(1)
Yotsuya Medical Cube, Chiyoda-ku, Tokyo, Japan
Basic Principles
Reconstruction of the skin of the finger trunk area doesn’t require reconstruction of sensory function, but it is preferable to use skin with similar quality, so the first priority is to see if reconstruction is possible using similar skin.
If it is not possible to elevate a flap from the same finger, then transfer of skin flaps from adjoining fingers or from other areas of the hand are considered.
It is possible to perform skin graft on the dorsum of the hand, however for reconstruction of the skin on the palm side, a flap with suitable skin thickness is chosen.
Selectable Flaps and Surgical Procedures
Z plastyDigitolateral flapHeterodigital arterial flapCross finger flapSpinner flapReverse flow radial forearm flapReverse flow metacarpal arterial flapKite flapFree venous flapFree hemi pulp flap transferUlnar parametacarpal flapDorsolateral flapModified Kleinert methodDigital arterial adipofascial flap and Skin graftDouble-opposing digitolateral flapBi-lobed palmar flapThe difficulty level of each surgical procedure is shown subsequent to the procedure title (e.g., Level of Difficulty: 2). The levels range from 1 to 5, with level 1 indicating a preliminary level and level 5 indicating a very advanced level.
7.1 Z Plasty (Level of Difficulty: 1)
Information
Vascular pedicle Subcutaneous vascular plexus
Caution Auxiliary incisions are made in the skin creases of the finger to avoid creating new contracture. Z plasty that is too small doesn’t alleviate contracture and can actually cause new contracture. Z plasty of 1 cm is desirable
7.1.1 Operation Procedures

Fig. 7.1
Procedure 1: Longitudinal scar contracture is recognized in the palmar side of the ring finger

Fig. 7.2
Procedure 2: Several successive 1 cm Z plasty are designed on the finger
Note
Auxiliary incisions are made so as to avoid cutting the skin crease at right angles.



Fig. 7.3
Procedure 3: An incision is made and subcutaneous scar tissue is resected, and the contracture released

Fig. 7.4
Procedure 4: The small transferred flap is sutured
7.2 Digitolateral Flap (Level of Difficulty: 2)
Information
Vascular pedicle The digital artery is not included, but instead the subcutaneous vascular plexus of the middle of the finger is the main circulation
Size When creating in the proximal phalanx area, the length can be up to the PIP joint crease, and if width is less than 10 mm, it is possible to directly suture the donor site closed. When creating in the middle phalanx area, the length can be up to the DIP crease, however suturing the donor site closed is difficult and a skin graft is required.
Advantage Practical for use in covering skin defects due to releasing contracture in the palmar side of the finger base or the PIP crease. Major vascular pedicles are not included, but it is possible to create a thin long flap, and there are no restrictions on length to width ratio. The skin flap can be made normal flow or reverse flow, but the blood flow in reverse flow flaps is instable in some cases. There is also a method (Leuder’s flap) of transferring the normal flow (or reverse flow) flap created in the middle phalanx area to cover a skin defect area on the dorsal DIP and PIP joints.
7.2.1 Operation Procedures

Fig. 7.5
Procedure 1: Due to scar contracture on the palmar side of the ring/little finger, unable to sufficiently extend PIP joint. A long scar contracture is present from the base of the ring finger to the DIP joint

Fig. 7.6
Procedure 2: A digitolateral flap is designed from the ulnar proximal phalanx area for the base of the ring finger, and from the radial middle phalanx area for the PIP crease
Note
Z plasty is designed for the little finger.



Fig. 7.7
Procedure 3: The digitolateral flap is detached from above the fascia or from above the flexor tendons, however the digital arteries or digital nerves are not included. A sufficient amount of skin flap is removed up to the base, rotated 90° and transferred to the palmar side

Fig. 7.8
Procedure 4: Appearance after transferring the skin flap. The proximal phalangeal donor site can be sutured closed
Note
In this case example, a middle phalangeal skin flap donor site was also possible, so it was sutured closed.
Tips
Don’t use excessive force to close the donor site
When elevating a digitolateral flap from the lateral middle phalanx area, many cases require a skin graft in order to be closed.


7.3 Reverse Digitolateral Flap (Level of Difficulty: 2)
Information
Vascular pedicle The digital artery is not included, but instead the subcutaneous vascular plexus of the lateral finger is the main circulation
Siz: When creating in the proximal phalanx area with a distal pedicle, the length can be up to the length of the proximal phalanx area of the finger, and if width is around 10 mm, it is possible to directly suture the donor site closed. When creating in the intermediate phalanx area, the length can be up to the length of the middle phalanx area, however suturing the donor site closed is difficult and a skin graft is required.
Advantage Practical for use in covering skin defects following release of contracture in the palmar side of the finger base or the PIP crease. Major vascular pedicles are not included, but it is possible to create a long thin flap, and there are no restrictions on length to width ratio. The blood flow in reverse flow flaps is instable in some cases


7.3.1 Operation Procedures

Fig. 7.9
Procedure 1: A scar contracture is present in the longitudinal direction at the palmar side of the finger PIP joint
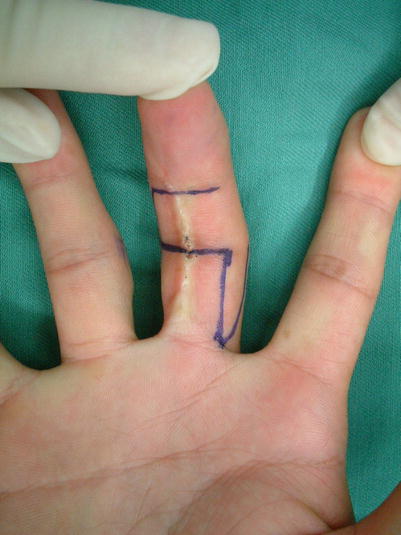
Fig. 7.10
Procedure 2: A distal pedicle flap is designed in the lateral side of the middle and proximal phalanx area
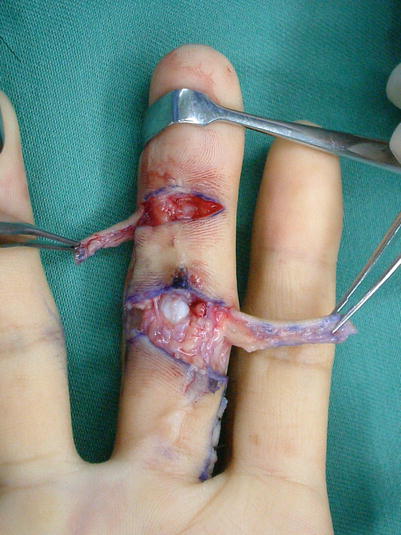
Fig. 7.11
Procedure 3: A lateral incision is made along the DIP and PIP crease and the contracture released. The flap is then elevated above the periosteum and rotated 90° and transferred to the palmar side

Fig. 7.12
Procedure 4: The skin flap is sutured in place. The proximal phalanx donor site is sutured closed. In many cases a skin graft is conducted for the lateral middle phalanx donor site
Tips
Observe progress for 2 weeks without performing debridement
Occasionally digitolateral flaps transferred to the distal pedicle are subject to surface necrosis at the edge of the flap, but in many cases, if treated conservatively and progress is observed for 2 weeks, epithelization occurs without need for debridement.


7.4 Heterodigital Arterial Flap (1) (Level of Difficulty: 3)
Information
Vascular pedicle Digital artery of adjoining finger and surrounding fine veins
Size From the skin above the digital artery to the dorsum of the finger
Caution A thick vascular pedicle including the fine veins surrounding the digital artery pedicle is harvested. It is a requirement that the contralateral digital artery of the adjoining finger be retained.


7.4.1 Operation Procedures

Fig. 7.13
Procedure 1: Skin defect present on dorsum of finger accompanying exposure of extensor tendons following re-attachment

Fig. 7.14
Procedure 2: The skin flap is designed from the lateral center of the adjoining finger onto the dorsum of the finger

Fig. 7.15
Procedure 3: The digital nerve is retained and a thick vascular pedicle including the digital artery and the surrounding fat tissue is created and elevated. The skin flap is detached from above the extensor tendon

Fig. 7.16
Procedure 4: The skin flap is transferred and a skin graft conducted for the donor site. A tie-over bolster dressing is applied. (Part of photos reproduced from Hirase, Y.: Reconstruction using vascularized skin flaps: Plastic Surgery for Injuries (edited by Anze, M.) pp 121–126, Kokuseido, Tokyo, 2007)
Tips
Use the distal part of the digital artery of the elevated flap for reconstructing circulation of the reconstructed finger
By conducting anastomosis of the distal part of the vascular pedicle of the elevated heterodigital flap to the artery in the recipient site, it is possible to simultaneously reconstruct blood flow of the reconstructed finger.
7.5 Heterodigital Artery Flap (2) – Transfer to Skin Defect of Thumb (Level of Difficulty: 3)
Information
Vascular pedicle Digital artery and surrounding small veins on ulnar side of middle finger or ulnar side of ring finger.
Size From the skin above the digital artery to the dorsum of the finger.
Caution A thick vascular pedicle is harvested with inclusion of small veins surrounding the digital arterial pedicle. It is a requirement that the digital artery of the contralateral finger to the donor finger be retained.
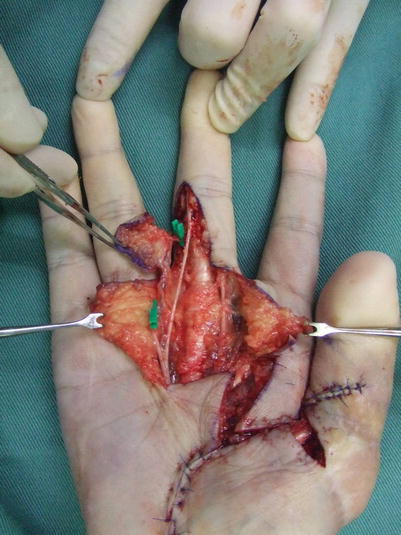


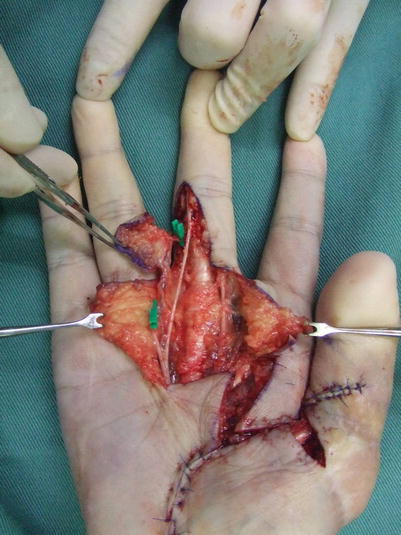

Fig. 7.17
Procedure 1: Skin defect accompanied by exposure of the flexor pollicis longus muscle tendon at the base of the palmar side of the thumb

Fig. 7.18
Procedure 2: A hetero-digital arterial flap is designed on the ulnar side of the middle finger
Note
The ulnar side of the ring finger can also be used as the donor site.
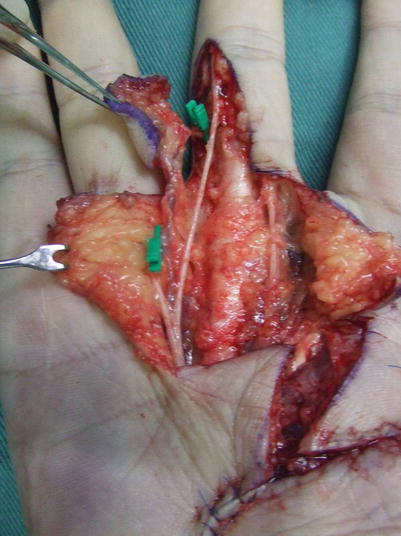


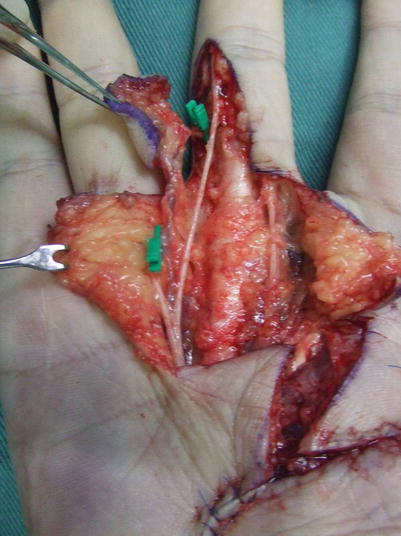
Fig. 7.19
Procedure 3: The digital nerve alone is retained/detached and separated from the neurovascular pedicle of the finger and the flap is elevated with only the vascular pedicle. Further distal of the proper digital artery flap, the arterial pedicle is ligated and cut at two branch locations to the palmar digital artery of the adjoining finger

Fig. 7.20
Procedure 4: A zig zag incision is made in the palm, and the flap vascular pedicle is dissected up to the arterial arch

Fig. 7.21
Procedure 5: The flap is transferred to the base of the thumb and a skin graft is conducted on the donor site. A tie-over compression is applied
7.6 Cross Finger Flap (Level of Difficulty: 2)
Information
Vascular pedicle Dorsal branch of digital artery
Disadvantage There is a problem with skin texture due to use of skin with different quality. Also, not a sensory flap.
Caution A long flap should be dissected, exceeding the lateral center of the contralateral finger, so that the flap doesn’t bend over on itself. The hand is placed in syndactyly fashion for 2 weeks, and it is easy for the finger joints to develop contracture, so active and passive exercise should be commenced soon after the flap is separated.
7.6.1 Operation Procedures

Fig. 7.22
Procedure 1: A skin defect is present with exposure of tendons on the palmar side of the index finger

Fig. 7.23
Procedure 2: The flap on the dorsum of the finger is detached to a good length above the extensor tendon and transferred to the palmar side
Note
The flap is detached nearly up to the palmar digital nerve/vascular pedicle before transfer, to prevent it from folding over on itself.


Fig. 7.24
Procedure 3: A skin graft is conducted on the donor site, and a tie-over compression applied. The flap is separated 2 weeks later
7.7 Spinner Flap (Level of Difficulty: 1)
Information
Vascular pedicle No specific arteries are included
Size Created in the radial lateral side of the index finger, however when creating skin flaps exceeding a width of 20 mm, it is necessary to conduct a skin graft as reefing is difficult.
The tip of the skin flap is made distal to the PIP joint
Advantage Simple with stable blood flow. Specific arteries are not included, however there is no problem if the width to length ratio exceeds 1:3.
Disadvantage In cases where large soft tissue is required, skin graft is required for the donor site which can become somewhat obvious.
7.7.1 Operation Procedures