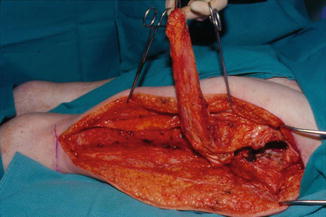
Fig. 11.1
Operative photograph of a patient in the semi-lateral position showing the marking for the Girdlestone procedure and vastus lateralis or rectus femoris muscle for utilization to close the hip defect
The main technical obstacle in the Girdlestone procedure was how to close the defect resulting from removal of the head, neck, and trochanter of the femur. The problem was finding soft tissue to close the defect. Girdlestone and the other authors described various different local tissues to close the defect, for example, the gluteus maximus muscle and deepithelization of the skin and insertion into the defect. Unfortunately, all these procedures were unsuccessful and eventually left a defect or discharging sinus. In 1983, however, Arnold and Witzke [8] described the use of the vastus lateralis muscle flap to repair a failed total hip arthroplasty. This technique had been described previously by Minami et al. [9] to close a trochanteric ulcer. The main postoperative complication for the surgeon was how to immobilize the pelvis and the lower extremity to prevent hematoma resulting from mobility of the proximal femur against the inserted muscle into the defect. Klein et al. [10], in 1988, presented a group of patients who had a Girdlestone procedure and vastus lateralis muscle flap by stabilizing the pelvis and the proximal femur using an external fixture. They claimed this method stopped the pistoning effect of the femoral shaft against the muscle. The wounds healed, but, unfortunately, there were complications from using the external fixture, such as pin track infection with loosening of the pin. In addition, an orthopedic surgeon was needed to place and remove the external fixture, and it was difficult to place the patient in a specialized bed postoperatively with the external fixture.
The author [11], in 1991, presented a larger series of patients with a Girdlestone procedure and vastus lateralis muscle flap with modified operative procedures and postoperative management. The Girdlestone procedure was performed in a radical way by excising the head of the femur and greater trochanter to a level below the lesser trochanter to eliminate the entire infected bone and to detach the insertion of the iliopsoas muscle, which eliminated the source of severe spasticity or contracture of the muscle. This step of the procedure enabled straightening of the lower extremity of the patient. The author, at that time, performed this procedure in three stages – debridement, bone excision, and then insetting the muscle in the defect. The final stage was placement of the skin graft over the muscle surface. The main modification by the author was replacing the external fixture with a foam abduction pillow placed between the lower extremities of the patient to maintain stability of the surgical site until healing was achieved 4 weeks postoperatively. To prevent any residual postoperative muscle spasms, antispasmodic medication was given. This approach achieved good healing of the hip wound. Years later, the author modified the entire procedure, as a result of extensive exposure and experience in at least 1,000 Girdlestone procedures for different etiologies, by performing the procedure in one stage, that is, debridement and bone excision, insetting the muscle, and closure by local fasciocutaneous flap or direct wound closure. This modification resulted in excellent healing and decreased the number of trips to the operating room to one, in the end shortening hospitalization time. This practice became the standard protocol at our center and part of the teaching curriculum to plastic surgery residents in training.
11.4.2 Side Effects of the Girdlestone Procedure
This procedure is lifesaving as it eradicates the infection with debridement of the involved bone. Pathological specimens are obtained for histology and bacteriology of the pelvic bone to determine the type and extent of infection and the duration of antibiotic treatment that is indicated. Unfortunately, there are a few side effects from the procedure, listed below, that the surgeon and the patient should be aware of, especially if the patient has a spinal cord injury and understands the importance of the hip joint for their function as a wheelchair sitter:
The lower extremity becomes loose and the leg can be rotated up to 360°
Shortening of the leg, which may not be important or functional in wheelchair sitters
Loss of stability during sitting and transferring. Normally the hip joint provides the patient with stability during transfer
Pelvic obliquity may result, and eventually this predisposes to development of pressure ulcer over the contralateral ischium
Heterotopic ossification can develop between the end of the proximal femur and the pelvis, which limits the range of motion in the hip area
Educating the patient on the outcome protects the surgeon from medico-legal liability post-surgery. The Girdlestone procedure is an important procedure in the life of the patient with spinal cord injury, which was advanced with the utilization of the muscle flap, and it is one of the important reconstructive surgery procedures around the pelvis. The author strongly believes that plastic surgery trainees should be exposed and trained to perform this procedure. The plastic surgeon should be the team leader in the management of these difficult reconstructive surgery cases.
11.4.3 Operative Technique of Girdlestone Procedure
Patient Position
If the Girdlestone procedure is performed for femoral fracture, dislocation, or heterotopic ossification, the appropriate position is the supine position with a pelvic tilt toward the contralateral side or the complete lateral position using a bean bag for patient support. The prone position is used when the hip joint is affected with the existence of a pressure ulcer.
11.4.4 Topographical Marking of the Operative Site
The most important markings for the surgical approach to the vastus lateralis muscle are the anatomical markers of the greater trochanter and the hip joint. A vertical line extends a few centimeters above the lateral condyle of the femur in the mid-lateral thigh, which is midway between the anterior and posterior territory of the tensor fascia lata fascia. Proximally, the line divergies into a T-shape where the lateral line of the T is over the lower part of the gluteus maximus muscle. This approach is important when dealing with a dislocated hip or femoral fracture. The medial part of the T-line extends anteriorly. This extension is important when excising heterotopic ossification of the hip, which usually extends anteriorly (Fig. 11.2). When there is an existing trochanteric ulcer, the design of the incision should involve ulcer excision and repair by a tensor fascia lata flap. The vascular pedicle of the vastus lateralis muscle should be marked to avoid the risk of damaging the pedicle during the dissection, which is 10 cm below the anterior superior iliac spine.
Fig. 11.2
Operative photograph showing the exposure of the vastus lateralis muscle and the greater trochanter. Arrow indicates hip joint location
11.4.5 Operative Technique
The author prefers to begin incising the skin distally because the iliotibial tract is superficial at that site. After incising the skin and the subcutaneous layer, the deep fascia, which is the iliotibial tract, is identified. When the fascia of the vastus lateralis muscle is observed, a scalpel is used to incise the fascia. The incision extends proximally, exposing the vastus lateralis muscle to the level of its origin from the greater trochanter. Above that point, the gluteus maximus and the tensor fascia lata muscles are observed. Using an electrocautery, separation between the two muscles is performed. By completing this dissection, two flaps are raised. A self-retaining retractor can be placed superiorly and inferiorly. The hip joint is exposed (Fig. 11.2). Depending on the pathology of the hip joint, the superior incision can extend anteriorly toward the groin or posteriorly through the gluteus maximus muscle. To expose the proximal femur, a transverse incision is made over the origin of the vastus lateralis muscle using an electrocautery about 2 cm below the greater trochanter. The vastus lateralis muscle fibers are dissected from the proximal femur using a periosteal elevator. The lateral attachment of the vastus lateralis muscle from the lateral inter muscular septum is dissected and transected by an electrocautery for about 5 cm inferiorly or to a level below the lesser trochanter of the femur. A noncrushing tissue clamp is placed over the free edge of the vastus lateralis muscle to expose the proximal femoral shaft (Fig. 11.3). Two protector instruments, called a cobb elevator or Chandler, are placed under the shaft of the femur to protect the soft tissue from injury during the bone cutting (Fig. 11.4). A transverse osteotomy below the level of the lesser trochanter is made over the femoral shaft using a bone oscillating saw. Complete division of the bone can be performed using a bone osteotome. A bone ring forceps is placed over the proximal femoral component and is lifted up using electrocautery dissection, or transection of the soft tissue attachment is completed (Fig. 11.5). The tissue holding the femoral head in place is the capsule, which is a strong tissue. Multiple longitudinal incisions are made and then a transverse incision is made to transect the entire capsule from the acetabular attachment and the attachment at the neck of the femur. At this stage, the head of the femur is still in the acetabulum. Using the cobb elevator, which can be slipped between the head and the acetabulum with a retraction maneuver, the head can be dislocated from the acetabular cavity. The ligamentum teres (ligament head of the femur) keeps the head attached to the acetabular cavity and can be transected, which completes the Girdlestone procedure (Fig. 11.6).
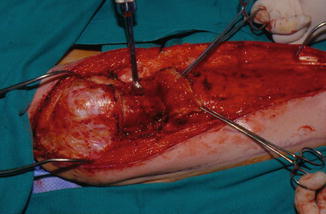
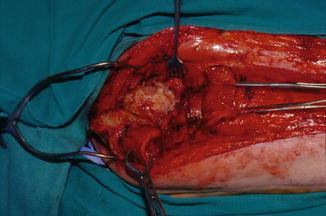

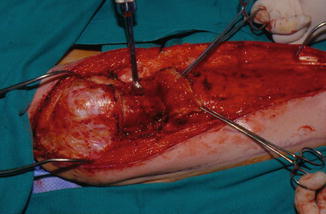
Fig. 11.3
Operative photograph showing the reflection of the vastus lateralis muscle from its origin to expose the proximal femur when a cobb elevator instrument is inserted underneath the femur to prepare for the femur transection by oscillating saw
Fig. 11.4
Operative photograph showing the osteotomy of the proximal femur has been performed. The proximal component of the hip is lifted by a bone forceps for dissection. Arrow indicates the location of the proximal femur post osteotomy
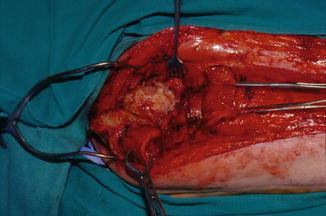
Fig. 11.5
Operative photograph showing the soft tissue attachment and the capsule of the joint dissected and the head of the femur is nearly dislocated from the acetabular cavity

Fig. 11.6
Operative photograph showing the actual specimen of the head of the femur, greater trochanter, and lesser trochanter removed by Girdlestone procedure
The end of the proximal femur can be smoothed using a flat bone file (Fig. 11.7). If the medullary cavity continues to bleed, pieces of collagen hemostat (Avitine®, Bard) are packed in the medullary canal to stop bleeding. The author prefers not to use bone wax because it may act as a foreign body. The acetabular cavity treatment depends on the original pathology of the hip joint. If the the hip joint was infected, curetting the cavity is performed and then a deep bone biopsy is taken for histopathology and bacteriological examination for culture and sensitivity. The acetabular cavity should be irrigated well with normal saline and bacitracin solution. The resulting large cavity from removal of the femoral component or bone destruction must be filled with muscle to fill the dead space and maintain healing (Fig. 11.9).
Fig. 11.7
Operative photograph showing the proximal femur and the cavity resulting from removing the femoral component. Short arrow indicates the proximal femur after osteotomy, long arrow indicates the location of the acetabulum
The main difference between the approach used in the 1940s and the one today is the repair of the defect resulting from the Girdlestone procedure by muscle flap. The next step is for the plastic surgeon to determine which muscle to use to repair the defect. This depends on the patient’s primary disease, whether they are nonambulatory or ambulatory, the size of the defect, and the age of the patient. The main muscles available locally for repair of the defect are the vastus lateralis muscle, the rectus femoris muscle, and the rectus abdominis muscle. Figures 11.1, 11.2, 11.3, 11.4, 11.5, 11.6, 11.7, 11.8, 11.9, and 11.10 show the operative technique for the Girdlestone procedure.
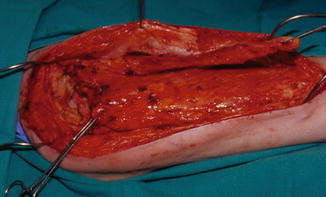
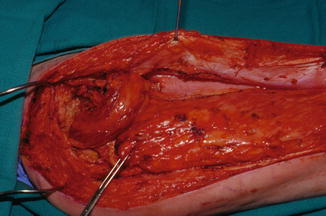

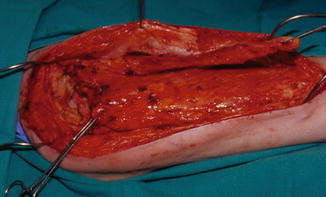
Fig. 11.8
Operative photograph showing the dissection of the rectus femoris muscle for use to close the defect
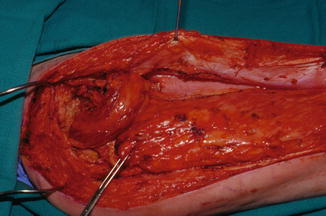
Fig. 11.9
Operative photograph showing the method by which the rectus femoris muscle is insetted to cover the hip defect. The proximal part of the vastus lateralis muscle will be advanced to cover the free proximal femur

Fig. 11.10
Operative photograph showing the complete closure of the wound
11.5 Vastus Lateralis Muscle Flap
11.5.1 Surgical Anatomy of the Vastus Lateralis Muscle
The vastus lateralis muscle is a powerful muscle in function and volume with a reliable blood supply. It is one of the important muscles in the formation of the quadriceps mechanism, which is responsible for extension of the leg at the knee joint. When utilizing the vastus lateralis muscle in ambulatory patients, this should be taken into consideration. The author usually repairs the resulting defect between the rectus femoris and the vastus medialis. The vastus lateralis muscle originates from the lateral surface of the greater trochanter and the trochanteric line of the femur, and posteriorly from the lateral intermuscular septum and the lip of the linea aspera of the femur. It is inserted with the other tendons of the rectus femoris and the vastus medialis to form the common quadriceps tendon, which is inserted into the patella. The vastus lateralis muscle has a relationship to the other muscle of the lateral thigh muscle group. It is situated between the rectus femoris muscle and the biceps femoris muscle. The vastus lateralis covers the vastus intermedius, which is a thin sheath of muscle covering the entire femoral shaft. When raising the vastus lateralis it is difficult to separate the plane between the vastus lateralis and the vastus intermedius muscle, as it is not well defined. For this reason, the vastus intermedius muscle is always raised as a part of the vastus lateralis muscle.
The vastus lateralis muscle is supplied with the main pedicle from the lateral circumference artery, which is a branch from the profunda artery. The vascular pedicle is the descending artery at a level about 10 cm below the anterior superior iliac spine. The lower portion of the muscle is supplied by branches from the femoral artery, which are branches from the lateral geniculate artery. The author’s clinical observation is that, when utilizing the entire muscle, the main pedicle can support the entire muscle bulk. For this reason it is rare to encounter ischemia or necrosis of the distal part of the muscle. The motor nerve of the vastus is a branch from the femoral nerve. The vastus lateralis muscle, with its excellent blood supply and volume, is used to reconstruct the hip and pelvic region. In addition, it can be used to repair the sacral area when the gluteus maximus muscles are not available. When there is extensive ischial perineal ulceration, it can be used to reconstruct the entire perineal area, even to the contralateral side.
The vastus lateralis can be raised as an island flap and rotated in a large arc of rotation. It can be covered with a skin graft with scoring of the muscle fascia to increase the size of the surface. A skin graft is acceptable functionally, otherwise, the muscle can be covered with a fasciocutaneous flap, such as the tensor fascia lata as a rotation flap, or a posterior thigh flap. The donor site of the vastus lateralis muscle flap can be closed primarily without any major complications. In the author’s experience, in closing a hip defect it is not a standard to utilize the vastus lateralis muscle, especially in a patient with spinal cord injury, because this group of patients has a high rate of ulcer recurrence and they need a reserve of muscles. Therefore, the vastus lateralis muscle is an excellent muscle to close different anatomical locations and, for this reason and considering the size of the defect, the rectus femoris muscle is recommended as a substitute.
11.5.2 Operative Technique for Elevation of the Vastus Lateralis Muscle
The position of the patient on the operating table depends on the pathology of the hip joint or the existence of a pressure ulcer as described in the section on the Girdlestone procedure. When a pressure ulcer and other hip pathology exists, the prone position is used. If the vastus lateralis muscle is to be used for a hip joint defect resulting from heterotopic ossification or a traumatic condition such as fracture or dislocation, the supine or lateral position is used.
The standard skin incision is in the mid-lateral thigh extending from above the knee and passing the greater trochanter. Depending on the pathology of the hip, it can be extended medially or posteriorly. If the tensor fascia lata flap is needed for a trochanteric ulcer, the design can accommodate the flap. The skin is incised deep to the iliotibial tract, exposing the vastus lateralis muscle. Blunt dissection is performed to raise two flaps for complete exposure of the vastus lateralis muscle. There are many perforators originating from the muscle to supply the deep fascia that need to be coagulated. The pathology of the hip or the ulcer is then dealt with (see under Girdlestone procedure and heterotopic ossification or trochanteric ulcer). Two self-retaining retractors are placed on the upper and lower parts of the wound. The author prefers to first identify the plane between the vastus lateralis and the rectus femoris superiorly with blunt dissection; the two muscles can be easily separated. Inferiorly, the plane becomes tendinous and an electrocautery is used for dissection. Dissection is stopped above the suprapatellar bursa. Care should be taken not to open it. Dissection then continues to separate the vastus lateralis muscle from the trochanteric and femoral attachment. A transverse incision is made over the origin of the muscle from the greater trochanter. Care should be taken not to extend too medially to avoid injury to the vascular pedicle. The muscle is lifted from the proximal femur, leaving behind the periosteum intact. Dissection continues laterally to detach the muscle from the lateral intermuscular septum. There are many large perforators that sometimes are difficult to coagulate and they retract behind the septum. Small amounts of muscle fiber can be left behind to help coagulate these perforators. The muscle is detached inferiorly and transected horizontally at a level above the condyle of the femur and the formation of the quadriceps tendon. Care should be taken to avoid opening of the suprapatellar bursa. If it is opened accidentally, it should be closed. When the muscle is completely free laterally, it can be easily dissected from the entire femoral shaft, leaving the periosteum intact.
As described previously, the vastus intermedius is a thin muscle and the author’s practice is to leave the muscle intact with the vastus lateralis as one component. The dissection of the vastus lateralis medially is to locate the interdigitation between the vastus lateralis muscle and the vastus medialis, which is difficult to find as a real plane, although there is a demarcation of tendinous part. Using an electrocautery in a perpendicular fashion on the femoral shaft, dissection between the two muscles is performed starting inferiorly and proceeding superiorly. The dissection is stopped when approaching the level of the muscle pedicle, which enters the muscle surface medially. After obtaining a sufficient length of the vastus lateralis muscle to cover the defect or to be rotated to cover ulcers, the dissection is stopped. When the muscle is needed to cover a hip or pelvic defect, the muscle is rolled on itself without tension and inset into the defect, including the acetabulum. As a standard, two drains are used, one under the muscle in the acetabular cavity and the other over the muscle. The exits of these drains are above the knee. At the same time, they will drain the vastus lateralis donor site. A third drain can be used to drain the superior part of the field, especially if the gluteus maximus muscle was incised during the surgery. The vastus lateralis muscle is sutured to the surrounding soft tissue, which is the gluteus maximus muscle, and the thigh wound is closed in three layers (deep, dermal, and skin). See Chaps. 8 and 11 (Figs. 11.11, 11.12, 11.13, 11.14, 11.15, 11.16, 11.17, 11.18, 11.19, and 11.20).



Fig. 11.11
Plain x-ray of the pelvis of a patient with spinal cord injury showing a previous right femoral fracture and left dislocated hip

Fig. 11.12
Operative photograph showing the patient in the supine position with skin marking for the surgical procedure of a Girdlestone and muscle flap. Arrow indicates the anterior territory of the tensor fascia lata (TFL) fascia
Fig. 11.13
Operative photograph, lateral view, showing the marking for the exposure of the vastus lateralis. Arrow indicates the topographical marking of the vascular pedicle
Fig. 11.14
Operative photograph showing the exposure after the Girdlestone procedure and dissection of the vastus lateralis distally from the rectus femoris muscle. Arrow indicates the vastus lateralis muscle
Fig. 11.15
Operative photograph showing complete dissection of the vastus lateralis muscle from the entire femoral shaft and other attachments