(1)
Department of Dermatology, Drexel University, Philadelphia, Pennsylvania, USA
Abstract
Two major physiological events in eczema include transepidermal water loss owing to the loss of the stratum corneum, and occlusion of the sweat ducts, which leads to decreased sweat on the skin surface. Sulzberger noted occluded sweat ducts in atopic eczema in 1947. The observations that people with atopy do not sweat normally and that they will then suffer the effects of heat prostration combine with the clinical observation (and patient historical data) that sweating makes eczema worse. We propose that atopic dermatitis results from subclinical miliaria, which involves occlusion of sweat ducts. The difference in miliaria and eczema is found within the genetic part of the double-hit phenomenon. Once a patient begins scratching a genetically deficient stratum corneum, the disease process becomes ongoing.
Keywords
Atopic dermatitisAtopyDouble-hit hypothesisEczemaMiliariaOccluded sweat ductsPruritus Staphylococcus epidermidis Stratum corneumTransepidermal water lossThere are perhaps two major physiological events that occur in eczema. One is transepidermal water loss (TEWL), which is a constant phenomenon in acute and in most subacute eczema [1]. The loss of the stratum corneum is the major contributing factor in TEWL, and when the condition improves and the stratum corneum becomes reestablished, TEWL diminishes to baseline levels [2]. The TEWL gets contributions from the genetic disorders affecting the stratum corneum that have been mentioned previously and from the extensive scratching, which rips hundreds of crevices in the skin. This, however, is not the heretical part of the story.
The other event is the occlusion of the sweat ducts, which leads to decreased sweat on the skin surface. This is also the heretical finding, which is also the “oldest new finding” in this disease. As mentioned many times in this treatise, Sulzberger noted the occluded sweat ducts in atopic eczema (Fig. 6.1) and in seborrheic eczema (Figs. 3.9 and 6.2; miliaria, the known disease with eccrine duct occlusion).
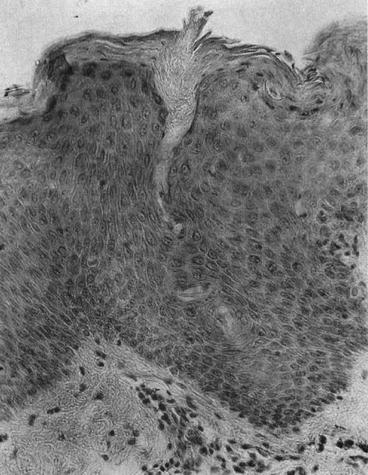

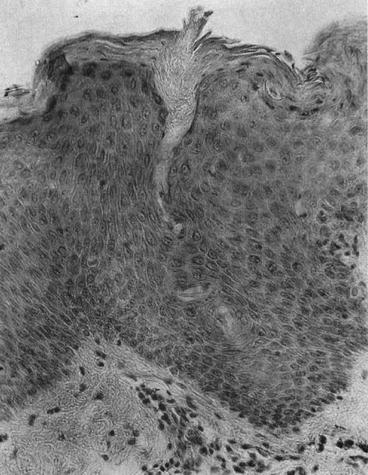
Fig. 6.1
Sulzberger’s observations from 1947. Occlusion is noted in the outer portion of the eccrine sweat duct in a patient with eczema (From Sulzberger et al. [1]; with permission)

Fig. 6.2
Hospitalized patient with miliaria rubra. The photomicrograph in Fig. 3.9 shows the same patient’s occluded sweat ducts
Sulzberger also made observations on the pH of the fluid in the vesicles in the acute disease. This fluid pH was much lower than serum or interstitial fluid and was consistent with the pH of sweat. With the low pH of the vesicular fluid, the observed ductal occlusion, and the fact that patients with atopic dermatitis had faulty sweating, Sulzberger believed the occluded sweat ducts played a large role in eczema [3]. We believe the very same.
Vesicle Fluid from Eczema Was Measured by Sulzberger
Eczema fluid showed lower pH than …
Fluid from inflammation (serum).
Sulzberger postulated—we believe correctly—that the fluid was from an occluded sweat duct.
The tropical anhidrosis Sulzberger was investigating is another feature in our story [4]. My former clinical practice partner, Dr. Philip LoPresti, was in the Army National Guard and was responsible for 400 National Guardsmen on their summer maneuvers at Fort Drum. He noted that the men who had atopic dermatitis would not sweat appropriately and would be subject to heat retention that would lead to heat prostration with core temperatures above 104 °F. The guardsmen who had atopy would be totally ineffective inside the Army tanks where the temperature was often 125 °F in the New York summers. (This was prior to air conditioning in the tanks of today.) He would consequently reassign all the guardsmen with atopy to different jobs that did not expose them to such high ambient temperatures.
Thus, the observations that people with atopy did not sweat normally and that they would then suffer the effects of heat prostration were combined with the clinical observation (and patient historical data) that sweating made eczema worse. Sweating in fact is one of the minor determinants of atopic dermatitis noted by Hanifin and Rajka [5]. The major determinants are pruritus, typical morphology and distribution, chronic or chronically relapsing dermatitis, and personal or family history of atopy. The minor determinants include xerosis; ichthyosis; palmar hyperlinearity; keratosis pilaris; hand or foot dermatitis; cheilitis; nipple eczema; susceptibility to bacterial, viral, or fungal infections; erythroderma; follicular accentuation; food intolerance; pruritus with sweating; intolerance of wool; and white dermographism, among others (Table 6.1).
Table 6.1
Major and minor features of atopic dermatitis
Major features | |
Pruritus | Chronic or chronically relapsing course |
Typical morphology and distribution | Personal or family history of atopy |









