Fig. 10.1
(a) Operative photograph showing the patient in semi-supine position with a trochanteric ulcer marking of the important landmarks, interior superior iliac spine, the vascular pedicle to the muscle, and the anterior territory of the TFL fascia, arrow pointing to the line. The type of flap used in this case is TFL in a V-Y fashion. (b) Operative photograph showing the patient in semi-supine position with marking of the posterior trochanteric ulcer (Q-tip) and the marking of the posterior territory of the TFL fascia. Arrow indicates the lateral intermuscular septum. The type of flap used in this case is the V-Y advancement flap. (c) Operative photograph showing the marking for trochanteric ulcer and the V-Y TFL flap, in addition to other markings of the interior territory of the TFL fascia. Arrow indicates the interior territory of the TFL fascia
When the patient is turned into the lateral position which is the ideal position for this type of surgery, the patient is maintained in the lateral position by using a bean bag. The ulcer is marked in a triangular shape with the apex directed anteriorly. A line is drawn from the inferior lateral angle of the ulcer and extended inferiorly to a level about 10 cm above the knee. From this point, the other triangle limb is extended superiorly and stopped below the marking of the vascular pedicle. If the patient has more ulcers to operate upon at the same time with the trochanteric ulcer, then the patient is placed in the prone position.
10.2.3 Operative Technique
The lateral position of the patient is used when operating on a solitary trochanteric ulcer. The general principle of excision of the ulcer and the trochanteric bursa is performed as described in Chap. 7. The prominent greater trochanter is shaved to reduce the size of the bone to eliminate the pressure point. Care should be taken not to cause an intertrochanteric fracture during the excision of the prominent bone. Post completion of this procedure, flap raising is performed; it is advisable to start distally the incision and dissection at the level of V apex because the fascia is superficial. Post incising the skin and the thin subcutaneous layer, the fascia of the iliotibial tract is exposed; then with a scalpel, it is incised and the vastus lateralis muscle is exposed to prevent detaching the fascia from the skin above it. An absorbable stitch is placed between the fascia and the skin; with a blunt dissection using the finger, it will make it easy to find the plane between the two fascias (iliotibial and vastus lateralis muscle fascia), and the skin of the marked flap is incised with a scalpel and the fascia can be incised with electrocautery or scalpel. The dissection is continued laterally dividing part of the fibers of the gluteus maximus at the level of the lower angle of the ulcer defect, and this step concludes the freeing of the flap laterally. Medially the dissection of incising the skin and the fascia continues until approaching a point where the pedicle is marked. If there is difficulty in advancing the flap in that circumstance a small division of the tensor fascia lata muscle to allow complete advancement of the flap into the ulcer defect. Two drains are placed under the flap, and the exits of these drains are distally above the knee joint and sutured to the skin by purse-string silk suture. When the flap is advanced in the defect, the flap donor site is closed in a V-Y fashion. It is very rare that the donor site cannot be closed; in that situation, a split skin graft is used. The flap is closed in three layers, the deep layer, dermal layer, and the skin. Figures 10.1, 10.2, 10.3, 10.4, 10.5, 10.6, and 10.7 show the steps of the surgical procedure.



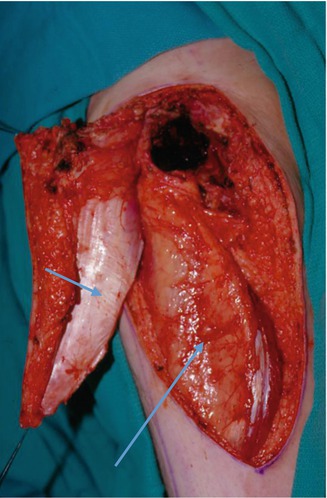



Fig. 10.2
X-ray of AP pelvis showing some calcification over the greater trochanter which can cause high pressure on the skin resulting in pressure ulcer

Fig. 10.3
Operative photograph showing the excised ulcer and the shaved trochanteric bone

Fig. 10.4
Operative photograph showing the defect of the excised ulcer and the shaved bone and complete dissection of the flap
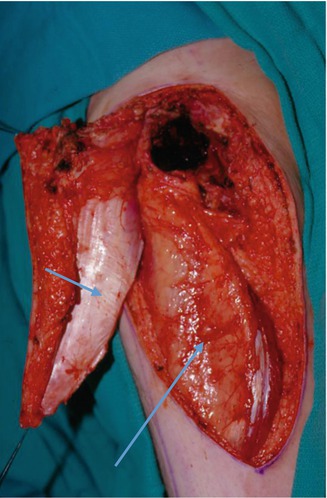
Fig. 10.5
Operative photograph showing the reflected flap to demonstrate the TFL fascia. The large muscle in the photo is the vastus lateralis muscle (long arrow). The short arrow indicates the TFL fascia

Fig. 10.6
Operative photograph showing the complete closure of the TFL flap in a V-Y fashion

Fig. 10.7
Photograph 6 weeks post-surgery showing complete healing of the flap
10.3 The Tensor Fascia Lata Rotation Flap
When the great trochanter is not located in the lateral anatomical position, secondary to pathological changes in the hip joint, the trochanter is rotated and located posteriorly. As a result, the V-Y advancement flap will not be suitable for this situation; therefore, the option is to utilize the tensor fascia lata in a rotation form. It is worth mentioning that it is well documented in literature that the length of tensor fascia flap will determine the viability of the distal part of the flap. It is recommended that when designing such a flap, it should not exceed 18 cm in length or it should be 8–10 cm above the femoral condyle; for vascular reason, the distal part of the fascia is supplied by perforators from the vastus lateralis muscle. Consequently, if a flap is designed, for example, to close an ischial area, the clinical picture of the vascular compromise may show as an epidermolysis of the skin and then will convert into a full-thickness skin loss. The recommendation in such circumstance is to delay the flap and then to raise the flap after 3 weeks. This procedure will direct the blood supply to be derived from the main pedicle to the distal part of the flap. Unfortunately, in our busy clinical practice, sometimes it is difficult to take the patient twice to the operating room, and sometimes we take the risk with minor morbidities because of the patient’s medical condition.
10.4 Surface Marking of the Flap
The anterior superior iliac spine is marked 8–10 cm; below that mark is the location of the vascular pedicle of the tensor fascia lata muscle. As mentioned previously, the tensor fascia boundary consists of the anterior border, a line drawn from the anterior superior iliac spine (ASIS) to the lateral condyle of the femur, and the posterior border located over the lateral intramuscular septum; the design of the flap is between the two borders as a rectangular-shaped flap. The width of the flap should be according to the diameter of the defect, the acceptable width is about 10 cm, and the length is not to exceed 8–10 cm above condyle of the femur; the arc of rotation of the flap is located at the vascular pedicle of the muscle.
10.4.1 Operative Technique
The ideal position of the patient on the operating table is lateral position, but if the position of the ulcer is more posterior and there are other ulcers to be closed at the same time, the prone position is preferred. The ulcer is excised and the bone is shaved as described in Chap. 7. The first step of the dissection is to find the tensor fascia lata tendon distally by making the transverse incision at the end of the flap by utilizing the scalpel to incise the skin and the fascia exposing the vastus lateralis muscle as described in the V-Y flap; dissection is continued anteromedially and laterally by dividing the skin and the fascia. The medial dissection is stopped at the level of the vascular pedicle, and this point represents the arc of the flap rotation; the dissection is carried on posterolaterally including dissection into the gluteus maximum muscle and part of the lateral intermuscular septum which is a rich vascular area. The flap is freed completely from the trochanteric area; the trochanteric bursa can be seen under the flap which should be excised completely to promote the flap healing and adhesion. Care should be taken not to violate the lateral intermuscular septum of the thigh which will expose the posterior thigh muscle; at this stage, the flap is rotated posteriorly to ensure if it can cover the defect without tension. This flap can be used to cover the posterior thigh and ischial defect. When the distal part of the flap shows doubtful perfusion especially if the flap was too long, to check the tissue perfusion, injection of (IV) fluorescence dye and utilizing ultraviolet light (wood light) intraoperatively to demonstrate the perfusion of the distal part of the flap by showing a yellow coloration of the skin which indicates sufficient vascularity and perfusion; when the color of the skin is dusky, it does indicate not a viable tissue. The flap donor site closure depends on the patient’s skin laxity and the width of the flap; if the donor site cannot be closed directly, skin graft should be applied. Two drains should be used and the exits of these drains located distally from the flap arc of rotation. Flap is closed in three layers, the deep layer, dermal, and skin. Figures 10.8




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








