ACL Reconstruction and Extra-articular Tenodesis
Keywords
• ACL reconstruction • Extra-articular tenodesis • ACL revision
Key Points
Introduction
Historically, anterior laxity in ACL-deficient knees was treated surgically by isolated extra-articular tenodesis, as described by Lemaire or MacIntosh.1,2 This procedure effectively limited rotation of the tibial plateau relative to the femur; however, isolated extra-articular reconstructions provided only moderate control of anterior laxity. The procedure was largely abandoned when single-bundle intra-articular ACL reconstruction emerged as the gold standard surgical treatment of ACL tear. Some patients, however, experience persistent rotatory laxity after such reconstructions. Double-bundle ACL reconstruction was developed in part to allow improved control of rotational laxity through independent reconstruction and tensioning of the posterolateral (PL) bundle of the ACL. Although this procedure has been shown to produce excellent results in the hands of experienced surgeons, it is technically challenging, particularly in patients with smaller ACL footprints. Excessive rotatory laxity can also be controlled by the addition of an extra-articular lateral tenodesis to a single-bundle intra-articular ACL reconstruction. Recent studies report comparable results of double-bundle ACL reconstruction and single-bundle reconstruction augmented with lateral extra-articular tenodesis. The aims of this article are to review the clinical indications, surgical techniques, and reported results of augmentation of intra-articular ACL reconstruction with lateral extra-articular tenodesis.
Background
Single-Bundle ACL Reconstruction
Single-bundle ACL reconstruction is performed to restore control of anterior and rotational knee laxity that is lost with rupture of the native ACL. Stabilizing the knee aims to prevent further injury to articular cartilage and the menisci and to maximize patient function. This technique provides good to excellent results in most cases and reliably restores function in activities of daily living and athletic activities in most cases. A meta-analysis of 48 studies (5770 participants) on return to sport after ACL reconstruction showed that 90% of participants achieved normal or nearly normal knee function; 82% of participants had returned to some kind of sports participation, 63% had returned to their preinjury level of participation; and 44% had returned to competitive sport at final follow-up.3 Recurrent or persistent instability after ACL reconstruction, however, several studies report 11% to 30% of recurrent and persistent instability after ACL reconstruction.4–6
Failure of ACL Reconstruction
Reasons for instability after ACL reconstruction are varied7 and include technical error (frequently tunnel malposition or failure to address associated injuries), inadequate graft material or fixation, traumatic reinjuries, and biologic failure.8 Recurrent or persistent laxity, in particular rotational laxity associated with a positive pivot shift test, has been associated with poorer patient-reported outcomes after ACL reconstruction.4 This rotatory laxity has been reported even without failure of the ACL graft, suggesting that in some patients a single-bundle intra-articular reconstruction is not sufficient to completely restore rotational knee stability.9
Double-Bundle ACL Reconstruction
Several approaches have been developed in recent years to improve rotational control after ACL reconstruction. First, the concept of anatomic ACL reconstruction has been advanced as a possible solution to persistent rotational laxity. The native ACL is composed of 2 bundles: the anteromedial (AM) bundle and the PL bundle. Traditional single-bundle ACL reconstructions often resulted in nonanatomic vertical graft placement or at best only recreated the AM bundle.10 Vertical graft placement fails to recreate the PL bundle (which functions to resist tibial internal rotation near full-knee extension), possibly contributing to persistent rotatory laxity in some patients undergoing this procedure. More anatomically placed single-bundle reconstructions as well as anatomic double-bundle ACL reconstructions have been developed to better restore the function of the PL bundle. Biomechanical studies have demonstrated better rotational control with anatomic double-bundle reconstructions, leading to the increased popularity of these techniques.10,11 Clinical superiority of this technique, however, has not been definitively demonstrated.12
Lateral Extra-Articular Tenodesis
Another approach to improve rotational control after ACL reconstruction is based on the concept that anterolateral capsular injury is frequently associated with ACL tears. The capsular avulsion is termed a Segond fracture13,14 when associated with bony avulsion of the lateral tibial plateau but does not always include an osseous fragment. This lesion has been shown to be present in the vast majority of acute ACL injuries and its presence is associated with significantly increased rotational knee laxity. Furthermore, when chronic anterior laxity is left untreated, rotatory laxity can develop due to a progressive stretching of secondary restrains in the lateral aspect of the knee.15 This stretching can further increase anterior laxity. To address the contributions of anterolateral capsule injury to rotational knee laxity, some investigators have proposed the addition of a lateral extra-articular tenodesis to the standard intra-articular ACL reconstruction.16 Several techniques classically used for isolated lateral tenodesis have been modified and used as an adjunct to intra-articular ACL reconstruction in this manner. These combined procedures are advantageous for several reasons. First, the longer lever arm of the lateral reconstruction allowed for efficient control of tibial rotation. Second, the lateral tenodesis may effectively control rotational laxity even in the face of failure of the intra-articular graft, provided a backup for the intra-articular graft in such cases.17 Finally, the addition of a lateral tenodesis has been shown to decrease the stress seen by the associated intra-articular reconstruction by more than 40%.18 These advantages are especially useful in cases of revision ACL reconstruction. One contraindication to lateral extra-articular tenodesis is the presence of a PL corner injury. In such cases, the tenodesis may tether the tibia in a PL subluxated position.
Surgical techniques
Iliotibial Band
Lemaire procedure
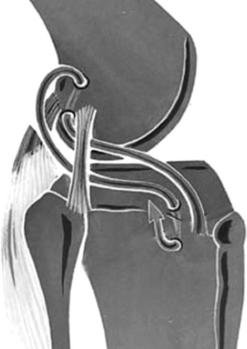
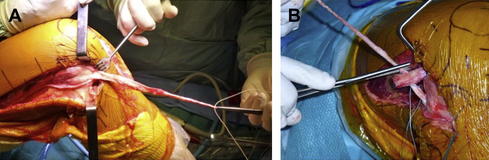
The Lemaire procedure was first described in 1967.1 This extra-articular tenodesis uses a strip of iliotibial band measuring 18 cm long and 1 cm wide that is left attached to the Gerdy tubercle. Two osseous tunnels are prepared to anchor this graft: the first is in the femur, just above the lateral epicondyle and proximal to the lateral collateral ligament (LCL) insertion; the other is through the Gerdy tubercle on the proximal lateral tibia. Once the strip of iliotibial band is harvested and the bony tunnels are prepared, the graft is passed under the LCL, through the femoral bone tunnel, and back under the LCL and finally inserted into Gerdy tubercle via the second bone tunnel. Graft fixation is done at 30° of knee flexion, with neutral rotation (Fig. 1). When this technique is performed in association with a standard ACL reconstruction, a technical problem can be encountered in the lateral distal femur when the femoral tunnel made for the ACL graft interferes with the femoral tunnel made to anchor the iliotibial band graft. To avoid this problem, the bone-tendon-bone ACL graft can be prepared with a hole in the tibial bone block that is fixed in the femoral tunnel. The iliotibial band graft (Fig. 2A) can be passed through this bone block and is thus automatically anchored in the femur when the ACL graft is fixed in the femur (see Fig. 2B).
Modified Lemaire procedure
Christel and Djian19 described a modified Lemaire procedure in order to simplify the classic Lemaire technique. First, the length of the iliotibial band graft is diminished in order to decrease the required skin incision and subcutaneous dissection on the lateral thigh. Christel and Djian described a graft measuring 75 mm long and 12 mm wide, again left attached distally on the Gerdy tubercle. The proximal portion of the graft is then passed to an isometric point on the lateral femoral condyle determined by a compass and secured in a femoral tunnel with an interference screw. To avoid possible devascularization of the LCL, the graft is not passed under the ligament. The graft is twisted 180° because this method has been shown by Draganish and colleagues17 to yield more homogenous graft forces and better isometry.
MacIntosh procedure
The first described MacIntosh procedure2 (MacIntosh 1) was similar to the Lemaire procedure; however, femoral fixation was achieved not via a bone tunnel but through suture fixation to the lateral intermuscular septum. This procedure was modified (MacIntosh 2) to include passage of the graft into the joint via the over-the-top position, through the notch, and into a tibial tunnel. In 1979, the Marshall-MacIntosh procedure20 (MacIntosh 3) was described. The central third of the entire extensor mechanism is harvested with a wider portion taken from the prepatellar aponeurotic tissue. This graft was used to reconstruct the intra-articular ACL via a tibial tunnel and passage over the top of the lateral femoral condyle, and to complete the extra-articular tenodesis by fixing it in Gerdy tubercule. This same concept of using one graft to reconstruct both the ACL and perform the extra-articular tenodesis is used now with hamstring tendons (discussed later), although current techniques use a femoral tunnel rather than passing the tendons over the top.
Hamstrings
Hamstrings for both ACL reconstruction and extra-articular tenodesis
Colombet,21 in 2011, described a mini-invasive technique using the same hamstring graft for intra-articular reconstruction and extra-articular tenodesis. The gracilis and semitendinosus tendons are harvested and stripped of muscle fibers. Then, the graft is prepared in 1 of 2 possible configurations according to the length or the tendons: 4 + 2 or 2 + 2. The overall length graft should measure at least 21 cm. When the gracilis and semitendinosus tendons are long enough to form a 9-cm segment containing 4 strands (which are used to reconstruct the ACL) and a 12-cm segment containing 2 strands (which are used to do the extra-articular tenodesis), the 4 + 2 configuration is used. If not, the 2 + 2 configuration is used. The tibial and femoral tunnel tunnels are drilled via an outside-in approach and absorbable interference screws are used in both tunnels to secure the graft. The remaining extra-articular graft is then passed under the iliotibial band and anchored with an interference screw in a tibial tunnel made in the Gerdy tubercle. Navigation can be used to optimize tunnel placement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree