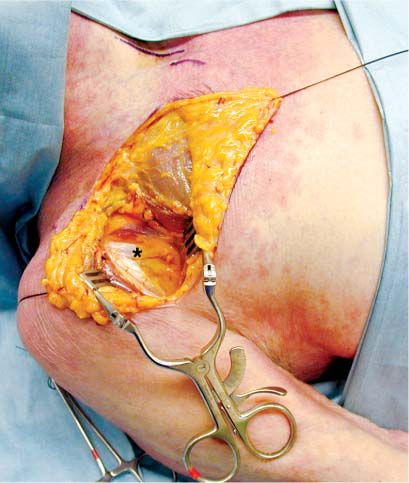
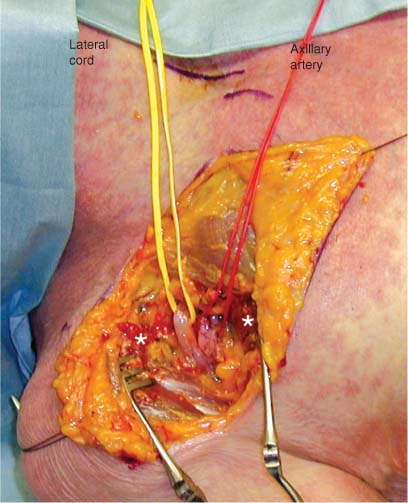
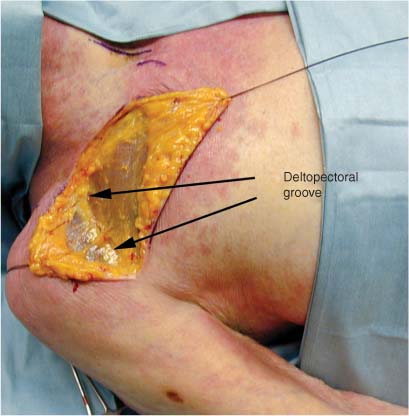
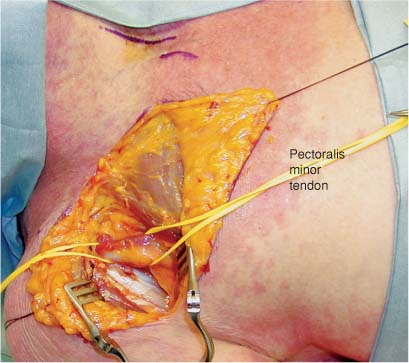
5 The radial nerve arises from the posterior cord of the brachial plexus. In the proximal third of the arm the nerve descends posterior to the brachial artery and anterior to the long head of the triceps muscle.1 Distally, at the level of the proximal and middle third portions of the humerus, the nerve moves laterally into the interval between the long and medial heads of the triceps. The nerve then passes between the medial and lateral heads of the triceps and reaches the lateral intermuscular septum lying adjacent to the spiral groove of the humerus. It then pierces the intermuscular septum ~10 cm above the lateral humeral epicondyle, leaving the extensor compartment of the arm and passing into the flexor compartment of the arm. Distally in the arm the nerve lies in the interval between the brachialis muscle and the brachioradialis muscle. Once past the cubital fossa it lies between the brachioradialis muscle and the extensor carpi radialis longus muscle. In the arm the nerve innervates the triceps muscle, including the long, lateral, and medial heads as well as the brachioradialis, the extensor carpi radialis longus, and the anconeus muscles. It also gives off three cutaneous nerves and several articular branches that supply the elbow joint. As the main trunk of the radial nerve passes anterior to the lateral epicondyle it lies posterior to the brachioradialis muscle. Within an area 3 cm proximal or distal to the elbow joint it divides into superficial and deep terminal branches. The superficial branch passes anterior to the supinator muscle in the forearm and lies on the deep surface of the brachioradialis muscle. This branch goes on to innervate the extensor carpi radialis brevis muscle. At ~10 to 15 cm distal to the elbow joint the superficial branch moves from the deep surface of the brachioradialis muscle and emerges from between the tendon of that muscle and the tendon of the extensor carpi radialis longus. The nerve travels in this superficial position distally in the forearm to supply sensation to the anatomic “snuff box” on the dorsum of the hand. Once divided from the radial nerve, the deep branch or posterior interosseous nerve enters an area described as the radial tunnel.2 The nerve courses obliquely through the supinator muscle and into the extensor compartment of the forearm. The nerve lies between the abductor pollicis longus muscle deeply and the extensor carpi ulnaris, extensor digiti minimi, and extensor digitorum muscles superficially. In the distal forearm the nerve passes superficial to the extensor pollicis brevis and deep to the extensor pollicis longus muscles. Penetrating either over or through the extensor pollicis brevis muscle, the nerve comes to lie on the interosseous membrane between the radius and ulna. It continues on to divide into terminal branches that provide sensory innervation to the wrist. The posterior interosseous nerve innervates the supinator, extensor carpi ulnaris, extensor digitorum, abductor pollicis longus, extensor pollicis longus, extensor pollicis brevis, extensor digiti minimi, and extensor indicis muscles. If access to only the very most proximal portion of the radial nerve is required, that is, at the level of its takeoff from the posterior cord to its egress through the triangular interval, the patient may be placed in the supine position. The approach to this portion of the radial nerve is via a standard infraclavicular incision described in detail in Chapter 1. An incision is laid out along the lateral two thirds of the clavicle and down onto the deltopectoral groove (Fig. 5-1). The skin should be infiltrated with a vasoconstrictive agent such as lidocaine 1% with epinephrine in a 1:100,000 concentration prior to incision. The skin and subcutaneous tissue are then divided exposing the deltopectoral groove (Fig. 5-2). The deltopectoral groove is opened, the cephalic vein ligated, and the tendon of the pectoralis minor muscle is exposed (Figs. 5-3 and 5-4). The pectoralis minor tendon is retracted after being divided and tagged for reapproximation at the conclusion of the procedure. Once retracted the lateral cord and the adjacent axillary artery are visible (Fig. 5-5). The lateral cord is seen to divide into the musculocutaneous nerve to the biceps and the lateral cord contribution to the median nerve (Fig. 5-6). For full exposure of the radial and/or axillary nerve of the posterior cord, the lateral cord may require retraction in a medial direction. It is therefore prudent to dissect free the musculocutaneous nerve so that it is not unduly retracted or injured beneath a retractor when exposing the posterior cord. The posterior cord is then dissected free from just medial and posterior to the lateral cord (Fig. 5-7). The posterior cord is then seen to divide into the axillary nerve and the radial nerve (Fig. 5-8). The radial nerve then continues on out of the axilla via the triangular interval between the medial and long head of the triceps muscle. If exposure much beyond this interval is required, a posterior approach to the radial nerve is necessary. FIGURE 5-1 Incision laid out for exposure of proximal radial nerve. This is the same incision as the infraclavicular approach described in more detail in Chapter 1. FIGURE 5-2 Skin and subcutaneous tissue divided exposing the deltopectoral groove. FIGURE 5-3 Deltopectoral groove opened, cephalic vein ligated, and pectoralis minor tendon exposed (*). FIGURE 5-4 Pectoralis minor tendon elevated between two vessel loops. The ends should be tagged prior to division to facilitate reapproximation at the conclusion of the procedure.
RADIAL NERVE AND POSTERIOR INTEROSSEOUS NERVE
ANATOMY
In Arm
In Forearm
POSITIONING AND SURGICAL EXPOSURE
In Arm

< div class='tao-gold-member'>
Radial Nerve and Posterior Interosseous Nerve
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree