Chapter 4 Primary Rhinoplasty
In this Chapter Online at experconsult.com
Online Contents
Preparation of the Nose Video 4.1
Making the Step Incision Animation 4.1
The Marginal Incision Video 4.5
Separating the Columella from the Medial Crura Video 4.6
Separating the Soft Tissues from the LLC Video 4.7
Elevating the Periosteum Video 4.8
Removing the Dorsal Hump with a Carbide Rasp Video 4.10a, b
Removing the Dorsal Hump Animation 4.2
Removing the Cephalic Margin of the LLC Video 4.11
Removing the Cephalic Margin of the LLC Animation 4.3
Separating the Mucoperichondrium from the Septal Cartilage Video 4.12
Fixing the Doyle Stents Video 4.15
Lateral Anteroposterior Percutaneous Osteotomy Video 4.17
Low-to-Low Osteotomy Animation 4.5
Applying Spreader Grafts Video 4.19
Applying Spreader Grafts Animation 4.6
Placing the Septal Rotation Suture Video 4.20
Placing the Septal Rotation Suture Animation 4.7
Placing the Columella Strut Animation 4.8
Use of a Tip Rotation Suture Animation 4.10
Reshaping and Repositioning the Footplates Video 4.22
Placing a Subdomal Graft Video 4.23
Placing a Subdomal Graft Animation 4.11
Harvesting an Onlay Tip Graft with the Tip Punch Animation 4.12
Harvesting a Tip Graft with the Shield Punch Animation 4.13
Placing a Supratip Suture and Repairing the Columellar Incision Video 4.24
Placing a Supratip Suture Animation 4.14
Placing an Alar Rim Graft Video 4.25
Placing an Alar Rim Graft Animation 4.15
Pearls
• The nose is initially injected with xylocaine containing 1 : 200 000 epinephrine and then 1 : 100 000 epinephrine after a few minutes to minimize the systemic reaction and maximize vasoconstriction.
• Preservation of the periosteum over the cephalic bony dorsum will protect the overlying muscles, provide a more natural shape to the nose and make minor residual nasal imperfections less discernible.
• When trimming the cephalic portion of the lower lateral cartilages, it is important to leave an equal amount of the cartilage behind rather than removing an equal amount since most lower lateral cartilages are asymmetric.
• If deepening the radix is part of the plan, it is often necessary to reduce the hump to facilitate deepening of the radix.
• The dorsal hump is removed using a combination of a bi-directional rasp for the bony hump and a knife for the cartilaginous hump after separation of the upper lateral cartilages.
• Before separation of the upper lateral cartilages, the soft tissue overlying the anterocaudal septum is removed.
• The sharp end of the septal elevator is used to separate the mucoperichondrium over the overlying dorsum to keep it intact.
• The upper lateral cartilages are separated from the dorsum if there is asymmetry or a large enough dorsal hump removal which can result in an open dorsal roof.
• A septoplasty is carried out using the anterior approach or an L-shape (Killian) incision.
• A septoplasty is performed leaving an L-shaped frame, at least 15 mm wide anteriorly and 10 mm wide caudally.
• Septal mucoperichondrial tears that are unilateral or bilateral, but not apposing, do not require any treatment.
• For opposing perforation of the septum, replacement of the septal cartilage or vomer bone will be sufficient without an attempt to repair to the laceration.
• Doyle or simple stents should be used after this type of septal perforation and left in place for at least a week.
• On patients with a longstanding deviation of the septum, the opposite inferior turbinate and occasionally the middle turbinates will become enlarged. This is usually ipsilateral to the external deviation of the nose.
• Only the hypertrophic portion of the inferior turbinate is removed with a pair of turbinate scissors, leaving behind an evenly shaped, normal sized turbinate. The raw surface of the turbinate is gently cauterized using suction cautery.
• A medial osteotomy is done using a 4 mm or 6 mm osteotome, complemented with a 2 mm percutaneous anteroposterior osteotomy and a lateral low-to-low osteotomy using a guarded osteotome.
• A wedge of bone is removed medially only if the nasal bones are too far apart.
• It is important to trim the upper lateral cartilages only after the septum and nasal bones have been repositioned, especially when there is an external nasal deviation.
• Spreader grafts are commonly used when a large dorsal hump is removed causing an open roof, or when there is a preexisting mid-vault narrowing and internal valve collapse.
• The upper lateral cartilages are approximated to the septum and spreader grafts using 5–0 PDS to avoid sinking posteriorly.
• When the anterior septum is deviated caudally, a septal rotation suture is used.
• A columella strut will be placed to elongate the columella and/or support the tip using septal cartilage, preferably, which is 3 mm wide with a variable length depending on the intended aesthetic goals.
• The tip cephalic rotation is achieved by removal of a triangular piece of caudal septum based anteriorly, a proportional amount of nasal lining and a tip rotation suture.
• The footplates are trimmed, if the subnasale is in an optimal position, or dissected and approximated (if the subnasale is retracted) using 5–0 PDS suture.
• If the domal arches are too wide, a transdomal suture is used.
• If the domal arches are ideally shaped but too far apart, then an interdomal or medial genu suture is used.
• If the domal arches are too close or are asymmetric, a subdomal graft is placed using a block of 1.5 mm × 1.5 mm cartilage approximately 10 mm long.
• If the infratip lobule is deficient causing an underprojected tip, a tip graft is applied.
• For patients who lack projection and in whom the infratip lobule does not extend caudally, a shield graft will be utilized.
• On patients who possess thick skin, a supratip stitch is placed.
• The columella incision is repaired using 6–0 fast absorbable catgut.
• A septal cartilage graft measuring 13–15 mm long and 2–3 mm wide is crafted from the thinnest portion of the septum and placed in the pocket as close to the alar rim as possible through an incision in the rim area.
• A combination of SteriStrips, Aquaplast, and metal splint are utilized to confine the soft tissues, limit swelling and create a proper nose definition.
• Doyle stents are removed in 4–8 days.
• The splint is kept in place for 7–8 days and removed after removal of the Doyle stents.
• Patients are instructed to avoid strenuous activities for 3 weeks and use of glasses for 5 weeks.
• Patients who do not have a history of acne will receive 10 mg of dexamethazone during surgery and a Medrol Dose Pack postoperatively.
• On patients who have supratip swelling, the nose is taped in the evening and through the night for 6 weeks.
The ultimate goal of any rhinoplasty is to have a pleasing nose that is harmonious with the rest of the face. Thus, a circumspect assessment of the entire face and analysis of the life-size photographs1 is crucial because imperfections of other parts of the face that have been missed can detract tremendously from a nose that would otherwise have an ideal configuration. It is the congruity of the nose with other facial structures that, regardless of the magnitude of the change in the nose, avoids the appearance of ‘surgical nose’. The other cardinal rule in achieving a desirable rhinoplasty outcome is to create an optimal balance between different segments of the nose itself. Each rhinoplasty step has to be logical and purposeful and must incorporate a full understanding of the dynamic changes that will ensue.
Operative Technique
The life-size photographs that have been analyzed using the soft tissue cephalometric principles described in Chapter 2 are hung from an IV pole next to the patient to be referred to during the surgery.1 The procedure is performed almost exclusively under general anesthesia in the author’s practice, unless a minor revision is planned. The nasal hair is trimmed using a pair of curved iris scissors and a piece of 0.5 inch (13 mm) adhesive tape wrapped around the end of a Q-tip is used to remove any hair particles (Video 4.1). The internal nose is cleansed and the face is prepped with Betadine solution and washed with saline solution.
Incision
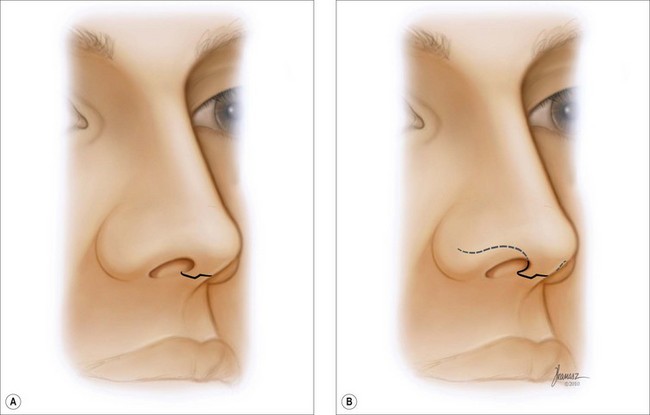
The incision is marked in the narrowest portion of the columella while the domes are pulled anteriorly using a blunt double hook. Before the incision is made, the skin hook is released to ensure that the incision is not too close to the nostrils. After allowing time for vasoconstriction, a step incision is made in the mid-columella and is continued along the caudal margin of the medial and lateral crura of the lower lateral cartilages (LLC) (Figure 4.1; Animation 4.1; Video 4.4). This incision provides the least visible scar and the best alignment of the wound margin at the time of repair.
Assessment of the Bleeding
At this point, nose bleeding is carefully evaluated. If it is deemed excessive, the blood pressure is measured by the anesthesiologist. If the systolic pressure is higher than 120 mmHg, it is reduced to this level by the anesthesiologist. In the absence of hypertension, excessive bleeding is commonly the consequence of either von Willebrand’s disease or consumption of aspirin or nonsteroidal anti-inflammatory drugs, either of which will often respond favorably to the infusion of 0.3 µg/kg of body weight of DDAVP (desmopressin) dissolved in 50 ml injectable saline and infused over 30–45 minutes.10
Deepening the Radix
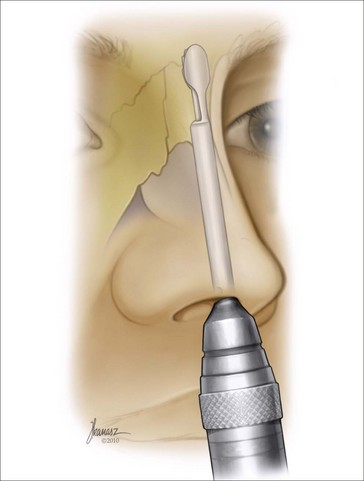
If the radix needs to be deepened after the periosteum is sufficiently elevated, a guarded burr will be used to achieve this (Figure 4.2; Video 4.9).2 While the burr is running, it is gently moved from side to side, not cephalocaudal, in order to avoid penetration of the frontal sinuses. The mid-portion of the burr is lined up with the upper tarsal crease. This is a very powerful tool and can produce sufficient deepening without too much effort. Additionally, the burr can generate significant heat, which can damage the soft tissues. It is therefore extremely important to lower the radix incrementally.
Removal of the Dorsal Hump
After the radix is deepened, the dorsal hump is eliminated. On patients with a large hump, it is often necessary to first remove a portion of the hump. Otherwise, one may face resistance in advancing the guarded burr in the desired site. In an ideal nasal frame, the nasion is deeper than the rest of the dorsum to accommodate the thicker soft tissues overlying this zone of the nose. The carbide push and pull rasp (Black & Black, Inc.) is then used to remove the bony hump. The rasp is activated in an oblique rather than a cephalocaudal direction, to minimize the potential for an inadvertent fracture of the septum. This is further minimized by placing the left index finger and thumb on either side of the nasal bones in such a way that, if the rasp slips, the digits will prevent it from damaging the septal frame (Figure 4.3; Animation 4.2; Video 4.10a). The rasping is done incrementally until the bony dorsum appears optimal and an adequate step is created between the bony and the remaining cartilaginous dorsum, indicating the magnitude of reduction in the dorsal hump (Video 4.10b). The cartilaginous dorsum is left alone at this point.
Removal of the Cephalic Margin of the Lower Lateral Cartilages
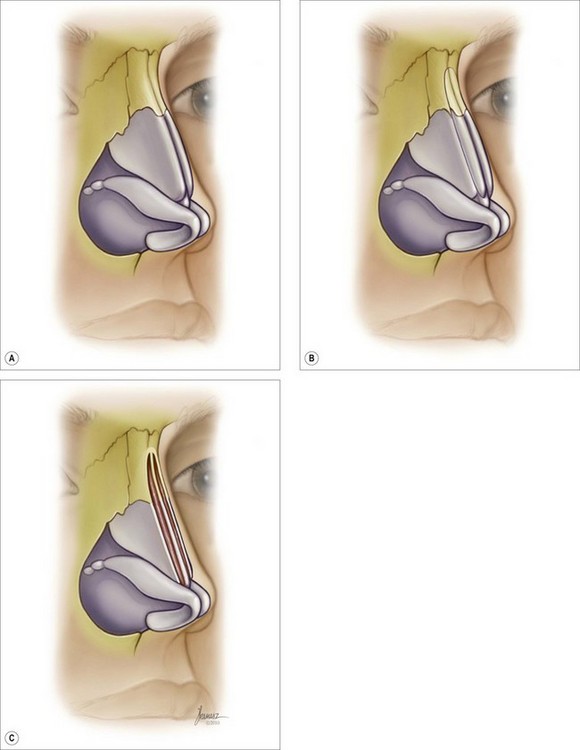
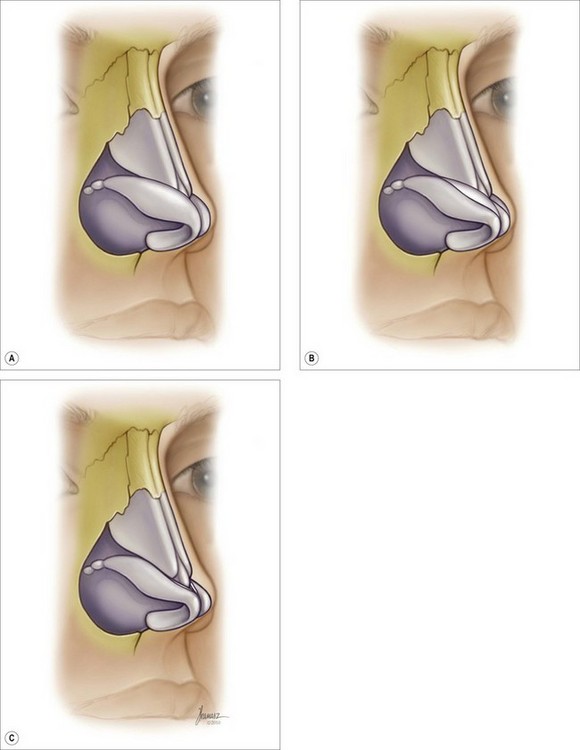
The Lateral Crus Stabilizer Black & Black Surgical, Inc. is then used to harness the LLC. Maintaining about 4–5 mm width of LLC anteriorly and 6 mm or more posteriorly, the excess portion of the cartilage is removed (Figure 4.4; Animation 4.3; Video 4.11).3 The incision in the cartilage is made with a no. 15 blade, and a pair of iris scissors is used to dissect and remove the excess cartilage. The mucoperichondrium is maintained intact, if possible. If the removed cartilage is thick and rigid enough it can be used as the alar rim graft. It is important to leave a symmetric amount of LLC in place since most of the time the LLCs are not symmetrical and, if one is focused on removing an equal amount of the LLCs, the remaining cartilages may not be symmetrical.