Fig. 7.1
(a) Arthroscopic visualization of failure and backout of previous bioscrew interference fixation of a tibialis anterior tendon allograft in the femoral socket. (b) Removal of this bioscrew was easily performed with an arthroscopic grasper demonstrating clear failure of fixation
Improper graft tensioning can also lead to ACL reconstruction failure. Under-tensioned grafts manifest in residual laxity after surgery, whereas over-tensioned grafts result in over-constraint of the joint and possible graft laxity over time. Ideal tensioning of the graft is complex and oftentimes clinically difficult to achieve. Factors that are important in tensioning include length of graft, the degree of tension applied, and the position of the knee at the time of tensioning [11, 19]. Graft type and graft fixation also play an important role in the success of reconstruction surgery. Grafts that are too small (e.g., some autologous hamstring tendons), or of poor quality, may lead to compromised results. Graft selection is an important step in successful ACL reconstruction and should be carefully considered in the preoperative stages. Prior history of severe patellar tendonitis or Osgood–Schlatter disease can compromise graft quality. Likewise, fixation failure due to bone block advancement (in the case of BTB) grafts), screw divergence, or loss of fixation with interference screws may negatively affect the intended outcome [11].
Biologic Failure
Infection after ACL reconstruction is relatively rare, with a rate of 0.58 % identified in one large retrospective series [20]. In that same series, hamstring autograft demonstrated a higher rate of infection (1.44 %) than BTB autograft (0.49 %) or allograft (0.44 %). Infection after ACL reconstruction presents a unique clinical problem and treatment options must be tailored to each patient. Successful outcomes after treatment of the infection with graft retention are possible; however, clinical results and motion are frequently negatively affected [21–24].
Stiffness after ACL reconstruction is often due to arthrofibrosis and usually affects extension more than flexion. There are several factors that have been associated with postoperative stiffness and arthrofibrosis including: early ACL reconstruction performed prior to restoration of complete range-of-motion after the initial ACL injury, excessive postoperative immobilization, Cyclops lesions, inappropriate graft tensioning, and non-anatomical graft placement [14, 25–27]
Another biologic cause of failed ACL reconstruction is poor graft incorporation. Patients with failed graft incorporation often present with clinical instability despite no history of trauma and no evidence of technical error [28]. Poor vascularity, failure of cellular repopulation of the graft, poor remodeling, and aberrant loads may all contribute to failed graft incorporation [12].
Mechanical Failure
The true incidence of traumatic failure after ACL reconstruction is not completely known and likely varies depending on the graft used [29, 30]. However, for the purposes of identifying etiologic causes it is useful to narrow traumatic failures to those that occur early (<6 months after surgery) and those that occur late (≥6 months after surgery). Early failures are often associated with aggressive physical therapy that overstresses the surgical fixation before incorporation has occurred [31]. Late failures are usually due to mechanisms similar to those involved in the initial ACL injury. It is believed that patients who have undergone well-performed ACL reconstructions with appropriate grafts are at no higher risk of re-rupturing the reconstructed ACL than the contralateral native ACL, though return to competitive sports and young age have been identified as potential risk factors [29, 32–34].
Unrecognized Concomitant Injury
A final category of causes of failed ACL reconstruction is unrecognized or untreated concomitant lesions of the knee such as meniscal injuries, articular cartilage wear (arthritis) or defects, posterolateral or posteromedial instability, and malalignment. All of these entities can negatively affect outcomes and potentially lead to failure. Needless to say, any revision procedure must address these problems prior to or during revision ACL reconstruction in order to optimize the chance at successful revision.
Patient Evaluation
History
As with all orthopedic conditions it is imperative that a careful history be performed. The nature of the symptoms and their onset (especially in relation to the index procedure) can provide significant clues to etiology. Frequently, the patient’s constellation of symptoms can be used to help identify whether the primary issue is pain, instability, or stiffness. Furthermore, the timing of these symptoms and signs in relation to the index procedure can help identify potential causes since failure that occurs within 6 months of the index procedure is often due to technical reasons and failure that occurs late may be caused by traumatic re-rupture, arthritic degeneration, or lack of graft incorporation.
Previous clinic notes, imaging studies, and intraoperative photographs may be helpful to better understand the clinical picture and should be reviewed, if possible. It is also useful to attempt to retrieve the index procedure operative report in order to identify the type of graft and hardware utilized and to understand how the tunnels were made (i.e., trans-tibial versus anteromedial portal, etc.).
The patient should be asked the circumstances behind the index procedure. How did the original injury occur? Was the index surgery delayed to allow motion recovery? Was there recurrent instability prior to surgery? Were there any postoperative wound healing issues? What postoperative rehabilitation was performed? At what time interval did they resume agility training, and when were they released for sports participation? What was the level of activity and overall knee performance after the index procedure? Did the patient return to sports? Was the return at the prior level of performance? Finally, it is important to discuss the patient’s desired level of activity and the expectations regarding possible surgical versus conservative management. Revision ACL reconstruction is a complex procedure and outcomes are less predictable than after primary reconstructions. Furthermore, rehabilitation after surgery can be more difficult. Patients should be counseled on all these factors and realistic expectations regarding operative and non-operative treatment should be clarified prior to making a final decision.
Physical Examination
Physical examination first begins with observation. Gait and lower extremity alignment should be carefully evaluated. Malalignment, excessive varus, or valgus with or without thrust may be indicative of a more complex structural problem that should be addressed prior to any revision ligament procedure. Inspection of scars can aid in preoperative planning and may suggest the type of graft used as well as the previous surgical approach. The integrity of the skin and overall muscle tone should also be reviewed. Thigh circumference should be compared with the contralateral limb in order to detect atrophy. Knee range-of-motion is evaluated, preferably with a goniometer, and evidence of stiffness should be recorded. Likewise, extensor mechanism dysfunction should be identified if present. Strength testing should also be performed.
A complete ligamentous exam including examination of the ACL, medial collateral ligament (MCL), lateral collateral ligament (LCL), PCL, as well as the posterolateral and posteromedial corners is necessary. ACL examination should include the Lachman, anterior drawer, and pivot shift tests. Varus and valgus testing at 0° and 30° should be performed to evaluate the collaterals. The posterior sag sign, posterior drawer, and the quadriceps active tests are used to evaluate the PCL. The Dial test or posterolateral spin test at 30° and 90° of knee flexion should be performed to test for posterolateral rotatory instability. The anterior drawer test with the tibia in external rotation can be used to test for increased anteromedial translation, a possible sign of posteromedial corner lesions.
Radiographic Evaluation
Plain radiographs including standing anteroposterior (AP) and lateral views as well as Merchant and Rosenberg [35] (45° posteroanterior (PA) weight-bearing) views are recommended. Standing AP and lateral views are used to inspect the femoral and tibial tunnel positions, hardware position, joint spaces, and overall alignment. The Rosenberg view is useful to evaluate the notch as well as the joint spaces in the medial and lateral compartments with the knee flexed [35]. A single standing hip-to-ankle alignment view may be used to draw out the mechanical axis from the center of the femoral head to the center of the talus to better evaluate lower extremity alignment. Any significant deviation from the mechanically neutral axis may require a concomitant or staged osteotomy. Plain radiographs that demonstrate osteolysis or bone defects should prompt further evaluation with a computed tomographic (CT) scan. CT scan is useful for more precisely evaluating the bone quality, architecture, tunnel position, and tunnel widening, which may require bone grafting as part of a staged procedure
MRI is often performed to review the integrity of the previous graft, the menisci, the articular surfaces, and the other ligaments and tendons about the knee. The degree and quality of signal in the graft is carefully evaluated, since increased signal may be indicative of graft impingement [36, 37]. MRI can also be used to look for loose bodies that are not visible on radiographs. Recent translation episodes may manifest in bone edema patterns that can also be seen on MRI.
Surgical Approach
Skin Incision
The data collected during a meticulous preoperative patient assessment and radiographic evaluation will aid in developing a preoperative plan and surgical approach. During the physical examination, careful inspection of the skin and myofascial envelope of the knee will help guide new skin incision placement. The positioning of the requisite skin incisions should include consideration of: (1) revascularization of dermal tissue, which is directly related to the time elapsed since previous surgical intervention, (2) potential incorporation of previous incisions without compromising surgical exposure, and (3) if new incisions are required for adequate exposure these should maximize skin bridges as bridges less than 7 cm may increase the risk of skin necrosis (Fig. 7.2) [37]. In this setting, the use of allograft tissue can reduce surgical dissection and thereby minimize the risk of wound complications. In the case of prior infection with poor quality or severely compromised soft tissues overlying the patella or tibia, plastic surgery consultation should be considered as a gastrocnemius flap may be required to prevent wound complications.


Fig. 7.2
(a) Skin necrosis and infection following BTB autograft required mobilization of a medial head gastrocnemius flap to facilitate soft tissue coverage. (b) Split-thickness skin grafting following flap placement resulted in effective coverage of the soft tissue defect
Tunnel Widening
Tunnel widening can cause a significantly increased degree of difficulty during ACL revision surgery due to complications secondary to bone loss and compromised fixation. While adverse clinical outcomes have been associated with tunnel widening, preoperative planning is critical to improve revision ACL reconstruction outcomes [38]. Femoral tunnel widening represents a specifically difficult problem due to impaired arthroscopic access, as compared to the superficially accessible tibial tunnel. Particular focus should be placed on preoperative radiographic evaluation of the previously placed tunnels. Plain radiography, CT, and MRI should be used to evaluate the dimensions of the tunnels (Fig. 7.3a–d). These dimensions can aid in selecting the preferred surgical option, including jumbo plug placement, divergent tunnel placement, stacking screws, matchstick or bullet grafting, or two-staged grafting and reconstruction (Fig. 7.3e–h) [38].


Fig. 7.3
(a) Anteroposterior (AP) and (b) lateral plain radiographs demonstrating tibial tunnel widening (c) Coronal and (d) sagittal CT images confirming and more accurately delineating tibial tunnel widening (approximately 18 mm). (e) AP and (f) lateral radiographs following removal of hardware and staged bone grafting of tibial and femoral tunnels. (g) Coronal and (h) sagittal CT images obtained demonstrating tibial tunnel graft fill and incorporation
Implanted Hardware
Recent advances in arthroscopic ACL reconstruction have resulted in a wide variety of fixation techniques. Specific hardware options range from aperture fixation with metallic and biologic interference screws to suspensory and double-cross pin fixation [39–41]. Knowledge of these various options is critical for the revision surgeon as removal or incorporation of the prior hardware may be necessary during the revision surgery. Many of these implants require specific removal instrumentation that should be available at the time of revision ACL reconstruction.
Optimal tunnel placement should not be compromised to avoid prior hardware. Removal of prior hardware should include meticulous excision of soft tissue and bone that may impede access to the hardware. Use of curettes, burrs, or small osteotomes may be required for adequate excision. If removal of a screw is required, care should be taken to confirm the correct screwdriver size and fully seat the screwdriver prior to removal (Fig. 7.4). A stripped metallic screw may be removed using an oversized screwdriver and direct impaction technique using a hand mallet, a reverse threaded screw removal instrument, or over-drilling with a coring reamer. Stripped biologic screw removal may be performed with direct drilling since metallic drills can effectively remove the softer, biologic screw. In these settings, removal of prior hardware may cause an additional increase in bone loss with subsequent tunnel widening. This situation should be considered prior to surgery and may result in the need for two-staged bone grafting and reconstruction. Removal of suspensory fixation is rare because these implants do not typically compromise new tunnel placement. Metallic staples may be removed with an implant-specific staple removal device or a small osteotome if necessary.
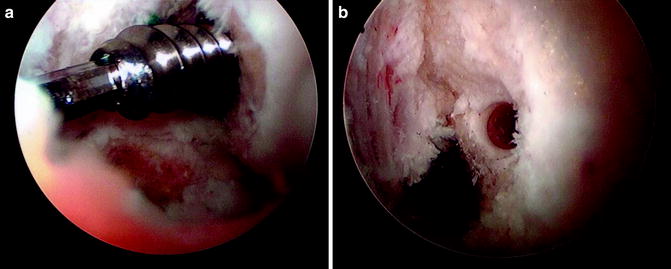
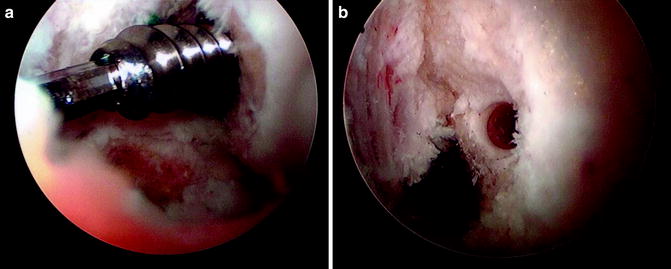
Fig. 7.4
(a) Traumatic rupture of previously well-positioned ACL graft may require removal of prior hardware prior to tunnel and socket drilling. Care should be taken to fully seat the appropriate screwdriver into the screw and thereby atraumatically remove the interfering hardware as shown in this arthoscopic image. A cannulated guide wire may also be used to ensure that the screw does not disengage and move freely within the knee joint. (b) Following complete hardware removal, the previous socket may be re-reamed in the absence of tunnel widening as in this case
In some cases, prior hardware does not compromise optimal revision tunnel placement and can be retained. Varying the trajectory of the femoral and tibial tunnels, while maintaining the optimal footprint position, can potentially avoid the need for hardware removal. The revising surgeon should be comfortable with multiple tunnel placement techniques including trans-tibial, anteromedial, two-incision drilling, and “all-inside” techniques (Fig. 7.5) [42]. In this setting, the retained hardware may serve to reduce potential bone loss and enable increased fixation as in the case of stacking screws [38].
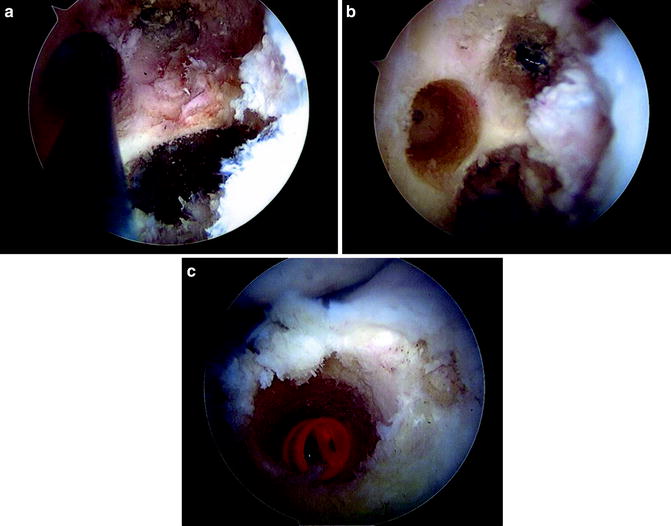
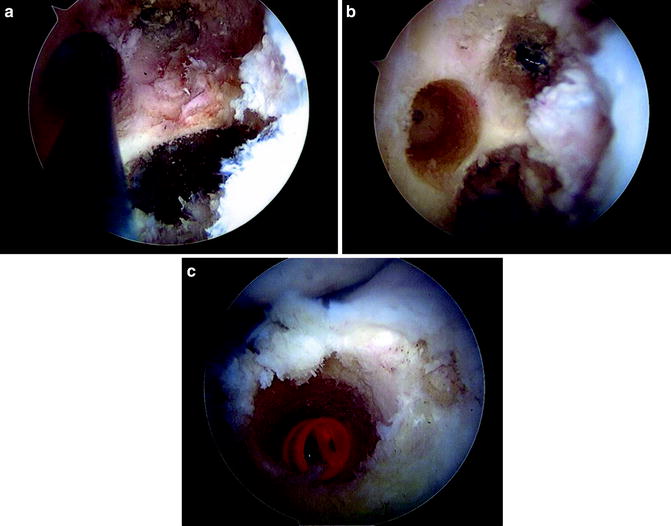
Fig. 7.5
(a) An anteromedial portal technique may be used to create a new revision femoral socket position without requiring hardware removal or bone grafting if the previous socket was not placed in the desired position as in this case. The guide wire can be seen arthroscopically placed in the new revision socket at the 10:30 position immediately below the previous vertical socket position. (b) Reaming of the femoral socket and guide wire removal demonstrates the new, divergent tunnel. (c) A prior well-placed tibial tunnel may be re-drilled following hardware removal and in the absence of excessive tunnel widening as in this arthroscopic image
Prosthetic Ligaments
Although synthetic ligaments are rarely used in ACL reconstruction surgery due to significantly increased failure rates, these ligaments may be encountered during revision ACL reconstruction [43




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








