pilling Co.) (to pull fascia or palmaris tendon around zygomatic arch |
| Straight sharp ligature carrier (to pull palmaris tendon from lip, lip-cheek incisions to incision over zygomatic arch) |
| Tools used to place miniplate noted in Figure 7-2D |
| Drain-TLS closed suction drain (#6640 Portex Surgical, Inc.) |
| Sutures |
| 4-0 Nurolon (Ethicon Co.), C-5546, and RB-1 taper needle (for suturing muscle to lip) |
| 2-0 Nurolon (Ethicon Co), C-526T, and CT-2 tapered needle (to suture tendon to itself around zygomatic arch) |
| 5-0 clear Prolene (Ethicon Co.) 1739G (for subcuticular wound closure) |
| 6-0 mild chromic (Davis and Geck Co.) (326-13, CE-2) (to close skin) |
| Special Instrumentation |
| Reese scissors P6574 (Padgett KC MO) |
| Ligature carrier |
| Miniplate system (see Figure 7-2D) |
| Hall micro E drill system |
| Eyelid set |
| Bipolar Bovie console |
| Gore-Tex graft 1 mm (15293-10) |
| Clindamycin 600 mg dissolved in 30 cc normal saline to irrigate wound and soak Gore-Tex |
| Sutures |
| 4/0 Ethibond ×557 (to attach Gore-Tex to corner of mouth) |
| Drains |
| TLS closed suction drain (#6640 Porex Surgical Inc.) |
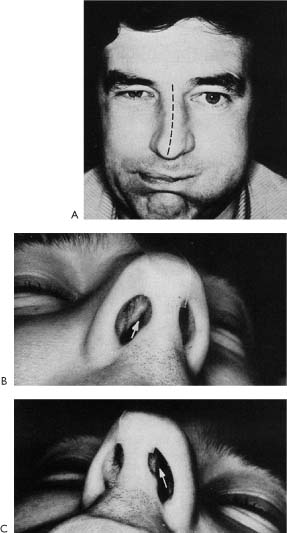
Figure 7-1. Nasal obstruction resulting from facial paralysis. A, Patient with faulty regeneration following right-sided facial paralysis. Note asymmetry when he attempts to blow out cheeks. Right eye closed, demonstrating synkinetic movement. Also note reversed C-shaped deformity of external nasal pyramid from nasal bones to tip. B, Patient complained of nasal obstruction from onset of facial paralysis that became more symptomatic by fourth month after onset because of faulty regeneration. Note collapse of angle between caudal edge of upper lateral cartilage and septum on the right. C, Normal relationship between caudal edge of upper lateral cartilage and nasal septum on the left. This patient was treated successfully with a nasosepto-rhinoplasty and did not need an alar lateralization procedure. (From May M et al.1 With permission.)
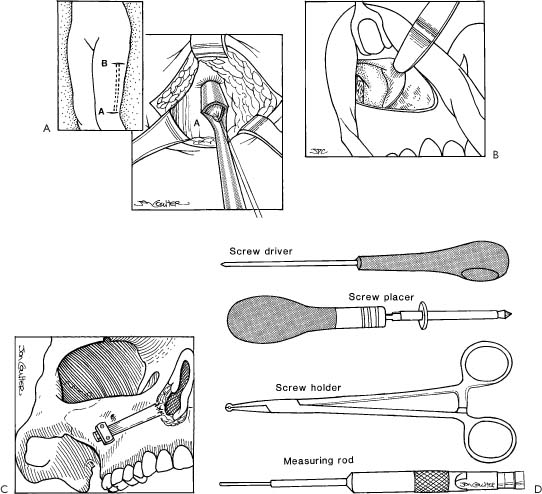
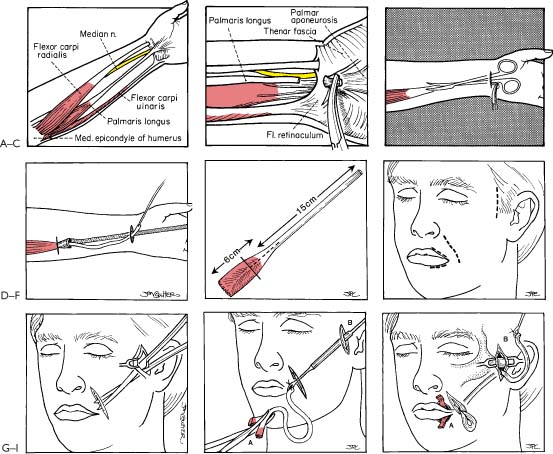
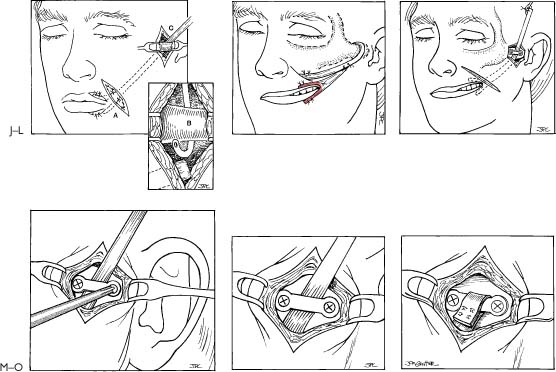
Figure 7-2. Nasal lateralization: fascia lata suspension and fixation with miniplate. Internal approach. A, Fascia lata taken from left thigh. An incision is made in the lateral thigh just above the knee (A). A tongue of fascia is pulled through a fascia stripper, and an appropriate length of graft material is taken. A counter incision is made at level (B) and the upper end of the fascia is divided. The fascia graft is then pulled inferiorly through incision (A). B, A buccolabial incision is made and periosteum is elevated exposing an area of the lateral ascending buttress of the maxilla. C, The fascia strip is fixed to the fibrocartilage base of the lateral nasal ala with 4-0 monofilament permanent sutures. The fascia strip is pulled laterally to create tension. Tension is maintained as the lateral aspect of the facial strip is fixed to the maxilla with a miniplate. A drain is placed in the surgical site prior to closing the wound. The wound is closed with a 4-0 chromic suture in a running locking fashion. (See Table 7-1 for instrumentation and suture materials.) D, Tools used to place miniplate.
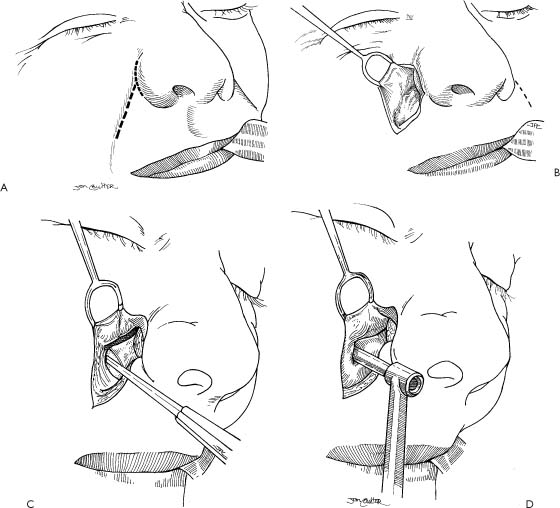
Figure 7-3. Nasal lateralization: fascia suspension and fixation with Mitek Mini Quick Anchor (Mitek Surgical Products, Inc., Norwood, MA). External approach. A, Incisions are made in the alar-facial and nasolabial crease. B, The deep aspect of the alar base is exposed. C, The periosteum is elevated exposing the lateral ascending buttress of the maxilla. D, A drill guide is placed perpendicular to the exposed area of maxilla in a position to produce the proper direction and tension for securing fascia from the alar base with a Mitek Mini Quick Anchor. E, A drill hole is made into the maxilla (ideally into the lateral ascending buttress and not through the face of the maxilla). F, A close-up of the end of the inserter with Mitek Mini Quick Anchor. Note the harpoon design. Once it is placed into a prepared hole in the bone, the metal “whiskers” keep it in place. G, Mitek inserter with mini quick anchor is used to push the anchor into the hole created in the maxilla. Braided polyester suture and two needles come already attached to the anchor. H, The fascia is first attached to the alar base with 4-0 monofilament permanent sutures. Then, under lateral tension, the fascia is fixed to the maxilla with the sutures attached to the anchor. The wound is then closed in layers after the insertion of a TLS drain. The suction drain is brought from the surgical site out of a separate puncture through the skin. (See Table 7-1 for instrumentation, suture materials, and type of drain used.)
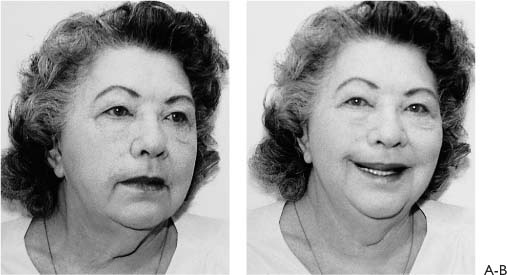
Figure 7-4. Nasal lateralization and upper lip suspension. Patient had a 2 × 2-cm epidermoid cancer resected that involved the skin in the right lip cheek crease region. Following this surgery, there was nasal collapse and upper lip droop on the operated right side. The rehabilitative procedure performed 2 years following the cancer resection is illustrated in Figure 7-3. Two months later, A, in repose. Note the barely noticeable healed scars are in natural skin creases. The nasal ala is in a normal position and nasal obstruction has been relieved. B, Smiling. The drooping of the upper right lip has been significantly improved.
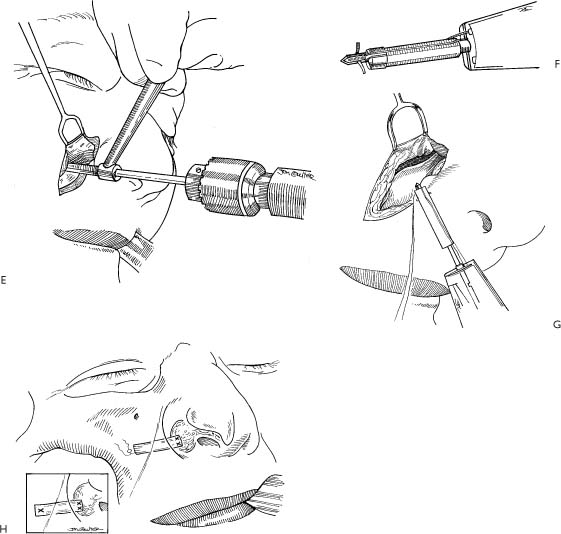
Figure 7-5. Palmaris longus muscle tendon reanimation technique (instruments used are listed in Table 7-1). A, The major landmarks and anatomical structures used for performing the palmaris longus muscle dissection are illustrated. B, Distal aspect of the palmaris longus tendon has been divided just as it inserts into the palmar aponeurosis. It should be noted the palmaris tendon is absent in 20% of patients. The presence of this tendon can be determined preoperatively by asking the patient to oppose the thumb to the little finger and flexing the wrist. The tendon can be found at surgery just deep to the skin and thin subcutaneous tissue through an incision that is made must behind the forearm palm crease. Structures at risk are the median nerve and the flexor carpi radialis tendon. The tendon of the palmaris longus muscle bisects the palmar crease; the flexor carpi radialis is deeper, thicker, and in a more lateral position when the forearm is rotated to place the thumb in the lateral position. C, The proximal end of the palmaris longus tendon is grasped with a clamp, and the soft tissue around the tendon is separated with a long scissors to about the lower third of the forearm. D
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree