Evidence-Based Practice to Improve Outcomes of Anterior Cruciate Ligament Reconstruction
Keywords
• Anterior cruciate ligament • Evidence-based medicine • Knee surgery • Expertise-based trails • Anatomic reconstruction • Narrative review
Key Points
Introduction
The earliest attempts to salvage the anterior cruciate ligament (ACL)-deficient knee were described by Battle in 1900 and Mayo Robson in 1903.1,2 In 1917, Groves was among the first to advocate reconstruction with graft tissue rather than primary repair.3 Many advances have taken place, and ACL surgery is among the most successful operations in orthopedic surgery. In the last 30 years, techniques in ACL reconstruction have evolved from open and extra-articular reconstruction techniques, to arthroscopic and more anatomic techniques. Considerable research has focused on graft selection, graft fixation, and tunnel placement.4 Modern techniques allow for minimal tissue trauma, accelerated recovery, and reproducible outcomes. For example, the use of an accessory medial portal for femoral tunnel drilling, based on an improved understanding of tunnel positioning, has led to an emphasis on anatomic ACL reconstruction.5
As described by Karlsson and colleagues,5 anatomic ACL reconstruction involves 4 key principles: the restoration of native insertion-site anatomy, the restoration of the 2 functional bundles of the native ACL, the restoration of native tensioning behavior between these 2 bundles, and the individualization of surgical techniques to each patient. However, anatomic ACL reconstruction is not synonymous with double-bundle ACL reconstruction. Just as the principles may be applied to single-bundle anatomic ACL reconstruction, they may likewise be discounted in nonanatomic double-bundle ACL reconstruction. A recent report has identified that while many studies have evaluated anatomic ACL reconstruction techniques, few provide enough surgical description to substantiate such claims.6
Whereas the immediate surgical goal of anatomic ACL reconstruction is to replicate native knee anatomy and biomechanical function, the long-term clinical goal is to stabilize the knee and minimize the development of symptomatic ACL-deficient degenerative arthrosis.5 Several cadaveric and in vivo kinematic studies have demonstrated improved biomechanical function and stability when anatomic ACL reconstruction techniques are compared with traditional nonanatomic techniques.7 Although early clinical results appear promising, long-term outcome data are lacking.8,9 Well-designed prospective studies with detailed technical descriptions and appropriate patient-centered outcomes will accurately investigate the benefits of this technique.
Evidence-based medicine (EBM) is the integration of best available research with clinical expertise and patient values to facilitate clinical decision making.10 Introduced by Sackett in the early 1980s and coined by Guyatt in the 1990s, both at McMaster University, EBM has been identified by the BMJ as one of the top 15 medical breakthroughs in the last 160 years.11,12
Diagnostic challenges: assessment of the ACL-deficient knee
Evidence for Clinical Maneuvers
Benjaminise and colleagues13 performed a meta-analysis of 28 studies to evaluate the accuracy of clinical tests for ACL tears. The included reports displayed some heterogeneity, but the Lachman test was identified as the most valid for ACL deficiency, with a pooled sensitivity of 85% and a pooled specificity of 94%. The pivot–shift test had a higher specificity, 98%, but a much lower sensitivity, 24%. The anterior drawer test had poor validity in acute tears, but good sensitivity and specificity in chronic cases. Despite these findings, preferential use of the Lachman test has been criticized due to its poor correlation with subjective and objective functional outcomes after ACL reconstruction surgery.14 Further, residual rotational laxity has been correlated with decreased patient satisfaction, functional instability, and the development of osteoarthritis.15–17
Role of the Pivot–Shift Test
Whereas reconstruction of the posterolateral bundle of the ACL during anatomic ACL reconstruction specifically aims to restore rotatory laxity, the pivot–shift test has received significant recent attention. Elimination of the pivot–shift phenomenon is a well-regarded goal of ACL reconstruction,18 and a recent systematic review identified an 85% correlation between reported pivot–shift test results and functional outcomes.19
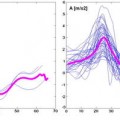
Nonetheless, performance and grading of the pivot–shift test remain subjective and poorly standardized. Applied forces and rotational moments, resulting tibial translation and tibial acceleration, and clinical grading all vary significantly between expert examiners.18 In a recent cadaveric study, Hoshino and colleagues20 demonstrated that standardization of the manual pivot–shift test might be possible. Variations in tibial acceleration were minimized after simple training, but the validity and reliability of this effect on clinical grading have not yet been investigated.
Other reports have described increasingly precise techniques to quantify the pathologic movements of the pivot–shift phenomenon. Noninvasive techniques include electromagnetic tracking of skin sensors, triaxial accelerometers, and digital image analysis.21 Even more precise, but also invasive, expensive, and complex, are intraoperative kinematic analysis with computer-assisted surgery, fixed electromagnetic tracking devices, fixed accelerometers, dynamic roentgen sterometric analysis (RSA), and open magnetic resonance imaging (MRI).22 Although these techniques demonstrate excellent promise, investigations of validity, reliability, and feasibility are required.
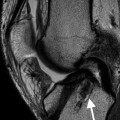
MRI continues to provide an important adjunct in the evaluation of ACL-deficient knees. Historical and recent reports have confirmed the high accuracy of conventional MRI in diagnosing ACL tears. Van Dyck and colleagues23 demonstrated accuracies of 97% and 95% for complete and partial ACL tears, respectively. MRI also identifies associated pathology, such as mensical injuries, that aid in preoperative planning.24
Surgical techniques: clinical studies and trial design
Expertise-Based Trials
Sackett and colleagues described that “Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients.”25 Importance is placed on high-quality research including well-designed randomized controlled trials (RCTs), rigorous systematic reviews, and meta-analyses. Due in part to some unique challenges when designing surgical RCTs, surgical decision making has long relied on nonsystematic clinical observations, expert opinion, and eminence-based decision-making.26
To conduct high-quality RCTs of surgical techniques, the following challenges must be overcome: a general lack of pre-existing EBM knowledge, difficulty with proper blinding, ethical considerations, and a tendency to defend historical procedures. Likewise, the effect of the learning curve effect, whereby seniority and experience often result in superior outcomes, must be considered.25 The latter can be overcome by well-designed expertise-based clinical trials.
Devereaux and colleagues26 describe differential expertise bias as being inherent to many RCTs of surgical procedures. A surgeon’s training and experience necessarily lead to the refinement of limited particular techniques to solve a given surgical problem. This creates restricted expertise. Subsequently, if surgeons with expertise in the novel intervention treat a majority of the patients in both treatment arms, and surgeons with expertise in the comparison intervention treat a minority of those in both arms, results could be biased toward the novel intervention. The inverse is also possible. Practically, the greater the disparity in distribution of expertise among the 2 groups, the greater risk of expertise bias to be present in a trial.
Many studies either fail to ensure or fail to report that the number of surgeons with expertise in each procedure is equal. Some studies stipulate surgeons complete a requisite number of cases with the novel procedure before entering the study, but bias may persist, because outcomes often continue to improve with extensive experience.26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree