Fig. 9.1
(a) Patient in the prone position with coccygeal ulcer; the essential topographical marking is on display. (b) Patient in the prone position in the lateral view, demonstrating the marking for the semicircular design passing over the greater trochanter for the gluteus maximus flaps
9.3.3 Operative Technique
The patient is placed in the prone position on the operating table. The ulcer is excised and the sacral bone is shaved as described in Chap. 8. When the coccygeal segment is prominent (especially at the sacrococcygeal angle) and is the direct cause of pressure or there is sign of infection, the distal segment of the coccygeal bone should be excised. The pelvic floor that covers the rectum is exposed, indicating the requirement for a durable coverage by muscle flap. The author’s recommendation in thin patients with a prominent posterior superior iliac spine is to shave these bones bilaterally for two reasons: to prevent development of a pressure ulcer at the site and so that the rotation flap used will not be under tension due to the prominent bone. The dissection of the gluteus maximus flap is performed as described in Chap. 8. The fasciocutaneous part of the flap that crosses the midline should be dissected from the strong fascia of the supra spinatus muscle and care should be taken not to raise the fascia or the muscle with the fasciocutaneous part of the gluteus maximus muscle. The supra spinatus muscle is identified by its fiber running in a longitudinal direction and it is covered by a strong sheath of fascia. The gluteus maximus fibers originate from the sacrum at the level of the posterior superior iliac spine and inferiorly from the lower part of the sacrum and the coccygeal bone. The muscle is dissected from these bones by an electrocautery with gentle tension on the muscle. To find the plane between the gluteus maximus and gluteus medius muscle, there are two options: the site of the posterior superior iliac spine or the lateral approach, as described in Chap. 8. At this stage of the dissection, the superior gluteal artery should be identified as it runs over the posterior surface of the muscle and is covered by transparent fascia. When the pedicle is identified, the dissection is directed laterally to release the muscle from its tendinous part. The extent of the dissection depends on the length required to rotate the flap medially as a musculocutaneous flap to cover the defect without tension. If there is tension, a back cut is made laterally and inferiorly. Two drains should be used, with the drains exiting laterally and inferiorly, one for the upper part of the defect and the other for the coccygeal part of the defect. The author recommends placing a few deep sutures between the posterior surface of the flap and the base of the defect to prevent the formation of bursa under the flap. The flap wound should be closed in three layers (deep, dermal, and skin). Figures 9.2, 9.3, 9.4, 9.5, 9.6, and 9.7 show operative details of the flap.






Fig. 9.2
Patient in the prone position after excision of the ulcer and shaving of the coccygeal bone

Fig. 9.3
The excised ulcer
Fig. 9.4
Dissection of the gluteus maximus flap, short arrow showing the fasciocutaneous part of the flap, long arrow indicates the anatomical demarcation of the gluteus maximus muscle

Fig. 9.5
Complete rotation of the gluteus maximus flap to cover the defect

Fig. 9.6
Sutured flap in place

Fig. 9.7
Photograph showing complete healing at 6 weeks post-surgery
9.4 Bilateral Gluteus Maximus Musculocutaneous Rotation Flap
In many cases, an extensive sacrococcygeal ulcer cannot be closed by a single gluteus maximus flap and it is necessary to raise bilateral flaps. This procedure cannot be performed in ambulatory patients because of the residual functional deficit in the muscle’s function. The operative technique is the same as when utilizing the gluteus maximus as a musculocutaneous flap. When an extensive ulcer is present, there is a strong indication for a diverting colostomy, which should be performed before flap surgery. One method of insetting the bilateral flap to cover the defect is accomplished by rotating the two flaps toward the midline, with each flap covering half of the ulcer defect. The only disadvantage of this method is that the seam of the two flaps is in the midline, which may become a weak point for breakdown. The posterior surface of the two flaps should be sutured to the base to prevent sliding of the flaps and the formation of bursa under the flaps. Another method of insetting the flaps, which the author prefers to avoid the previously mentioned risk of a midline breakdown, is to transpose the flaps. The flap that is more mobile is rotated all the way inferiorly to cover the defect and the other flap is rotated to cover the superior defect of the inferiorly rotated flap.
Another technique that can be adapted to prevent breakdown between the seam of the two flaps is to deepithilize the medial side of one flap and to inset that part under the other flap’s edge, like a “double-breasted” closure, to promote healing at an early and later stage of the flap surgery (Figs. 9.8, 9.9, 9.10, 9.11, 9.12, 9.13, 9.14, and 9.15).

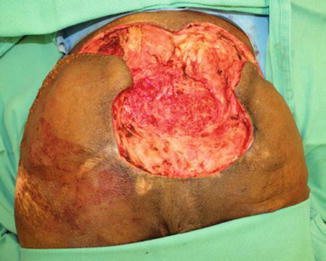






Fig. 9.8
Operative photograph showing the patient in the prone position with extensive recurrent sacrococcygeal ulcer. This patient had previous flap surgery; for this reason, we chose to utilize the bilateral gluteus maximus rotation flap
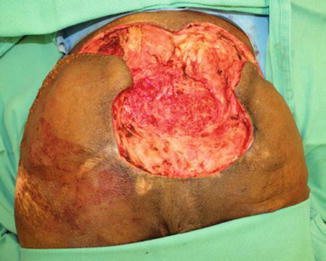
Fig. 9.9
Operative photograph showing excision of the ulcer and dissection of bilateral gluteal flap
Fig. 9.10
Operative photograph showing dissection of the gluteus maximus and separation between the maximus and the medius, arrow indicates the plane

Fig. 9.11
Operative photograph showing the dissected gluteus maximus of the other side

Fig. 9.12
Operative photograph showing the dissected bilateral gluteal flap with the transposition of the flaps, one flap to cover the ulcer and the other flap to cover the rest of the defect

Fig. 9.13
Operative photograph showing complete suturing of the flaps

Fig. 9.14
Operative photograph showing complete suturing of the flap, lateral view

Fig. 9.15
Photograph showing complete healing of the flaps 6 weeks post-surgery
9.5 Gluteus Maximus Advancement Island Flap
The gluteus maximus advancement island flap is a musculocutaneous flap. The vascularity of the skin island is based on the perforators from the gluteus maximus muscle underneath it. The flap can be utilized as a single, one-sided flap or a bilateral flap in extensive ulceration. This flap has been described with many modifications for different indications in ambulatory and nonambulatory patients to close sacrococcygeal ulceration [8, 17–19]. If the defect is greater than 8 cm in diameter, a bilateral island flap should be utilized to close the defect. This flap is technically easy to perform compared with a gluteus maximus rotation flap. In addition, with less blood loss and shorter operative time, the author’s opinion is that this flap is an excellent option for ambulatory and elderly patients.
9.5.1 Operative Technique
The patient is placed in the prone position on the operating table. If the ulcer is extensive and there is close proximity to the anus, then a diverting colostomy should be performed before flap surgery. A temporary purse string suture is placed around the anus to close it during surgery to prevent soiling on the wound. The ulcer and the bone are excised and shaved as described in Chap. 8. The marking for important landmarks is performed as described for the gluteus maximus rotation flap, and the design of the flap as an island of the skin is marked in an oval shape in the horizontal direction. The base of the flap is within the border of the ulcer and the apex of the flap is in the lateral landmark of the muscle (Fig. 9.16).


Fig. 9.16
Operative photograph patient in the prone position showing the design of the island flap for the closure of the coccygeal ulcer
Which side to mark the flap on depends on the side the where the ulcer is undermined, which is the appropriate side to utilize. A scalpel is used for skin incision and then an electrocautery is used for incising the subcutaneous layer and the deep fascia that covers the gluteus maximus muscle. When the muscle is exposed, the gluteal fibers are incised against the fibers’ direction in the muscle. It is important to release the muscle at the apex of the flap laterally. The flap is then tested to see whether it can be advanced medially without tension and if more muscle fibers need to be transected laterally. In addition, the origin of the muscle medially from the sacrococcygeal segment should be released. This step makes it possible to advance the flap medially to cover the defect. Care should be taken in ambulatory patients not to transect all the muscle fibers at the flap apex (i.e., laterally). This helps to preserve the function of the muscle. Two drains are placed, one superiorly and the second inferiorly. The exit of these drains should be placed laterally near the apex of the flap. The flap is advanced into the defect. The deep sutures are important to approximate between the gluteus maximus muscle of both sides passing the midline. If this step is difficult to achieve, mobilization of the gluteus maximus of other side is performed to assist in closing the deep layer without tension. The flap donor site is closed in a V-Y fashion and the flap is closed in three layers. Figures 9.16, 9.17, 9.18, 9.19, and 9.20 show steps in the surgical procedure.

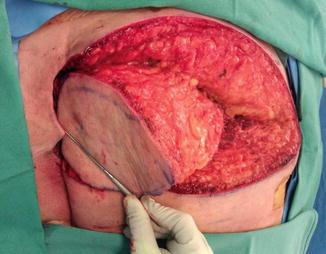


Fig. 9.17
Operative photograph showing the excision of the ulcer, shaving of the bone, and dissection of the island flap
Fig. 9.18
Operative photograph close-up view showing the shaving of the coccygeal bone. Arrow indicates the location of the bone
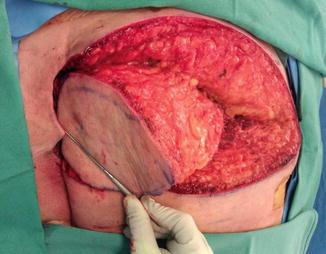
Fig. 9.19
Operative photograph showing the complete dissection of the island laterally and the advancement of the island to cover the defect

Fig. 9.20
Operative photograph showing complete closure of the flap
9.6 Bilateral Gluteus Maximus Island Advancement Flap
When the defect is extensive and a unilateral flap is not adequate to close the defect, a bilateral island flap is used. The operative technique is the same as described previously. Both flaps are advanced toward the midline and the two side muscles are sutured together in the midline. As a result, the defect is covered by muscle. Anatomically, there is no muscle covering the area; therefore, by this method a healthy tissue padding is added to cover the sacrococcygeal area. The donor site of both flaps is closed in a V-Y fashion. Two drains are used and the exit is laterally on one side. Figures 9.21, 9.22, 9.23, 9.24, 9.25, 9.26, and 9.27 show the surgical steps.







Fig. 9.21
Operative photograph showing the design of a bilateral gluteus maximus island flap for an extensive sacrococcygeal ulcer. Note: patient had recent surgery for a Girdlestone procedure and ischial ulcer, which are closed by multiple flaps

Fig. 9.22
Operative photograph showing the excised ulcer and the shaving of the coccygeal bone

Fig. 9.23
Operative photograph showing the complete dissection of the bilateral island flap

Fig. 9.24
Operative photograph showing the lateral dissection of the island flap

Fig. 9.25
Operative photograph showing the approximation of the two islands to the midline

Fig. 9.26
Operative photograph showing complete closure of the two islands










