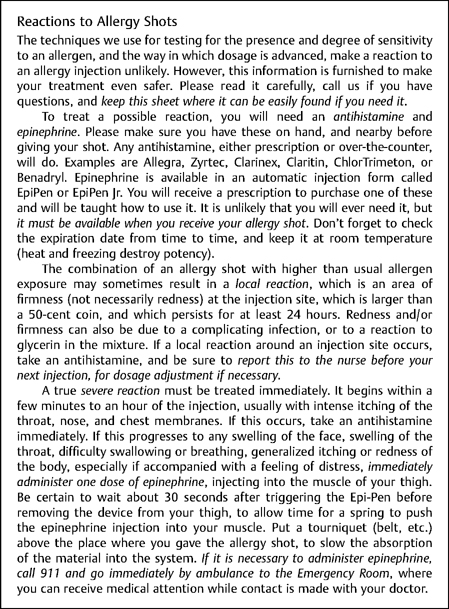
10 Note: Because emergency treatments often change, do not use this chapter as an inflexible treatment guide. Instead, use multiple reference sources to broaden and constantly update your knowledge. There are about 500 anaphylaxis deaths annually in the United States,1 and about one case per 3500 persons per year, with a fatality rate of 3%.2 Frequent causes are food, insect sting, drugs, and exercise.3,4 Fortunately, anaphylaxis rarely occurs during allergy management,5 with major systemic reactions occurring after only 0.005% of immunotherapy injections.6 This very low reaction rate is largely due to the safety of quantitative testing techniques7 such as intradermal titration (IDT),7 in vitro tests,8,9 the intracutaneous progressive dilution food test (IPDFT),10 and the use of immunotherapy based on these methods.11 It is more likely that anaphylaxis treatment knowledge will be used to treat acute asthma, food or drug reactions, and insect stings than reactions from allergy testing or treatment. Quick, positive action is needed to manage anaphylaxis. Pumphrey12 carefully investigated all fatal anaphylaxis cases in the United Kingdom from 1992 to 1999 to evaluate treatment details. He found that anaphylaxis deaths had been underreported, and that half the deaths were iatrogenic, with the rest about equally divided between food and insect stings. In most cases, food reactions caused asthma flares, resulting in respiratory arrest. Hypotensive shock was common with stings (in one half of cases) and iatrogenic anaphylaxis (in one third of cases). Previously unappreciated was how very rapidly anaphylaxis victims progress to respiratory or cardiac arrest. Median times to arrest were 30 minutes for foods, 15 minutes after stings, and only 5 minutes in iatrogenic situations. Excessive antigen exposure is the most common reason for anaphylaxis.11 This can arise from immunotherapy during peak pollen13 or mold14 seasons, or with any high allergen exposure.15 Overdoses also may arise from inexperience,16 error, skin testing an excessive number of antigens at one time, or by starting immunotherapy at too high a dose. The great advantage of quantitative testing methods is that accurate measurement of the patient’s degree of sensitivity to each allergen17 allows the preparation of a treatment mix and initiation of treatment, with a high degree of confidence that injections will not result in an overdose reaction.18 The use of glycerin preservative, refrigeration, and dated treatment vials help to reduce variations in potency, which may also be a source of error. During immunotherapy, excess antigen may be administered,6,14 by either too rapid an escalation or too frequent dosing.14 When immunotherapy is administered at home or in the office of a physician who is not specially trained in allergy, additional safety measures should be considered.6 Finally, errors in patient identification, dose calculations, diluting, mixing, or injecting may result in reactions. 6,19,20 These issues are thoroughly discussed in the immunotherapy safety study by Hurst et al.6 Cottonseed, flaxseed, castor bean, peanut, insect venoms, pollens in season (especially grass), and any allergen the patient suspects of causing previous reactions have a high risk,20 and testing with these antigens should be performed with caution. Screening tests at a high dilution, or the use of in vitro tests, is recommended before proceeding.21 Caution and a conservative approach are urged when dealing with highly sensitive patients,13,22 such as children,23 patients with a history of prior anaphylaxis,13 those taking a beta-blocking agent,22 and patients with uncontrolled asthma.6,15 A vial test is useful as a safety check before administering any allergy treatment mix.24 This initial skin test from the treatment vial (before starting dose escalation) must always be done when therapy is based on in vitro testing. Some physicians always use a vial test for the first dose from any vial. Some ailments resemble anaphylaxis.2,25,26 These include anxiety, flushing, hypoglycemia, arrhythmia, angina, myocardial infarction, transient ischemic attack, seizure, hereditary angioedema, airway obstruction, and acute pulmonary embolism. If any significant symptoms occur in the hours following antigen exposure (Fig. 10-1), prompt medical evaluation is recommended,27,28 to establish a diagnosis and render appropriate treatment. Most allergy-related reactions fall into three categories: vasovagal events, delayed allergic reactions, and immediate allergic reactions. Vasovagal events are common reactions that are not themselves dangerous but that must be quickly diagnosed to differentiate them from anaphylaxis. The predominant features of vasovagal attacks are pale skin, cold sweats, slow pulse, and normal blood pressure (BP) when recumbent. On the other hand, the features of anaphylaxis are usually opposite to those of a vasovagal event. The skin is red or flushed, warm, and dry, and there is a rapid pulse and a low recumbent BP. In addition, anaphylaxis patients often demonstrate itching or respiratory distress early in the reaction, but these are not seen during vasovagal events. Anxious patients can appear to have respiratory distress due to hyperventilation. Close examination of the skin is important, because over 90% of anaphylaxis patients develop skin urticaria, angioedema, or pruritus,29 and do not generally demonstrate diaphoresis. Cyanosis or pallor may develop later in anaphylaxis.1 Some vasovagal patients lose consciousness, experience seizures, or develop bradyarrhythmia, but these patients always recover rapidly when placed in a head-down position. The differential between anaphylaxis and a vasovagal event may be particularly difficult in patients who are taking beta-blockers, or patients with a large local or general allergic reaction and panic or anxiety. Table 10-1 compares the signs and symptoms of anaphylaxis and vasovagal events. Fig. 10-1 Sample patient handout.
Prevention and Management of Anaphylaxis
Bruce R. Gordon
♦ Time is Critical
♦ Prevention of Reactions
Diagnosis and Treatment
Potent Antigens
Sensitive Patients
In Vivo Safety Test (Vial Test)
♦ Diagnosis of Reactions
Nonallergic Events
Vasovagal Events
| Sign or Symptom | Vasovagal Event | Anaphylaxis |
| Pulse | Slow | Fast* |
| Blood pressure (recumbent) | Normal | Usually low |
| Feeling of impending doom | Absent | May be present |
| Itching, urticaria, or edema | Absent | Usually present |
| Skin color/temperature | Pale/cool | Red/warm** |
| Sweating | Present | Absent |
| Respiratory distress | Absent† | May be present |
| Cough or wheeze | Absent | May be present |
*May be slow with beta-blockade.
**Cyanosis or pallor may develop subsequently.
†May be tachypneic due to anxiety.
Anaphylactoid Reactions
Allergic mediators, or substances capable of releasing allergic mediators, may be released without actual allergen exposure, triggering anaphylaxis. This is called an anaphylactoid reaction. Common anaphylactoid triggers are scombroid fish poisoning, narcotics, vancomycin, anesthetics, muscle depolarizing drugs, hyperosmolar solutions, and radiologic contrast agents. Contrast agents cause about one anaphylactoid reaction for every 5000 exposures,25 whereas anaphylactoid reactions during general anesthesia occur in fromone in 6000 to one in 20,000 cases.30 Anaphylactoid reactions present in the same way, and are treated exactly like allergen-induced anaphylaxis.29
Delayed Allergic Reactions
Skin test or immunotherapy injection wheals may enlarge or reappear after 6 or more hours,31 and such delayed reactions may require a reduction in dosage. Delayed systemic reactions, usually in the form of worsening of preexisting allergic symptoms, also are possible. Delayed systemic reactions require both symptomatic treatment of the event and subsequent dose reduction. Unless asthma is provoked by these late reactions, emergency treatment is seldom necessary. However, especially in the case of reactions to food, in rare instances there may be a delay of up to 6 hours before symptoms worsen to a serious level.12
Immediate Allergic Reactions
There are four types of immediate reactions: local, large (severe) local, generalized (systemic), and anaphylaxis. These reactions differ in their degree of severity, and only anaphylaxis is life threatening. Reactions may occur within seconds, minutes, or up to several hours following antigen exposure.32 As already noted, iatrogenic cases (immunotherapy, skin tests, drugs, anesthesia) are likely to result in cardiopulmonary arrest within minutes.
Local Reactions
Local reactions are frequent normal events during allergy treatment, and are characterized by local itching, erythema, or swelling smaller than a half-dollar coin (3 cm) in diameter.
Large Local Reactions
These reactions vary from silver-dollar–sized (4 cm) indurated areas to swelling of the whole upper arm, and usually indicate an antigen overdose or strong contemporaneous environmental exposure. Successful immunotherapy need not include the production of large local reactions,33 and when these are encountered, they indicate a need to reduce the antigen dosage.
Generalized (Systemic) Reactions
These reactions may manifest themselves as exacerbation of preexisting allergic symptoms, bronchospasm, urticaria, or angioedema. These reactions correspond to grade I or II in the classification of Müller.34 They occur when the patient is already experiencing a high antigen exposure, and testing or treatment add sufficient antigen to exceed the symptomproducing threshold. Although generalized reactions usually do not progress to anaphylaxis, they do require symptomatic treatment and careful observation. Even if anaphylaxis does not occur, a general reaction may initiate a dangerous late-phase asthma flare within 6 to 8 hours.35
Anaphylaxis
True anaphylaxis, Müller grades III to IV, may begin like a generalized reaction, and then rapidly evolve to cardiopulmonary collapse. Early marked exacerbation of allergic symptoms, especially nasal, throat, and ocular itching, facial flushing, and throat tightness,36 are usually accompanied by tachycardia, a normally reliable sign of anaphylaxis.37 Tachycardia may not occur in patients receiving β-adrenergic blocking agents.38 Other common symptoms of anaphylaxis are wheezing, cough, urticaria, pruritus, angioedema, or a feeling of impending doom (“angor animi”). Less often, confusion, diarrhea, cramps, vomiting, and urinary urgency develop. Severe asthma, oral or laryngeal edema, hypotension, and arrhythmias may precede cardiovascular collapse. Most cases progress to respiratory obstruction or shock,38 with arrest occurring in as little as 1 minute, unless appropriate measures are rapidly undertaken.12
Biphasic Anaphylaxis
In general, the longer the delay from exposure to onset of anaphylaxis, the less severe the reaction. In two studies, the initial symptoms of anaphylaxis symptoms always occurred within 60 minutes of parenteral antigen exposure.35 However, because of slow absorption of antigens after oral exposure, anaphylaxis symptoms due to drugs or foods may not begin to occur until 6 hours after ingestion of the offending substance.12,39 At a median time of 8 hours after initial treatment, 5 to 20% of anaphylaxis patients may relapse into protracted late-phase reactions, including oral, laryngeal, or pulmonary edema, hemorrhage, shock, and severe asthma.39,40 These cases are initially indistinguishable from patients who do not relapse,41 and because of this possibility, after stabilization, one should always consider hospitalization for observation of patients experiencing anaphylaxis.38
♦ Being Prepared to Treat Anaphylaxis
Every allergy office, even one within a hospital, and each patient must be ready to handle the first minutes of anaphylaxis (Fig. 10-1). The physician’s responsibility is to make a proper diagnosis rapidly, initiate treatment, and then stabilize the patient for transport. The basic measures are administering epinephrine without delay, ensuring airway support, and instituting cardiopulmonary resuscitation (CPR). Epinephrine must be immediately available, either in commercial kits or prefilled syringes, and all personnel should be trained and authorized in its use. All anaphylaxis patients must be given intramuscular (IM) epinephrine as quickly as possible. Early use of epinephrine was the most critical survival factor in Pumphrey’s12 study, in which only 14% of patients who died from anaphylaxis had received epinephrine before cardiopulmonary arrest.
Second only to administration of epinephrine is the maintenance of an airway. This may require only the use of bronchodilators, but the office staff should be prepared to perform either intubation or tracheotomy, with administration of oxygen under pressure. Three quarters of anaphylaxis victims die from hypoxia due to airway edema or asthma.42 Thus, equipment and training for establishing an airway are paramount.
Third, because failure to institute CPR when needed is a recognized error,38 one must consider CPR training for all personnel. Physicians and nursing supervisors should consider obtaining advanced cardiac life support (ACLS) certification.27 One quarter of anaphylaxis fatalities occur from circulatory failure; therefore, rapid volume replacement, pressor support, and effective CPR are critical. Finally, how extensive other preparations must be depends on the practice’s geographic location. Rural practitioners, without nearby hospital facilities, may need to function at an advanced level. Readiness drills before anaphylaxis strikes are useful for evaluating readiness of supplies and personnel, and for maintaining familiarity with emergency plans.
♦ Drug Interactions Complicating Anaphylaxis
Beta-Blockers
Beta-adrenergic blockers43 affect anaphylaxis adversely in two ways. First, beta-blockade is proallergic, it and reduces the effectiveness of anaphylaxis therapy.44 In addition, beta-blockade, especially that produced by noncardioselective drugs, may cause a hypertensive crisis due to unopposed β-adrenergic effects of epinephrine.39 Beta-blockade increases the risk of reactions to radiocontrast material by about threefold,45 and it probably has similar effects on allergic anaphylaxis. Beta-1 selective beta-blockers are less likely to trigger asthma, but are otherwise still proallergic,43 as well as interfering with anaphylaxis treatment.
Tricyclic and Monoamine Oxidase (MAO) Inhibitor Antidepressants
Tricyclics block the reuptake of catecholamines.46 MAO inhibitors prevent degradation of catecholamines.7,47 In both cases, it is necessary to utilize reduced epinephrine or dopamine doses, and to closely monitor patients for the development of hypertension when such drugs are employed.
♦ Recommended Emergency Drugs and Supplies
The supplies that should be on hand to manage anaphylaxis depend on many factors, especially the distance of the office from hospital care. Several lists of recommended drugs and supplies have been published, 27,29,48,49 but these should be modified to suit the needs of each office, as follows:
- Monitoring equipment: Every office should have a sphygmomanometer and stethoscope. In addition, one may consider having on hand an oximeter, and an electrocardiograph (ECG)/defibrillator or an automated external defibrillator (AED). Early monitoring of pulse and BP is important in distinguishing a vasovagal reaction from true anaphylaxis. Once epinephrine is given, continuous monitoring of vital signs is critical.
- Epinephrine 1:1000 (1 mg/cc): This is the single most valuable drug in the management of anaphylaxis.37 It should be immediately available in the office, as well as in homes where it may be needed.3,50 At the first suspicion of anaphylaxis, administer epinephrine. A prolonged resuscitation effort or a fatal outcome is generally the result when epinephrine is not used early in the reaction.1,12,38 The Canadian Laboratory Centre for Disease Control states, “Failure to use epinephrine promptly is more dangerous than using it improperly,”51 and, according to the United Kingdom Resuscitation Council, “Epinephrine is greatly under-used. . .and, when given intramuscularly is very safe.”1 However, despite the critical role of epinephrine, it should be used carefully, because administration of too large a dose, or intravenous administration too rapidly or in too concentrated a form can be fatal.12,52
- Adult use: Prefilled 0.3-cc dual-dose syringes (Ana-Kit, Hollister–Stier, Spokane, Washington) or self-injecting 0.3- or 0.15-cc syringes (EpiPen, EpiPen Jr., Dey Laboratories, Napa, California) of epinephrine are recommended because they can be used quickly. The usual adult dose is 0.3 to 1.0 cc (0.3 to 1.0 mg) intramuscular (IM). The English consensus recommendation is to use 0.5 cc IM.1 IM use is always preferred because of more rapid action than with subcutaneous (SC) administration.1,51,53
- Pediatric use: The usual IM pediatric dose of epinephrine is 0.01 cc/kg (up to 0.3 to 0.5 cc maximum).53 To accurately measure the small doses required for infants, 1:1000 weight per volume (w/v) epinephrine should be diluted 1:10 before administration. Because of variable absorption in this age group,53 additional epinephrine may be required, although this will require careful monitoring. Epinephrine 1:1000 w/v can also be given intratracheally, 0.1 cc/kg.46
- Reduced doses: Older patients, especially those with arteriosclerosis or hypertension, may not tolerate the usual adult dose of epinephrine. In this group, it may be necessary to start at a dose of 0.2 cc.27
- Beta-blockers: Persons taking beta-blockers may require more epinephrine than usual to counter anaphylaxis, but giving multiple doses to these patients may also cause hypertension. Therefore, careful monitoring is needed in these situations.
- Inhaled epinephrine: Epinephrine can be administered by metered dose inhaler (over-the-counter brands) provided the patient is able to inspire deeply. Ten to 15 puffs in a child, or >20 puffs in an adult, produce blood epinephrine levels similar to those seen with recommended IM doses.3
- Repeated doses: In adults epinephrine is rapidly inactivated. A single dose is clinically effective for only about 3 to 5 minutes. Don’t hesitate to repeat epinephrine, with monitoring, every 3 to 5 minutes until the patient is clinically stable.1,46 In children, the half-life of epinephrine is about 40 minutes.53 It is necessary to monitor to determine the need for subsequent doses.
- Shock: In circulatory collapse, epinephrine (always diluted to 1:10,000 or 1:100,000) must be given centrally via intravenous (IV)54 or endotracheal routes.46 If no airway or IV access has been established, it may be given IM into the tongue, or via a transtracheal puncture. Epinephrine should be administered IV only to treat immediately life-threatening shock. The initial IV dose (children or adults) is 5 μg/kg,54 up to a maximum adult dose of 1 mg in 10 cc.46 Give half the calculated dose by slow IV push, then slowly give the remainder in small amounts while monitoring rhythm and BP. Monitoring is strongly suggested whenever IV epinephrine is used.1 British authorities prefer using 1:100,000 solutions, starting at 1 to 2 cc/minute.42 When treating shock, endotracheal or IM routes may require 2 to 2.5 times greater epinephrine doses than those employed for anaphylaxis alone. IV epinephrine must be used early for the treatment of shock, as animal data suggest that late use is ineffective.55
- Pediatric use: The usual IM pediatric dose of epinephrine is 0.01 cc/kg (up to 0.3 to 0.5 cc maximum).53 To accurately measure the small doses required for infants, 1:1000 weight per volume (w/v) epinephrine should be diluted 1:10 before administration. Because of variable absorption in this age group,53 additional epinephrine may be required, although this will require careful monitoring. Epinephrine 1:1000 w/v can also be given intratracheally, 0.1 cc/kg.46
- Adult use: Prefilled 0.3-cc dual-dose syringes (Ana-Kit, Hollister–Stier, Spokane, Washington) or self-injecting 0.3- or 0.15-cc syringes (EpiPen, EpiPen Jr., Dey Laboratories, Napa, California) of epinephrine are recommended because they can be used quickly. The usual adult dose is 0.3 to 1.0 cc (0.3 to 1.0 mg) intramuscular (IM). The English consensus recommendation is to use 0.5 cc IM.1 IM use is always preferred because of more rapid action than with subcutaneous (SC) administration.1,51,53
- Oxygen and ventilation support: Second only to epinephrine, oxygen is a key drug. Low-flow oxygen should be started during initial treatment. If shock develops, the patient is intubated, or CPR is started, then it becomes necessary to give 10 to 15 L/minute1 to maintain > 90% oxygen saturation. Oral edema or laryngeal edema may require cricothyrotomy or tracheotomy. The office where allergy injections are given should be able to support respiration with an Ambutype bag, masks, oral airways, a laryngoscope (with fresh batteries), endotracheal tubes, and cricothyrotomy instruments such as Nu-Trake and Pedia-Trake (Armstrong Medical Industries, Lincolnshire, Illinois), or tracheotomy instruments.
- Intravenous supplies: The largest possible IV catheter should be inserted as soon as possible (before shock causes vascular collapse). The office should have available IV catheters, syringes, needles, lidocaine, alcohol wipes, connecting tubing, IV fluids (several liters), tape, tourniquets, and an IV pole. Crystalloid solutions may not be effective in treating anaphylactic shock.38,42 Therefore, both types of IV solutions are recommended: normal saline or 5% dextrose (D5W), and 5% albumin, 5% plasma protein solution, or a dextran solution. If shock is present, give fluid first, before starting pressor agents, administering ~20 cc/kg of IV fluid as initial therapy in adults or children.1,54
- Suction and catheters: In anaphylaxis, thick secretions may make ventilation or intubation difficult or impossible. When setting up supplies, check that suction catheters fit into the endotracheal and cricothyrotomy tubes, and that suction will reach wherever it is needed, and is strong enough (greater than — 120 mm Hg).46
- Bronchodilators: An albuterol inhaler, or equivalent, should be available. Multiple inhalations may be required if the patient is beta-blockaded or has been using β-agonists regularly. Ipratropium (Atrovent) inhaler, or equivalent, may also be helpful, but requires 15 to 30 inhalations. Anticholinergics are not blocked by betablockers and are synergistic with inhaled β-agonists.56
- Dopamine: This drug is primarily β-adrenergic at doses below 10 μg/ kg/minute. Start treatment at 1 μg/kg/minute IV, and titrate up to a maximum of 20 μg/kg/minute to support BP. Reduce the initial dose to 0.1 μg/kg/minute if the patient is on MAO inhibitors.46 Dopamine must be diluted before IV administration.
- Phentolamine: This α-adrenergic blocker is used in 5- to 10-mg IV increments (for children, 1 mg) every 5 to 15 minutes, to control BP in a hypertensive crisis (e.g., beta-blockade).57
- Nitroglycerin: Stock sublingual 0.4-mg tablets. For angina, give one tablet under the tongue every 5 minutes, up to three doses, or until relief occurs.46
- Antihistamines: Treatment should include an H1 antihistamine, such as diphenhydramine 100 mg IV (child: 12.5 to 100 mg).51 Alternatively, one may give an oral (PO) antihistamine. Following this, slowly (over 5 minutes) give an H2 IV antihistamine,39 such as ranitidine 50 mg. Do not administer cimetidine because it interferes with the metabolism of many drugs, including beta-blockers.58 Both H1 and H2 agents are helpful, particularly in beta-blockaded patients,59 and in refractory anaphylaxis.42 Always give an H1 antihistamine before an H2 antihistamine, to prevent cardiac side effects.
- Corticosteroids: Steroids take up to 4 to 6 hours to work,42 but they act to shorten anaphylaxis and can prevent late reactions. An oral dose of 40 to 50 mg of prednisone may be given.38 For IV administration, slowly give dexamethasone 20 mg, or hydrocortisone 500 mg.1,42,60 If the patient is sulfite allergic, one may substitute IV methylprednisolone 40 mg, unless the patient has a known succinate ester allergy,36 or allergy to benzyl alcohol. In children, a minimum dose of 0.5 mg/ kg methylprednisolone may be given. Corticosteroids in some form should probably be given to every patient with a generalized or anaphylactic reaction,37 and they should always be administered if severe asthma is present.61 Because of the risk of preexisting suppression of endogenous cortisol, steroids should also be administered to patients who are already taking systemic corticosteroids or high-dose inhaled steroids.
- Heparin: In difficult cases of anaphylaxis, consider giving heparin. Heparin adsorbs and inactivates histamine and other allergic mediators,62,63 releases histaminase, which lowers histamine levels,64 improves the coagulopathy of anaphylaxis,65 and is antiinflammatory.66 Heparin ameliorates or prevents anaphylaxis in animal models,67 and it has been used successfully in small clinical trials of acute asthma.68,69 According to experienced clinicians, it is especially useful in beta-blockaded or refractory anaphylactic patients. The adult dose is 10,000 units IV, whereas the dose for children is 50 to 75 U/kg. The contraindications in the heparin package insert must be considered before it is used. Low molecular weight heparins have not been tested in anaphylaxis.
- Aspirin: For suspected coronary insufficiency, give 325 mg PO.
- Phentolamine: This α-adrenergic blocker is used in 5- to 10-mg IV increments (for children, 1 mg) every 5 to 15 minutes, to control BP in a hypertensive crisis (e.g., beta-blockade).57
♦ Anaphylaxis Treatment: Sample Protocol
- Cease administration of allergenic extracts.
- Assess symptoms, pulse, BP, respirations; evaluate skin color, temperature, and moisture.
- Quickly deduce type of reaction.
- Consult other clinicians within office.
- Always give IM epinephrine, as soon as anaphylaxis diagnosis is made.
- Confirm diagnosis; continue recording vital signs.
- Apply tourniquet proximal to allergen injection site.
- Assess reaction severity and review patient’s medical and medication history.
- Check peak flow, give albuterol inhaler, repeat if not effective.
- Lower patient’s head, loosen clothing.
- Call for help and notify supervisor physician. Call ambulance, if not already done.
- If severe hypotension (shock) occurs, give epinephrine 1:10,000 centrally, with monitoring.
- Request crash cart, defibrillator, suction machine, and oximeter.
- If continued bronchospasm, give ipratropium inhaler, repeat if not effective.
- Start 100% oxygen by mask. If oximeter available, keep O2 saturation > 90%.
- Assign duties; record personnel involved, patient symptoms, vital signs, and treatment given.
- Establish IV as soon as possible, start IV fluids.
- If patient beta-blocked, consider heparin IV; repeat epinephrine and monitor for hypertension.
- If angina occurs, give nitroglycerin. If no relief, give aspirin and start ACLS protocol.
- If no respirations, begin CPR, bag-mask, intubate, or perform a cricothyrotomy or tracheotomy.
- If no pulse noted, begin CPR, attach defibrillator or AED.
- Consider second dose of epinephrine; repeat at least every 3 to 5 minutes, with monitoring, in adults until satisfactory clinical improvement occurs. In children, monitoring is required to determine if subsequent doses are necessary.
- Check and loosen tourniquet every 5 minutes.
- Give IV or oral H1 antihistamine.
- Give IV (slowly) or oral H2 antihistamine (not cimetidine).
- Give IV (slowly) or oral corticosteroid.
- Reconsider heparin IV, for severe anaphylaxis.
- If hypotension noted, administer IV fluid, up to 1000 cc every 20 minutes and start second IV.
- If hypotension persists, mix and begin dopamine IV drip per package insert.
- If hypotension continues, administer IV colloid solution wide open.
- If hypertension occurs, turn off dopamine; if persistent, give phentolamine 5 to 10 mg IV, repeat every 5 minutes until BP normal.
- Transport via ambulance to hospital as soon as possible, communicate with emergency room physician, consider cardiology consult, encourage 24-hour observation.
- Postcode debriefing of personnel, completion of records, replenish supplies.
- Consider second dose of epinephrine; repeat at least every 3 to 5 minutes, with monitoring, in adults until satisfactory clinical improvement occurs. In children, monitoring is required to determine if subsequent doses are necessary.
♦ Conclusion
Acute anaphylaxis is a rare, potentially fatal, multisystem allergic reaction that every allergy office must be prepared to treat. Key points are (1) reaction prevention; (2) diagnosing the serious reaction; (3) proper staff training; and (4) keeping on hand, readily accessible, and in functioning condition, adequate supplies to provide emergency treatment appropriate to the office locale. Early administration of IM epinephrine is the most crucial step in managing anaphylaxis. The airway must be maintained, oxygen given, circulation supported, and further mediator effects blocked. Cardiopulmonary resuscitation is used whenever respiration or circulation is insufficient. Cardiac monitoring and the capability for defibrillation are helpful in the event of a severe reaction. Similarly, the ability to intubate or create a cricothyrotomy or tracheotomy may be life saving. Stabilized patients should be transported as soon as possible, preferably by ambulance with medical personnel in attendance. Because of the risk of delayed-onset reactions, and the possibility of multiorgan injury, anaphylaxis patients should be considered for admission to the hospital, and some authorities would make admission mandatory. Patients should be observed for a minimum of 8 hours,27,40,42 and appropriate specialist consultations should be arranged.
References
2. Heffner D. Anaphylaxis. Lippincotts Prim Care Pract 1997;1:220–223
3. Sampson HA. Fatal food-induced anaphylaxis. Allergy 1998;53(suppl 46): 125–130
8. Anon JB. Introduction to in vivo allergy testing. Otolaryngol Head Neck Surg 1993;109:593–600
9. Fadal RG. Experience with RAST-based immunotherapy. Otolaryngol Clin North Am 1992;25:43–60
16. Norman PS. Editorial: safety of allergen immunotherapy. J Allergy Clin Immunol 1989;84:438–439
19. King HC. An Otolaryngologist’s Guide to Allergy. New York: Thieme, 1990:175–177
22. Greineder DK. Risk management in allergen immunotherapy. J Allergy Clin Immunol 1996;98:S330–S334
24. King HC. An Otolaryngologist’s Guide to Allergy. NewYork: Thieme,1990:103
25. James JM. Anaphylaxis: multiple etiologies—focused therapy. J Ark Med Soc 1996;93:281–287
26. Wyatt R. Anaphylaxis. Postgrad Med 1996;100:87–99
28. Freeman TM. Anaphylaxis: diagnosis and treatment. Prim Care 1998;25:809–817
29. Kagy L, Blaiss MS. Anaphylaxis in children. Pediatr Ann 1998;27:727–734
38. Fisher MM, Baldo BA. Acute anaphylactic reactions. Med J Aust 1988;149: 34–38
39. Dykewicz MS. Anaphylaxis and stinging insect reactions. Compr Ther 1996; 22:579–585
49. Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Diagnosis and management of anaphylaxis: an updated practice parameter. J Allergy Clin Immunol 2005;115:S483–S523
56. Beakes DE. The use of anticholinergics in asthma. J Asthma 1997;34:357–368
57. Calhoun DA, Oparil S. Treatment of hypertensive crisis. N Engl J Med 1990; 323:1177–1183
62. Dolowitz DA, Dougherty TF. Allergy as inflammatory reactions. Ann Allergy 1971;29:410–417
66. Gervin AS. Complications of heparin therapy. Surg Gynecol Obstet 1975; 140:789–796
< div class='tao-gold-member'>