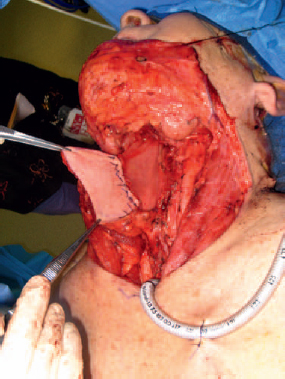
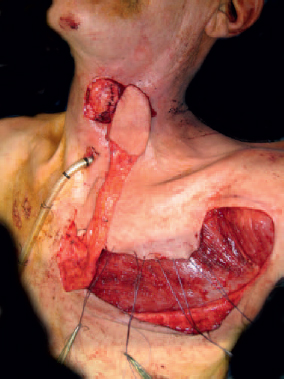
5 The upper aerodigestive tract is a complex organ responsible for deglutition, respiration, and communication. Cancers and disease of this organ often impact these functions and are detrimental to a patient’s quality of life. The primary goal of the head and neck reconstructive surgeon is to obtain a safe and stable wound, but it is imperative during reconstruction that the surgeon account for these issues to have a successful functional outcome. In the era of increasing primary chemoradiation for many tumors, wound complications for salvage surgery and reconstruction have become routine. Understanding the functional principles of defects and the potential reconstructive options is necessary to obtain a safe wound, reduce complications, and improve the quality of life. Wound breakdown and infections often result in pharyngocutaneous fistula and potential great vessel rupture. The incidence of pharyngocutaneous fistula is up to 75% for salvage surgery within 3 months of completing chemoradiation.1 Fistulas for patients who have been treated with radiation occur in 25 to 30%.2 The incidence of carotid blowout syndrome is between 3 and 4% of all head and neck cases, with increasing occurrences in patients who have had preoperative radiotherapy.3 To reduce the incidence of morbidity related to these wounds complications, reconstructive surgeons use vascularized tissue via regional or free flaps. Vascularized flaps have the advantage of providing supplemental tissue to restore some function to the organ. In the setting of postradiation wounds, both regional and free flaps bring tissue from outside the radiation fields. This has been shown to significantly reduce the incidence of major wound complications but not the incidence of fistula.4 The Montgomery salivary bypass tube is a plastic conduit inserted at the time of reconstruction or after fistula development to reduce and prevent salivary flow over or through the suture line. It has been shown to significantly reduce the incidence of strictures, major wound complications, and length of stay in the hospital, but not the incidence of fistula.5 Optimal nutrition and metabolism are critical factors to account for to obtain a successful outcome. Nutrition is often difficult to optimize in the head and neck cancer patient, but it is a factor we often overlook. Hypoalbuminemia, anemia, and weight loss 6 months prior to surgery have been found to be independent predictors of wound complication in laryngectomy patients.6 Additionally, proper thyroid function or supplementation is imperative. Hypothyroidism is well known to increase wound complications and is common in the head and neck cancer patient, with an incidence up to 48%.7 Supplementation of exogenous thyroid hormone hastens wound healing; thus, preoperative assessment of thyroid function is necessary in the postradiation patient.8 The pharynx and cervical esophagus are fundamentally essential structures to swallowing, speaking, and respiration. The pharynx extends from the cranial base to the level of the cricoid cartilage and is subdivided into the nasopharynx, oropharynx, and hypopharynx. The hypopharynx is contiguous with cervical esophagus. The pharynx is encompassed by horizontal muscle fibers of the superior, middle, and inferior constrictors, which are responsible for the contraction of the tubular organ and propulsion of the food bolus into the upper esophagus. Elevation of the pharynx and larynx via the vertically oriented stylopharyngeus, palatopharyngeus, and salpingopharyngeus muscles leads to improved movement of the bolus into the esophagus and protection of the larynx. The inferior constrictor and cricopharyngeus muscles act as a sphincter to prevent the entrance of air into the esophagus. This is a complex coordinated reflex that is often impaired in head and neck patients. Reconstructive goals of pharyngeal and esophageal defects center on restoration of an oral diet, respiration, and communication. Integral to these goals is the basic concept of replacing missing tissue with similar tissue. Local, regional, or free flaps are better suited for reconstruction if they emulate the structure to be replaced. Most of the pharynx and esophagus is thin, mobile, and pliable, and thus reconstructive tissue should be similarly modeled. Thick bulky local, regional, or free tissue flaps should be avoided if possible. Healing by secondary intention or direct closure often leads to superb results if chosen in the right defects. Skin grafts can be appropriate if the proper vascular bed is available. Local flaps are advantageous, as similar tissue is brought into the field. The most versatile tissue is from microvascular free flaps. Proper planning and tissue choice are absolutely necessary to obtain a safe and functional outcome. We have divided defects of the pharynx and esophagus into categories that facilitate a systematic approach to reconstruction. Each category has unique characteristics to consider during reconstruction. The lateral pharyngeal defect involves the pharynx superior to the hypopharynx and posterior to the soft palate. The posterior pharyngeal wall is at the same level but lies between the two lateral pharyngeal walls. It is the least mobile of all the structures. Contrasting with the posterior pharyngeal wall defect is the soft palate, which is the most mobile and sensitive structure. Velopharyngeal incompetence is a devastating consequence of scarring and inadequate reconstruction of the soft palate, affecting swallowing and communication. The cervical esophagus extends from just inferior to the postcricoid region to the thoracic inlet. Defects are subdivided into partial and circumferential and are treated in vastly different ways. Laryngopharyngeal and hypopharyngeal defects differ in terms of the presence or absence of the larynx. The combination defect, which includes a large portion of the trachea, laryngopharynx, and potentially the esophagus, is a challenging reconstructive problem that requires involvement of our thoracic colleagues. The lateral pharyngeal defect often involves the mucosa and underlying superior constrictor. Restoration of movement is the ultimate goal but can only be obtained if the muscle is not involved or if free edges can be realigned via primary closure. Healing by secondary intention is appropriate if the defect is small and does not include a through-and-through defect into the neck, as in transoral laser microsurgery. Care should be taken in this treatment decision, as secondary healing often leads to contraction and scarring. If excessive scarring occurs near or at the soft palate or glossotonsillar sulcus, velopharyngeal insufficiency or tongue tethering, respectively, can result. In these cases, alternate reconstruction should be chosen. If scarring encroaches on the soft palate, the reconstructive surgeon should have a low threshold for performing some level of palate reconstruction, as outlined in this chapter. If the defect is large and involves the glossotonsillar sulcus, consider free tissue transfer instead of primary closure or healing by secondary intention. If the defect is small (<2–3 cm) and does not involve the soft palate or glossotonsillar sulcus, primary closure can be adequate for a successful reconstruction. Careful layered closure including mucosa and muscle should be performed with Vicryl or similar suture. If the defect communicates with a neck dissection or involves exposed great vessels, it is imperative to ensure a watertight seal and reinforce it with tissue. Rotating vascularized tissue such as digastric or stylohyoid muscle is advantageous but sometimes not possible. A dermal graft works well to reinforce the suture line and provide one more layer of protection over the vessels. If the defect is greater than 3 cm, primary closure can alter the anatomy too much and lead to swallowing impairment and aspiration. A local, regional, or free tissue transfer should be considered in the case. Regional flaps such as the pectoralis myocutaneous (PM), lateral island trapezius, deltopectoral flap, submental island flap, and latissimus myocutaneous flaps are options to be considered in lateral pharyngeal wall defects (Fig. 5.1, Fig. 5.2, Fig. 5.3, and Fig. 5.4). The limitation of these flaps is the bulky nature of the myocutaneous paddles and the reduced pliability, which is essential for reconstruction of this area. However, in vessel-depleted necks, these flaps can serve as good alternatives to free flaps. If great vessel exposure is a problem, these regional flaps can provide excellent coverage of the carotid artery and jugular vein. ♦ Place a feeding tube prior to reconstruction if a gastrostomy tube is not already present. ♦ The cutaneous paddle of the regional flap should be designed as distal as possible but still over the muscle. Do not raise any portion of the skin paddle that is not over the muscle, as the blood supply is less reliable. ♦ For the PM flap, make sure the tunnel over the clavicle and into the pharynx is wide enough to accommodate the pedicle (Fig. 5.2). ♦ The latissimus flap should be passed through a generous tunnel between the pectoralis major and pectoralis minor into the neck. Once it has been passed, check to make sure the vascular pedicle has a gentle curvature and is not kinked. ♦ If the patient had a previous neck dissection or if there is variable vascular anatomy, the trapezius flap may not be available. The transverse cervical vessels need to be intact for this regional flap to work. The lateral island trapezius flap has a significant abort rate of up to 30% in one series9. Latissimus flap patients should have their arm in a sling immediately after surgery for at least 5 days to prevent compression of the pedicle. We allow a minimum of 5 to 7 days prior to initiation of oral feeding under the care and guidance of a speech pathologist. Once the patient reaches adequate oral intake to maintain nutrition and there is no evidence of a leak, we pull the nasogastric tube. The RFFF is a versatile reconstructive tool. It is thin and pliable and can be used to reconstruct multiple compartments of the pharynx and soft palate. Unless the patient is obese, this flap lacks a significant amount of fat and bulk. Bulk is important with significant defects of the base of tongue. If >50% of the base of tongue is missing along with the pharyngeal defect, we prefer to use a flap with more bulk. The lateral arm typically has more fat than the forearm, and we tend to use this in cases where a good portion of the base of tongue is missing. If the lateral arm is not available, the brachial fat pad or surrounding fat can be harvested with the RFFF and used to provide bulk to the base of tongue segment. ♦ The forearm can be harvested from either arm if the Allen’s test is appropriate bilaterally. We tend to choose the nondominant arm. ♦ Once the defect is defined, a template of the defect should be made. This assists with aligning the vessels appropriately, ensuring good geometry, and capturing the cephalic vein. The template is transposed to the forearm and the flap planned and harvested in standard fashion. This is particularly useful if different compartments need to be reconstructed. ♦ If the base of tongue segment needs more bulk, fat can be harvested adjacent to the cutaneous paddle and folded underneath that portion of the flap as we did in this case. ♦ Following the harvest, the flap is transferred into the defect and sutured with interrupted 3-0 Vicryl to form a watertight seal. The lateral arm free flap is particularly useful in reconstructing the pharynx if there is a significant base-of-tongue defect (>50%). It is a favorable donor site with little morbidity associated with it. Distal extension of the flap provides thinner tissue than the proximal flap. The pedicle length is more limited than the forearm flap but can be extended by designing the flap more distally and tracing the pedicle up the spiral groove. The profunda brachii artery can be used to lengthen the pedicle as the anterior radial collateral artery is typically ligated. The profunda has a caliber of 1.75 to 2.7 mm high in the spiral groove of the radius.10 ♦ Once the defect is defined, appropriate recipient vessels should be obtained because the limitation of this flap is often pedicle length. We tend to favor the occipital artery or facial artery for this flap. The occipital often is a similar match in caliber. If length will allow, the superior thyroid artery may serve as a good donor vessel. ♦ Take only as much skin (approximately one third of the arm) as can close primarily. It is generally 6 to 8 cm wide. A pinch test of the skin once the patient is asleep is a good measure of the quantity that can be harvested. If it can’t be closed primarily, a skin graft is necessary, but we tend to avoid this. ♦ If the patient has a significant amount of adipose tissue, the flap can be designed distally to capture thinner skin and subcutaneous tissue. Some groups have harvested tissue as far as 10 cm distal to the lateral epicondyle.11 ♦ For defect of the lateral pharynx with significant base of tongue involvement, we use the proximal portion of the flap for the base-of-tongue defect and the thinner distal portion for the glossotonsillar sulcus and lateral pharynx. Fig. 5.7 Lateral arm design with extension (dashed line) if thinner tissue needed for reconstruction. +, lateral epicondyle; arrow, deltoid insertion; BOT, base of tongue; PH, pharynx including tonsillar fossa and pillars. Composite defects that include the mandible, pharynx, soft palate, floor of mouth, and/or part of the tongue are best reconstructed with an osteocutaneous fibular free flap. Large, thin, pliable cutaneous paddles can be obtained to reconstruct these defects. There is a large bone stock and vascular pedicle. It is difficult for the flap to provide sufficient bulk for glossectomy defects, and it does not provide good-quality combined internal and external lining. Both of these limitations are solved by using a scapular osteocutaneous free flap. ♦ Obtain a computed tomography (CT) angiogram or a magnetic resonance angiogram (MRA) to assess the vasculature for a three-vessel run-off to the foot. This aids in the selection of the leg to use or in deciding if this flap should be abandoned altogether. This flap should be aborted if a congenital anomaly exists or if peripheral vascular disease has compromised the anterior or posterior tibial arteries. ♦ Once the defect is defined, perforators are mapped out on the leg and the cutaneous paddle designed in standard fashion. ♦ We typically prefer the contralateral leg. The pedicle comes off the back. If the ipsilateral leg is use, the pedicle exits from the front. Following reconstruction of the lateral pharynx, we place a nasogastric feeding tube if a gastrostomy tube is not already present. We allow a minimum of 5 to 7 days prior to initiation of oral feeding under the care and guidance of speech pathology. Once the patient reaches adequate oral intake to maintain nutrition and there is no evidence of a leak, we pull the nasogastric tube. If there is concern about a leak, we obtain a swallow study to document the location and quality of the leak and resume nil per os (NPO) status. The isolated posterior pharyngeal wall defect is uncommon but when present can be a difficult reconstructive challenge. Access to this area for reconstruction is typically via the neck, but occasionally the approach is transoral. An important aspect of the posterior pharyngeal wall defect is whether or not the spine is involved. Frequently the prevertebral fascia is intact, but in spine cases or when bone has been resected, care should be taken to ensure separating the pharyngeal tract from the spine. This is imperative, as the patient is at risk for cerebrospinal fluid (CSF) leaks, osteomyelitis, and epidural infections, which can be devastating. Small defects that include mucosa and muscle but have no connection to the neck often heal by secondary intention. Good oropharyngeal hygiene should be maintained throughout this process. If the prevertebral fascia is intact and the defect is limited to 2 to 3 cm, the mucosa and muscle can be dissected and mobilized. If the edges are able to be approximated with little tension, primary closure is suitable. The muscle should be closed in interrupted fashion with Vicryl or similar suture. The mucosa should then be closed as well with Vicryl sutures. We prefer 3.0 Vicryl for our closures. If the defect is too large for the edges to be mobilized and closed primarily, healing by secondary intention or skin graft is a powerful tool. As long as the bed to host the graft or healing by secondary intention is vascular and can support the process, this is an appropriate choice. ♦ The remnant edges should be tacked down to the prevertebral fascia to create a watertight seal and barrier from the neck. ♦ We tend to prefer healing by secondary intention, but a split-thickness graft can be harvested and tacked into place. The graft should be quilted and fixed into place in multiple locations. A bolster is not feasible. ♦ The preferred option is to allow the area to heal by secondary intention after the remnant edges are fixed down to the fascia with interrupted Vicryl sutures to form a watertight seal. Circumstances arise, particularly in spine surgery, when a free flap is needed to reconstruct the vertebral column. If spinal hardware becomes exposed to the pharyngeal compartment, there is not much choice but to remove the hardware. Unfortunately, this may lead to spinal instability, and thus the spinal surgeon often plans a reconstruction at the same time. The osteocutaneous fibular free flap provides vascularized bone that can support reconstructive plating, as well as vascularized skin that can be used to separate the pharynx from the vertebral column if the mucosa and fascia are in poor condition. It is rare in hardware exposure and osteomyelitis cases that the mucosa is in good condition so the fibular skin paddle can be handy to seal the pharynx from the spinal defect. Communication with the spinal surgeon is key to assessing exactly what the needs are for each patient. ♦ The patient should have a tracheostomy in place, as flap swelling postoperatively is unpredictable. ♦ Obtain a CT angiogram or an MRA to assess the vasculature for three-vessel run-off to the foot. This aids in the selection of the safe leg to use or in deciding if this flap should be abandoned. This flap should be aborted if a congenital anomaly exists or if peripheral vascular disease has compromised the anterior tibial or posterior tibial arteries. ♦ Assess the pharyngeal defect and map out an appropriate skin paddle with the Doppler. ♦ Perform a neck exploration for vessels prior to harvesting the flap. We prefer the facial, superior thyroid, or transverse cervical artery for this flap. ♦ After harvest, discuss and measure the required bone for reconstruction. Perform a subperiosteal dissection to lengthen the pedicle and acquire the appropriate bone length. Trim as necessary. ♦ With the assistance of the spinal surgeon, place the bone in the needed location and affix it. Perform the microvascular anastomosis prior to securing the skin paddle. Ensure that there are no geometry issues. ♦ If the spine reconstruction is high (C1-3), we prefer to have the pedicle exit inferiorly with the distal part of the bone and skin paddle superior. This helps prevent kinking of the pedicle. If the reconstruction is lower, orient it either way and assess the best geometry to prevent compromise of the vasculature. The radial forearm fasciocutaneous free flap is a versatile reconstructive tool for large posterior pharyngeal wall defects. It is thin and pliable and can be used to reconstruct multiple compartments if needed. It can also reach higher than most pedicled flaps. We prefer to use this flap in superior pharyngeal defects due to the long pedicle and versatile design. The regional flaps are bulkier and difficult to extend this high. ♦ The forearm can be harvested from either arm if the Allen’s test is appropriate bilaterally. We tend to choose the nondominant arm. ♦ Once the defect is defined, a template of the defect should be made. This assists with aligning the vessels appropriately, ensuring good geometry, and capturing the cephalic vein. The template is transposed to the forearm, and the flap is planned and harvested in standard fashion. This is particularly useful if different compartments need to be reconstructed. ♦ Following the harvest, the flap is transferred into the defect and sutured with interrupted 3.0 Vicryl suture to form a watertight seal. Following reconstruction of the pharynx, we place a nasogastric feeding tube if a gastrostomy tube is not already present. We allow a minimum of 5 to 7 days prior to initiation of oral feeding under the care and guidance of a speech pathologist. Once the patient reaches adequate oral intake to maintain nutrition and there is no evidence of a leak, we pull the nasogastric tube. The soft palate defect is one of the most challenging defects to reconstruct. The mobility and function of the soft palate is complex, and alteration of this function can lead to velopharyngeal insufficiency (VPI) and dysphagia. Traditionally, a palatal prosthesis was used for many defects, but with the expansion of reconstructive options, these are reserved for small defects (central and less than one fourth) of the palate). A palatal prosthesis is also an option in patients who are too ill for reconstruction or refuse the surgery. Hemipalate defects are poor candidates for palatal obturation. The key aspect of soft palate reconstruction is to seal the nasopharynx from the reflux of air and food during speech and deglutition, respectively. Additionally, the reconstruction should allow airflow in both directions that is balanced so that speech is neither hyper- or hyponasal. Lateral defects of up to one third of the palate can be closed primarily or with a palatal island flap. Defects greater than one third of the palate are best served with a radial forearm free flap. We reserve obturation for patients who fail reconstruction, are too ill to undergo lengthy surgery, or refuse the reconstructive effort. A good prosthodontist is critical to the successful outcome of properly chosen soft palate defects. Palatal obturators are best suited when the defects are small (less than one fourth of the soft palate), central, and do not involve the free edge. This allows for continued function of the lateral pharyngeal walls and remnant soft palate. The patient should have adequate dentition or implants to support the prosthesis and forces that will occur. Some individuals do not tolerate these devices due to an overactive gag reflex.
Pharynx, Cervical Esophagus, and Hypopharynx Reconstruction
♦ RELEVANT FUNCTIONAL ANATOMY
♦ FUNCTIONAL REHABILITATION
♦ CLASSIFICATION OF DEFECTS
♦ THE LATERAL PHARYNGEAL DEFECT
Option for Management: Primary Closure
Option for Management: Regional Flaps
Surgical Technique and Considerations
Patient Selection and Perioperative Management
Option for Management: Radial Forearm Fasciocutaneous Free Flap (RFFF)
Surgical Technique and Considerations (Fig. 5.5 and Fig. 5.6)
Option for Management: Lateral Arm Free Flap
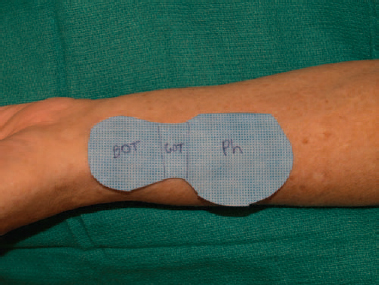
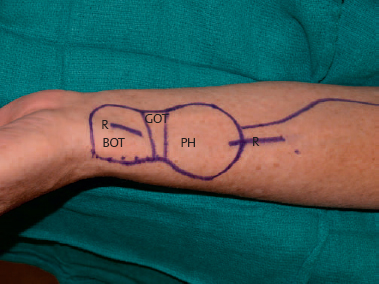
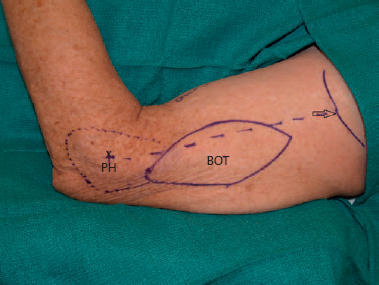
Surgical Technique and Considerations (Fig. 5.7)
Option for Composite Mandibular and Pharynx Defects: Fibular Free Flap
Surgical Technique and Considerations
Patient Selection and Perioperative Management
♦ THE POSTERIOR PHARYNGEAL DEFECT
Option for Management: Primary Closure
Option for Management: Skin Graft or Healing by Secondary Intention
Surgical Technique and Considerations
Option for Spine Plus Pharynx Reconstruction: Fibular Free Flap
Surgical Technique and Considerations
Option for Pharynx Only: Radial Forearm Free Flap
Surgical Technique and Considerations
Patient Selection and Perioperative Management
♦ THE SOFT PALATE DEFECT
Option for Management: Obturation
Option for Management: Palatal Remnant Adhesion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree