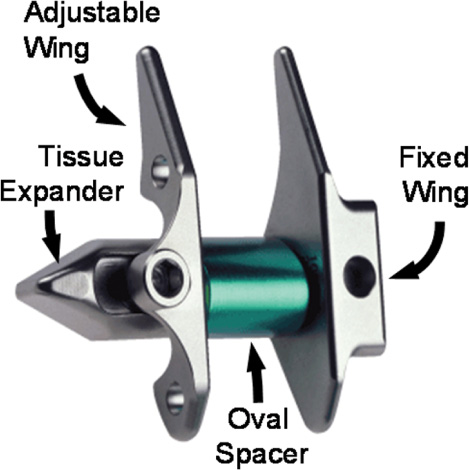
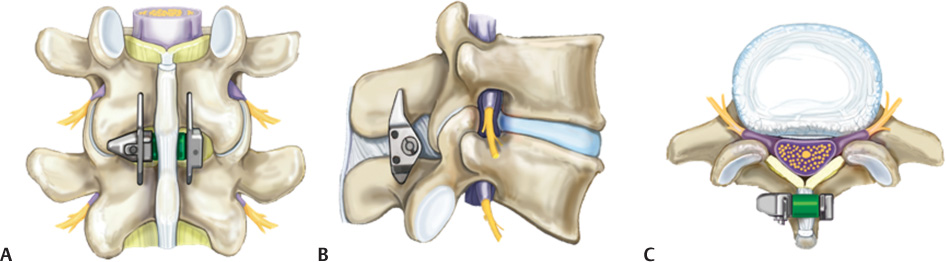
32 Neurogenic intermittent claudication is the most common and characteristic syndrome of lumbar spinal stenosis. Patients typically obtain relief from sitting and positions of flexion, and exacerbate the pain while standing or walking. The X STOP Interspinous Process Decompression (IPD) system (St. Francis Medical Technologies, Inc., Alameda, CA) is an interspinous spacer developed to treat patients with neurogenic intermittent claudication (Fig. 32–1). The implant limits extension of the stenotic levels of the lumbar spine by means of a spacer placed between the spinous processes. The procedure typically requires no general anesthesia and can be performed in under an hour. The X STOP is an alternative therapy to conservative treatment and decompressive surgery for patients suffering from lumbar spinal stenosis.1 The X STOP IPD system is indicated in patients whose symptoms are exacerbated in extension and relieved in flexion. Implanted between the spinous processes, the X STOP reduces extension at the symptomatic level and allows motion in flexion, axial rotation, and lateral bending.2 Figure 32–1 An image of the X STOP depicting the adjustable universal wing, tissue expander, fixed wing, and spacer. The tapered tissue expander allows for easier insertion between the spinous processes. The universal and fixed wings limit anterior and lateral migration. The spacer limits extension of the treated spinous processes. Although spinal stenosis had been observed in animals3–5 and found in Egyptian mummies, it was probably first described in 1803, by Portal of France, who observed that narrowed spinal canals were associated with leg pain and atrophy.6 Our understanding of this condition, however, really starts with Verbiest, who described the anatomical changes of hypertrophic articular processes causing spinal canal stenosis.7 Subsequently, Kirkaldy-Willis et al wrote about the three-joint complex and the pathological changes found in degenerative spinal stenosis.8 Degenerative processes may start in one-, two-, or three-joint complexes, including the disk anteriorly and the two facet joints posteriorly. With time, all three joints are involved. The degeneration of the joint also causes abnormal motion, which may produce osteophyte formation. Ultimately, disk protrusion or osteophyte formation, and hypertrophy of the facet joints and ligamentum flavum result in spinal stenosis. Medical literature regarding this condition became more available after the mid-1970s.9 The significant increase in the diagnosis of spinal stenosis is attributable to the introduction of axial imaging provided by computed tomographic (CT) and magnetic resonance imaging (MRI) scans. In the United States, lumbar spinal stenosis is the leading preoperative diagnosis for adults older than 65 who undergo spine surgery.10 In 1996, almost 90,000 surgeries were performed for lumbar spinal stenosis.10 Symptoms present with upright posture activity and include unilateral or bilateral radicular pain, sensation disturbance, and loss of strength in the lower extremities.7 Symptoms are typically relieved with flexion of the lumbar spine. The incidence of degenerative lumbar stenosis ranges from 1.7 to 8%.11 There does not appear to be gender predominance; however, degenerative spondylolisthesis associated with lumbar spinal stenosis is four times more common among women. Symptoms typically develop in the fifth or sixth decade of life in association with osteoarthritic changes in the lumbar spine. No known relationship exists between incidence of lumbar spinal stenosis and race. Spinal stenosis did not have the socioeconomic significance that we see today until the 1970s. The aging of our population is resulting in an increased incidence of degenerative stenosis. In 1900, the life expectancy was 45 years. People older than 65 constituted less than 4% of the population.12 The estimated life expectancy in 2026 is 86 years with 20% of the population expected to be older than 65 years of age. The U.S. Census Bureau projections estimate doubling of the population older than age 64 to 64 million by 2040. Symptoms of spinal stenosis may respond to nonoperative management. Conservative measures often begin with a period of rest as well as nonsteroidal anti-inflammatory drugs (NSAIDS), physical therapy, and, sometimes, oral steroids. In physical therapy, trunk stabilization and core muscle strengthening are typically the goals. Epidural steroid injection is often used as an adjunct, particularly in patients with unremitting radiculopathy and neurogenic claudication. There is no clear evidence of long-term efficacy of epidural steroids; however, they can give significant short-term relief and allow participation in physical therapy. Outcomes with nonoperative treatment reported by Hurri et al showed 44% of patients had at least some improvement in neurological symptoms.13 In other studies, Atlas et al found that 45% percent of patients had improvement in leg pain with nonoperative treatment, whereas Johnsson et al reported 32% of patients treated nonoperatively considered their condition improved.14,15 Operative treatment is indicated for patients with worsening pain that is resistant to conservative treatment. Patients with moderate to severe stenosis who do not improve with nonoperative interventions are likely to improve with surgical decompression. Historically, the literature supporting operative treatment has been shown to have methodological flaws with respect to indications for surgery and surgical outcome.16 However, in the last decade, prospective studies such as the Maine Lumbar Study have shown superior outcomes for operative treatment of symptomatic lumbar stenosis compared with nonoperative treatment.14 Surgical decompression, while offering the potential to improve the quality of life for individuals, also has the potential for significant complications, especially when a fusion is performed. Postoperative complications may include infection, epidural hematoma, instability, nonunion, instrumentation failure, and the need for future surgery due to the development of disease at adjacent levels. From a general medical perspective there is also a cardiac and respiratory risk, particularly in elderly patients undergoing procedures with extensive blood loss. The risk for postoperative infection remains significant despite the practice of antibiotic prophylaxis and strict sterile technique. In a study by Yuan et al 2 to 3% of patients undergoing lumbar decompression and arthrodesis with or without internal fixation suffered an infection.17 In this same study, the risk of nerve root injury from placement of pedicle screws was 0.4%. In addition to nerve root injury, dural tears are not uncommon during decompressive procedures. In a study by Wang et al, there was a 13.7% incidence of dural tears in 641 patients undergoing lumbar spine surgery, half of which were revisions.18 A meta-analysis of the literature performed by Turner et al in 1992 showed the following complication rates for neurogenic claudication surgery: perioperative mortality (0.32%), dural tears (5.91%), deep infection (1.08%), superficial infection (2.3%), deep venous thrombosis (2.78%), and any complication (12.64%).16 The X STOP was developed to fill the large void of treatment options between the safer yet less effective conservative care and the riskier but more effective surgical decompression. The X STOP was designed specifically to limit the terminal extension movement at only the individual level (s) that provoke symptoms, while allowing unrestricted movement of the remaining motion axes of the treated level (s). In addition, the implant was designed to be placed using a minimally invasive surgical technique with the patient under local anesthesia. Finally, it was designed to be placed without removing any bony or soft tissues, and removal is very straightforward should revision surgery become necessary. Several key design features allow for the straightforward implantation of the X STOP. The oval spacer separates the spinous processes and restricts extension at the implanted level (Fig. 32–2). The two lateral wings prevent the implant from migrating anteriorly or laterally, and the supraspinous ligament prevents the implant from migrating posteriorly. The tapered tissue expander facilitates lateral insertion while allowing the supraspinous ligament to be preserved. Biomechanical studies have shown that the X STOP significantly prevents narrowing of the spinal canal and neural foramina, limits extension, and reduces intradiskal pressure and facet loading.2,19–21 In an MRI cadaver study, Richards et al reported that X STOP placement increases the neural foramina area by 26% and the spinal canal area by 18% during extension.19 In addition, the foraminal width was increased by 41% and the subarticular canal diameter by 50% in extension.19 In a kinematics cadaver study, Lindsey et al reported that terminal extension at the implant level was reduced by 62% following X STOP placement, whereas lateral bending and axial rotation range of motion were unchanged.2 In a cadaveric disk pressure study, Swanson et al reported that the posterior annulus and nucleus pulposus pressures were reduced by 63% and 41%, respectively, during extension, and by 38% and 20%, respectively, in the neutral, standing position.20 Finally, Wiseman et al performed a cadaveric facet loading study and reported that the mean facet force during extension decreased by 68% during extension.21 In each of these studies, the adjacent level measurements were not significantly changed from the intact specimen state. These preclinical studies indicate that the X STOP increases spinal canal and neural foramina space and also produces signifi-cant unloading of the disk and facets. Figure 32–2 (A) Posterior, (B) lateral, and (C)
The X STOP Interspinous Process
Decompression System for
the Treatment of Lumbar
Neurogenic Claudication
 X STOP Design Rationale and Preclinical Confirmation
X STOP Design Rationale and Preclinical Confirmation
 The X STOP Multicenter Randomized Trial
The X STOP Multicenter Randomized Trial
Historical Perspective
Current Treatments
X STOP Design Rationale and Preclinical Confirmation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Historical Perspective
Historical Perspective Current Treatments
Current Treatments Operative Technique
Operative Technique Study Results
Study Results Discussion
Discussion Conclusion
Conclusion