Fig. 8.1
Creation of microsurgical anastomoses between the T10 and S2 ventral roots
The patients were moved to rehabilitation clinics 2 weeks after surgery. Patient follow-up was scheduled 6, 12, 18, and 24 months after the operation. At these visits, urodynamic studies, including detection of maximum detrusor pressure, maximum flow, and sphincter resistance, were performed and questionnaires were completed. From month 12 onwards, the patients were directed to scratch or gently squeeze the T10 dermatome when the bladder was full to initiate voiding. When there was evidence of significant recovery of bladder function, renal function was re-evaluated.
8.3.4 Case Report
A 43-year-old woman was referred for evaluation and treatment of atonic bladder caused by a conus medullaris injury in July 2000. She had fallen from an elevated height, which resulted in a compression fracture of the L1 vertebra and subsequently complete paraplegia. The patient complained of urinary retention and anuria, which required insertion of an indwelling urinary catheter. As expected, a serious urinary infection had developed, for which antibiotic therapy was instituted. Surgical reconstruction of the bladder reflex pathway was scheduled and performed 4 months after the injury. At this time, the medial sural cutaneous nerve was cut and anastomosed with the T10 and S2 ventral roots (Fig. 8.2).
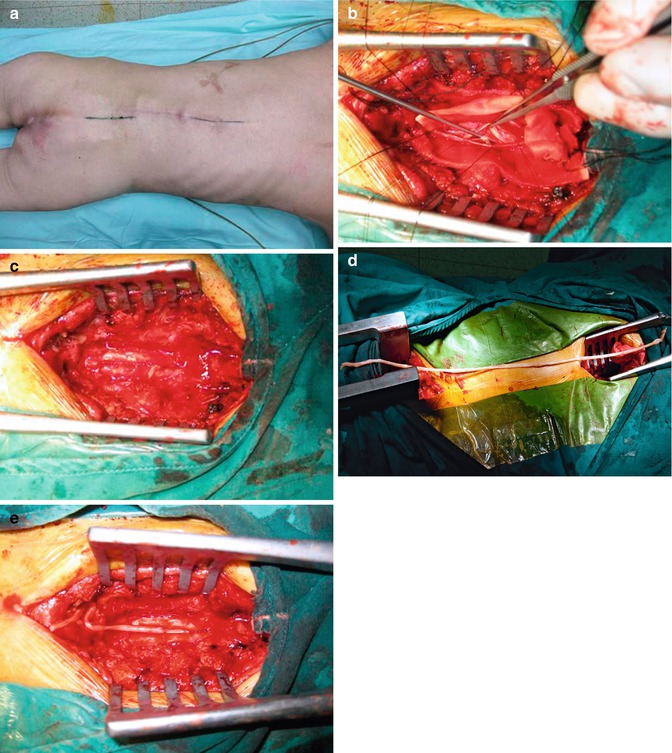
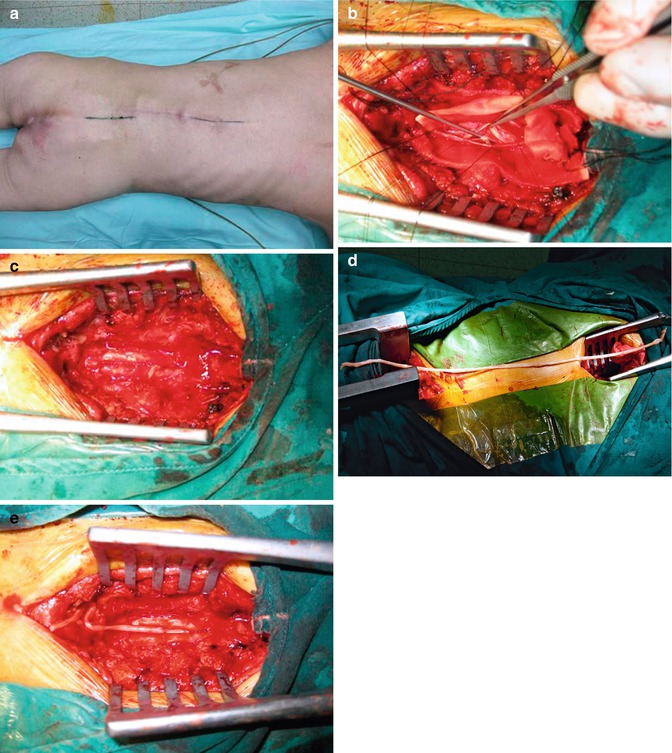
Fig. 8.2
Images of the surgical procedure used for reconstruction of the bladder reflex pathway in a 43-year-old woman. (a) Standard laminectomies from L5 to S3 and from T10 to T12 were performed with the patient lying in the prone position. (b) After the ventral root of T10 was identified and found to be functional, it was transected. (c) The dura was then closed, leaving the T10 ventral root outside. (d) A sural cutaneous nerve, about 30 cm in length, was taken for the nerve graft. (e) The T10 and S2 ventral roots were then anastomosed through a nerve graft
After the reconstructive procedure, the indwelling urinary catheter was kept in place for 1.5 years and caused multiple urinary system infections. At 2 years after the surgery, the patient experienced recovery of bladder storage and voiding functions. She could void by scratching her T10 dermatome. To date, this patient has been followed for 72 months and the urethral catheter has been removed. She has regained the sensation of bladder fullness, can contract the abdominal muscle, and is capable of complete urination without any difficulty. The total urinary output increased from 500 to 800 ml per day. According to the results of urodynamic analysis, the flow rate of patient’s maximal urine was 38 ml/s; urinary output, 596 ml/void; residual urine, 30 ml; vesical pressure, 145 cm H2O; abdominal pressure, 31 cm H2O; and detrusor pressure, 114 cm H2O (Fig. 8.3). The detrusor had acquired the nerve reflex since the external sphincter was denervated. Hence, the recovery of urinary function was mainly contributed to detrusor contraction, instead of bladder compression through the abdominal muscles.
Fig. 8.3
Urine pressure and flow diagram from the urodynamic test. (a) Preoperative study showed that the detrusor had no reflection but the external sphincter was denervated. (b) Postoperative study showed that the detrusor had regained nerve reflex when the external sphincter was denervated: intravesical pressure increased quickly while abdominal pressure did not increase significantly
8.3.5 Discussion
Based on our preclinical findings in the rodent model [18], we performed spinal ventral root anastomoses in ten paraplegic patients presenting with traumatic lesions of the conus medullaris. Seven of the patients recovered urinary function 2 years after undergoing the surgery of reflex pathway reconstruction [8




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







